Abstract
Angioleiomyoma (AL) is a very rare benign tumor that originates from smooth muscle cells and has thick walled vessels. It may be found throughout the body but more frequently occurs in the lower extremities and rarely develops in the head and other parts of the body. This paper presents a case report of giant AL detected in a 33-year-old woman who complained of severe anemia, menorrhagia, and palpable lower abdominal mass. The patient underwent myomectomy and was diagnosed with AL based on the pathological report of mass. The effective treatment for AL is either simple hysterectomy or angiomyomectomy depending on the patient's desire to preserve fertility and symptom.
Angioleiomyoma (AL), a very rare benign tumor, originates from smooth muscle cells and contains thick walled vessels [1]. AL may be found throughout the body but more frequently occurs in the lower extremities and rarely develops in the head and other parts of the body. This type of tumor presents as a painful palpable nodule in subcutaneous tissues [2]. AL of the uterus is an extremely rare variant with only fifteen case reports available in literature, and most commonly occurs in the middle-aged women [3]. In this study, we report a case report of giant AL detected in a 33-year-old woman with complains of severe anemia, menorrhagia, and palpable lower abdominal mass.
A 33-year-old unmarried woman was admitted to the emergency room with symptoms of vaginal bleeding, headache, vertigo, and vomiting. The laboratory findings revealed a hemoglobin (Hb) level of 7.0 g/dL. The transabdominal ultrasound sonography and abdominal computed tomography showed a huge leiomyoma measured at 14.2 cm in the longest length (Fig. 1A and 1B). She was discharged after being transfused with 2 pints of packed red blood cell and visited to the outpatient clinic 2 days later with major complaints of menorrhagia and dysmenorrhea. In addition, she complained of a sensation of falling due to dizziness and discomfort from progressive compression caused by an abdominal mass palpable over long periods. The patient was prescribed with ulipristal acetate at a single dose of 5 mg for 12 weeks for the management of leiomyoma. In addition, iron supplementation was administered intravenously and then given orally for 3 months. At a follow-up visit 12 weeks later, the size of leiomyoma reduced to 9.8 cm in the longest length. She received myomectomy. The uterine artery was ligated after opening the abdominal cavity, and the largest leiomyoma was removed at a lower blood flow. The removed mass was measured 12.5×9.0×6.0 cm3 and weighed 475 g (Fig. 1C). The pathologic biopsy report of the mass revealed AL, and no nuclear atypism or mitosis and immunohistochemistry manifested the positivity of the stromal cells for desmin, positivity for smooth muscle actin (SMA) in the vessels, and negative reaction for CD10 (Fig. 2). The desmin and SMA represent smooth muscle tumor, and CD10 represents endometrial stromal tumor. The pathology report showed a smooth muscle tumor with many blood vessels. She is currently under outpatient observation.
Leiomyoma of the uterus is one of the very common benign tumors, which frequently occurs in women of reproductive age. There are different variants of leiomyoma viz. cellular, epithelioid, myxoid, lipoleiomyoma, etc., and amongst these variants AL is extremely rare, as till date only 15 cases of AL of the uterine corpus have been described in the literature [2]. Uterine AL usually occurs in the middle-aged females [3]. The patient in this case report was a 33-year-old unmarried woman.
Histologically, AL can be classified into 3 subtypes: capillary or solid, cavernous, and venous [2]. This type of fibroids usually arises in the myometrium, with size varying in the range 0.2–4.3 cm [2]. They differ from other types of leiomyoma in that they are encapsulated, multi-loculated and contain numerous vessels [4]. The diagnosis of AL is dependent on the histological findings, and AL is nearly impossible to distinguish clinically. Patients with uterine AL typically complain of severe dysmenorrhea, abdominal pain or discomfort, anemia accompanied by uterine bleeding and/or palpable abdominal mass. Handler et al. [5] described a case of consumptive coagulopathy secondary to a large degenerated AL.
