Abstract
Objective
To report various anatomic locations and clinical characteristics of pathologically proven myofibroblastoma in Koran patients.
Methods
Pathologic reports of patients who underwent surgeries at two centers between April 2003 and March 2016 were retrieved from the electronic medical record system of the hospital. Pathologic reports were included after performing a search using the keyword “myofibroblastoma”.
Results
The cohort consisted of 11 subjects and included eight female and three male individuals. The patients' ages ranged from 9 to 66 years. Tumors were located in the vagina in three patients and presented in the breast in seven patients. One case presented with an abdominal mass. The tumors ranged in mean size from 4.0 to 53.0 mm. Despite a relatively long-term follow-up, no case had evidence of tumor recurrence.
Conclusion
We evaluated the various anatomic locations of pathologically proven myofibroblastoma in Korean patients. As an extremely rare tumor, physicians should pay special attention to differential diagnosis. Surgical resection is the preferred method for a cure, and the recurrence rate is extremely low.
Myofibroblastoma is a very rare benign mesenchymal tumor composed of spindle tumor cells with myofibroblastic-like differentiation. Mammary myofibroblastoma was initially reported to occur in the breast in 1987 [1]. After that, superficial myofibroblastoma of the lower female genital tract was initially described in 2001 [2]. Due to the rarity of the tumor, only a few case reports or case series have been reported [345]. Recently, the wider anatomic distribution of myofibroblastoma was reported [6] and is now increasingly recognized. It appears as though the vulvovaginal or inguinal region may be at least as common sites as the breast for these tumors.
Physicians should pay close attention to differential diagnosis from other soft tissue tumors. However, the precise etiology still remains unclear due to the rarity of the condition. Furthermore, although the etiology may vary by race and region, there has been no study with clinicopathologic information reported in Korean women. Herein, along with the rarity of these cases, we report the various anatomic locations and clinical characteristics of pathologically proven myofibroblastoma in 11 patients presenting at two centers.
This study was approved by the institutional review board at the Seoul National University Bundang Hospital and Seoul National University Hospital. Pathologic reports of patients who underwent surgery at these two centers between June 2003 and March 2016 were retrieved from the electronic medical record system of the hospital. Pathologic reports were included after performing a search using the keywords “myofibroblastoma”.
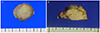
In our two hospitals, tissue samples were obtained from excisional specimens and pathologic diagnosis was confirmed as previously described in published reports [37]. Myofibroblastoma has been diagnosed and differentiated from other stromal tumors, both by morphology and immunohistochemistry. Grossly, the tumors were generally described as well circumscribed with a variably fatty appearance and the color is white-to-gray (Fig. 1). Histologically, the tumors generally comprised bundles of spindle shaped cells, which are arranged in interlaced or swirled patterns. Immunohistochemical staining with smooth muscle actin, desmin, CD34, vimentin, S-100, factor VIII, c-kit, cytokeratin and Ki 67 was used for differential diagnosis (Fig. 2).
The anatomic distribution of myofibroblastoma was investigated using the operative records and pathologic reports. Clinicopathologic variables including patient age, presenting symptom, size of tumor, and the status of the patient at last follow-up were analyzed.
The cohort consisted of 11 subjects and included eight female and three male individuals. Seven cases were from Seoul National University Hospital and six cases were from Seoul National University Bundang Hospital. All but one of the patients complained of a palpable, freely mobile and nontender mass. Immunohistochemical staining was used for differential diagnosis in seven cases.
Tables 1 and 2 show the clinicopathologic details of the patients with myofibroblastoma. The mean age at the time of diagnosis was 43.7 years, with a very wide range (median, 44 years; range, 9 to 66 years), but an overall predominance between the fifth and seventh decades. The mean size was 23.0 mm (median, 23.0 mm; range, 4.0 to 53.0 mm). No cases were documented to have positive resection margins.
Tumors were located in the vagina in three patients. Tumors were located in the breast in five women and two men. In all patients, there were no symptoms suggestive of breast cancer including nipple discharge, skin retraction or axillary node enlargement.
Intra-abdominal myofibroblastoma, which is extremely rare, was found in a 9-year-old boy. This child experiended intermittent abdominal discomfort. An approximately 5-cm mass with heterogenous enhancement, focal calcification and necrosis was observed on a computed tomography scan. The mass was excised en bloc including a part of omentum and peritoneum. The specimen was 6.5×5×4.5 cm in diameter. Myofibroblastoma was pathologically confirmed. There was no recurrence after excision at the 8-month follow-up visit. The mean follow-up time was 28.0 months (median, 28.0 months; range, 1 to 104 months). No case had evidence of tumor recurrence during this relatively long-term follow-up.
Myofibroblastoma is a recently discovered disease and is now increasingly recognized. In our two hospitals, a total of 11 cases were reported during 13 years. As a highly rare tumor, physicians should pay more attention to differential diagnosis to avoid excessive and radical treatment. The differential diagnosis of myofibroblastoma includes the following: spindle cell lipoma, fibromatosis, nodular and proliferative fasciitis, myoepithelioma and peripheral nerve sheath tumors. The differential diagnosis can be broad and somewhat dependent upon the anatomic location. It is also important to consider malignant tumors such as spindle cell carcinoma, leiomyosarcoma, infiltrating ductal carcinoma, metastatic malignant melanoma, apocrine carcinoma, stromal sarcoma and malignant fibrous histiocytoma in the differential diagnosis.