Although the patient of this case report had no consumptive coagulopathy, she had a low Hb level at 7.0 g/dL with symptoms of severe vertigo and vomiting. Most patients complained of menorrhagia, which appeared to be caused by an increase in vascular structures resulting from dysregulation of angiogenesis of AL. The patient did not complain of abdominal pain, but one of the most common symptoms of AL is abdominal pain. The AL diagnosis usually manifests as a multi-lobulated mass with solid and laminated configuration with cystic or multi-septal contents in radiology images [6]. In this case report, it appeared as a single, unilocular uterine mass like typical leiomyoma. For this reason, the radiologic diagnosis of this mass was almost impossible. The preoperative diagnosis of AL is extremely difficult or even impossible, and can be diagnosed after surgical procedure and histological assessment by involving immunohistochemical staining. AL is a benign tumor. Several studies have asserted that this tumor has to be categorized as a benign leiomyoma variant and included in the World Health Organization classification of tumors of the female genital tract [3]. Despite benign nature, in cases of severe and repetitive symptoms, complete excision of the tumor and its capsule or margin-free tumor resection needs to be performed through a surgical intervention. Therefore, complete surgical removal is the treatment of choice, and either angiomyomectomy or simple hysterectomy has been proven to be effective; and the decision depends on the patient's symptoms and her desire to preserve fertility [4]. Eventually, hysterectomy is another treatment option to consider. Most of patients reported a particular postoperative course with clinical improvement in the symptoms. No recurrence was reported in any case [7]. Thus, if completely excised, these tumors have an excellent prognosis. More studies are warranted to further investigate angiomyomectomy and hysterectomy for better treatment modality and prognosis [8]. In cases where fertility should be preserved, complete angiomyomectomy including margin free and whole capsule removal should be performed. However, simple hysterectomy should be performed if the symptoms are severe and persist, or it seems impossible to be differentiated from malignant gynecologic tumor. In myomectomy, only leiomyoma is often removed except capsule; however, in AL leiomyoma and capsule should be completely removed, because of the increased possibility of re-bleeding.
Uterine AL is a distinctive variant of uterine smooth muscle neoplasm exhibiting characteristic morphology and immunohistochemistry features but same symptom [2]. AL has no particular imaging findings to differentiate it from other smooth muscle neoplasm. In addition, uterine AL has preoperative differential diagnosis, which is extremely difficult from other tumors. However, in the case of AL, more amount of vaginal bleeding may occur, caused by leiomyoma depending on the location, but if too much bleeding with severe anemia and that being that there are many blood vessels in leiomyoma during operation. Therefore, it is important for the clinicians and pathologists to recognize this rare benign entity and differentiate it from similar characteristics including malignant neoplasms.
Figures and Tables
Fig. 1
(A) Computed tomography shows 14.2 cm huge uterine myoma with endometrial compression, (B) transabdominal ultrasound sonography shows huge myoma found anterior to the uterus, and (C) gross findings show a 12.5×9.0 cm2 sized gray firm mass after the operation. UT, uterus.
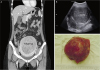
Fig. 2
(A) Microscopic findings indicate the tumor with interlacing short spindle cells and numerous thick walled vessels (hematoxylin and eosin stain, ×40), (B) immunohistochemical stain of smooth muscle actin (SMA) reveals diffuse positivity in the spindle tumor cells and swirling cells around the thick-walled blood vessels (immunohistochemistry of SMA, ×100).

References
1. Sharma C, Sharma M, Chander B, Soni A, Soni PK. Angioleiomyoma uterus in an adolescent girl: a highly unusual presentation. J Pediatr Adolesc Gynecol. 2014; 27:e69–e71.
2. Hachisuga T, Hashimoto H, Enjoji M. Angioleiomyoma. A clinicopathologic reappraisal of 562 cases. Cancer. 1984; 54:126–130.
3. Garg G, Mohanty SK. Uterine angioleiomyoma: a rare variant of uterine leiomyoma. Arch Pathol Lab Med. 2014; 138:1115–1118.
4. Zizi-Sermpetzoglou A, Myoteri D, Arkoumani E, Koulia K, Tsavari A, Alamanou E, et al. Angioleiomyoma of the uterus: report of a distinctive benign leiomyoma variant. Eur J Gynaecol Oncol. 2015; 36:210–212.
5. Handler M, Rezai F, Fless KG, Litinski M, Yodice PC. Uterine angioleiomyoma complicated by consumptive coagulopathy. Gynecol Oncol Case Rep. 2012; 2:89–91.
6. Hsieh CH, Lui CC, Huang SC, Ou YC, ChangChien CC, Lan KC, et al. Multiple uterine angioleiomyomas in a woman presenting with severe menorrhagia. Gynecol Oncol. 2003; 90:348–352.
7. Keerthi R, Nanjappa M, Deora SS, Kumaraswamy SV. Angioleiomyoma of cheek: report of two cases. J Maxillofac Oral Surg. 2009; 8:298–300.
8. Ishikawa S, Fuyama S, Kobayashi T, Taira Y, Sugano A, Iino M. Angioleiomyoma of the tongue: a case report and review of the literature. Odontology. 2016; 104:119–122.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download