The mean age at time of diagnosis and a wide range are consistent with previous reports [246]. However, in the present study, the predominance was in the slightly younger (between the fifth and seventh decades in our study compared with the sixth and seventh decades in other studies).
In our series, anatomic locations included the vagina (27.3%) and breast (63.6%). The most recent comprehensive analysis of the clinicopathologic characterization of myofibroblastoma examined 143 cases [6]. In that study, the most common site was the groin or inguinal region (45%), including vulvar, perineal, and scrotal locations. The second most common site was the lower extremities (13%). The proportion of breast tumor was relatively lower (10%) than that of our study. However, the previous study has a critical limitation. Because all of the cases in that study were reviewed in consultation, the anatomic distribution reported may have been affected by referral bias. Furthermore, detailed clinical information was received from the referring physicians in only small portions (38%) of cases.
Ganesan et al. [4] analyzed the results of 12 patients with histologically proven myofibroblastoma of the lower female genital tract. In that study, myofibroblastoma occurred more frequently in the vagina (10 patients) than the vulva (two patients). Similarly, in our study, there was no case occurred in the vulva, while tumors were located in the vagina in three patients.
Among extramammary myofibroblastomas, intra-abdominal myofibroblastoma is especially rare. Howitt and Fletcher [6] has reported that 14 (9.7%) out of 143 tumors were intra-abdominal, retroperitoneal, or visceral in location.
A previous study reported cases of tumor recurrence; however, the recurrence rate was only 1.4% [6]. Based on previously published data and supported by our series, it can be concluded that the risk of recurrence is extremely low. No case had a recurrence on follow-up in the present study. Because of the benign nature of these lesions, some patients had relatively short follow-up.
Our results suggest that the predominance of age distribution was in the relatively younger than previous studies. The anatomic distribution was also different from previous studies. However, it is difficult to achieve a solid conclusion due to the small number of patients. Further studies with larger numbers and long-term follow-up periods are needed.
In summary, we report a case series of myofibroblastoma involving the lower genital tract, breast and abdomen. Along with the rarity of this tumor, we also discussed its characteristic features and histopathological findings. To the best of our knowledge, this is the first study to report clinicopathologic information of myofibroblastoma in Korean patients.
Figures and Tables
Fig. 2
Positivity for immunohistochemical staining (×400). (A) Smooth muscle actin, (B) CD34, and (C) desmin.
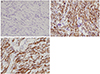
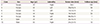
Table 1
Clinicopathologic details of the patients with myofibroblastoma of the vagin or inguinal region
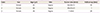
| Case | Sex | Age (yr) | Site | Tumor size (mm) | Follow-up (mo) |
|---|---|---|---|---|---|
| 1 | Female | 62 | Vagina | 50×30×15 | 39 |
| 2 | Female | 66 | Vagina | 30×25×23 | 1 |
| 3 | Female | 46 | Vagina | 11×9×6 | 29 |
Table 2
Clinicopathologic details of the patients with myofibroblastoma of the breast
Acknowledgments
The authors are indebted to J. Patrick Barron, Professor Emeritus, Tokyo Medical University and Adjunct Professor, Seoul National University Bundang Hospital for his editing of this manuscript.
References
1. Wargotz ES, Weiss SW, Norris HJ. Myofibroblastoma of the breast: sixteen cases of a distinctive benign mesenchymal tumor. Am J Surg Pathol. 1987; 11:493–502.
2. Laskin WB, Fetsch JF, Tavassoli FA. Superficial cervicovaginal myofibroblastoma: fourteen cases of a distinctive mesenchymal tumor arising from the specialized subepithelial stroma of the lower female genital tract. Hum Pathol. 2001; 32:715–725.
3. Gocht A, Bosmuller HC, Bassler R, Tavassoli FA, Moinfar F, Katenkamp D, et al. Breast tumors with myofibroblastic differentiation: clinico-pathological observations in myofibroblastoma and myofibrosarcoma. Pathol Res Pract. 1999; 195:1–10.
4. Ganesan R, McCluggage WG, Hirschowitz L, Rollason TP. Superficial myofibroblastoma of the lower female genital tract: report of a series including tumours with a vulval location. Histopathology. 2005; 46:137–143.
5. Chami R, Ertresvaag K, Azzie G, Thorner PS. Myofibroblastoma: report of a rare entity in the pediatric population. Pediatr Dev Pathol. 2012; 15:499–506.
6. Howitt BE, Fletcher CD. Mammary-type myofibroblastoma: clinicopathologic characterization in a series of 143 cases. Am J Surg Pathol. 2016; 40:361–367.
7. Pan J, Wang S, Zhang Y, Fan Z. Mammary myofibroblastoma in the right lateral abdominal wall. World J Surg Oncol. 2016; 14:55.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download