This article has been
cited by other articles in ScienceCentral.
Abstract
Objective
To evaluate the predictive factors associated with the success of medical abortion by misoprostol monotherapy within 24 hours in the first trimester of pregnancy.
Methods
The records of 228 women with miscarriage up to 11 weeks of gestational age who underwent medical abortion by intravaginal misoprostol monotherapy were reviewed. Success of abortion was defined as complete expulsion of the conceptus without the need for surgical intervention. Outcomes of interest were success of abortion within 24 hours following administration of misoprostol.
Results
Among 222 women who continued the process of medical abortion for 24 hours, 209 (94.1%) had a successfully completed abortion. Multivariate logistic regression showed that serum β-human chorionic gonadotropin (β-hCG) above 40,000 mIU/mL is significantly associated with failed medical abortion within 24 hours (odds ratio [OR], 7.13; 95% confidence interval [CI], 1.60–37.32; P=0.011). The area under the receiver operating characteristic curve of β-hCG level associated with successful abortion within 24 hours was 0.705 (95% CI, 0.63–0.77; P=0.007). Previous vaginal delivery seems to be significantly associated with successful abortion within 24 hours on univariate analysis (P=0.037), but the association was lost in multivariate analysis.
Conclusion
Misoprostol monotherapy has a high success rate for first trimester abortion. Women with serum β-hCG less than 40,000 mIU/mL are likely to achieve a successful abortion within 24 hours after intravaginal administration of misoprostol.
Go to :

Keywords: Chorionic gonadotropin, Beta subunit, human, Medical abortion, Abortion, Pregnancy trimester, first
Introduction
Surgical curettage has been performed for abortion care in early pregnancy since the 1960s. Medical methods of abortion have more recently been developed and are now an established alternative method of first trimester pregnancy termination. Among researched drugs for medical abortion, mifepristone combined with misoprostol is known as the most effective regimen with approximately 90% success rate, and this regimen is used most commonly in the United States and Western Europe [
123]. Misoprostol monotherapy appears less effective than mifepristone plus misoprostol, but has a relatively high success rate of the 84% to 85% [
45]. In parts of the world where mifepristone remains unavailable including Korea, misoprostol-only regimens have become the method of choice [
3]. Therefore, further research including on the efficacy, side effects, and factors affecting outcomes are needed for misoprostol-only regimens.
Of various methods of misoprostol monotherapy for first trimester abortion, a commonly used regimen includes 800 µg vaginally every 12 hours for a maximum of 3 doses or 800 µg sublingually every 3 hours for maximum of 3 doses [
6]. With this method, the expulsion of conception products may occur 1to 2 weeks later. Compared with surgical abortion, medical abortion takes longer to complete, requiring days to weeks. Women may suffer vaginal bleeding or abdominal pain at home during the waiting time. These drawbacks can affect a women's preference for method of abortion. If we could understand the predictive factors for abortion success by the medical method, it would be a great help for decision-making. However, few studies have examined the factors affecting time of expulsion.
The purpose of this study was to investigate the predictive factors associated with success of medical abortion within 24 hours with misoprostol monotherapy in the first trimester of pregnancy. We present our experience with a misoprostol-only regimen, including efficacy, side effects, and acceptability.
Go to :

Materials and methods
This retrospective hospital-based cohort study included all women who were diagnosed with miscarriage at the first stage of pregnancy and underwent pregnancy termination with the medical method at a university hospital between 2011 and 2015. This study was approved by the Institutional Review Board of The Catholic University of Korea. After chart review, 228 women up to 11 weeks by gestational age based on the crown-rump length (CRL) and who underwent intravaginal misoprostol monotherapy for medical abortion were enrolled. All women were confirmed to have intrauterine pregnancy by transvaginal ultrasonography. Women who suffered heavy vaginal bleeding and abdominal cramping pain before administration of misoprostol were not included. Twin pregnancies (n=7) were included.
Per protocol, after counseling about surgical and medical abortion, patients seeking medical abortion were administrated an 800 µg-dose of misoprostol (Cytotec®; Pfizer, Seoul, Korea) moistened with 2 to 3 drops of normal saline into the posterior vaginal fornix. If the products of conception had not been passaged within 12 hours, a speculum examination was performed, and any conceptus in the vagina or cervical os was removed. Ultrasound assessment was performed to check the presence of gestational sac (GS) in the uterine cavity. A repeat 800 µg-dose of misoprostol was then given intravaginally. If abortion had not occurred within the next 12 hours, following discussion of failure rate and risks, the third dose of misoprostol was given. If patients changed their mind on treatment method during the process, surgical curettage was performed immediately.
Success of abortion was defined as complete expulsion of the conceptus without the need for surgical intervention following administration of misoprostol. Abortion was confirmed by identification products of conception or by empty uterine cavity observed by transvaginal ultrasonography. Ongoing pregnancy or partial passage of products of conception was defined as failed abortion, and surgical curettage was performed. The time of expulsion was defined as the time interval from administration of misoprostol to passage of products of conception.
Baseline data included maternal age, menstrual age, previous vaginal delivery, previous cesarean delivery, and previous abortion. Dose of misoprostol administrated, the time of expulsion, failure or success of abortion, time of curettage in case of failed abortion, and side effects of misoprostol were reviewed from the chart. In addition, sonographic findings including mean GS diameter, CRL, the presence of fetal pole, and presence of uterine myoma or adenomyosis and β-human chorionic gonadotropin (β-hCG) were reviewed. Blighted ovum that had no fetal pole was considered 0 mm of CRL.
Outcomes of interest were defined as success of abortion within 24 hours following administration of misoprostol. All maternal and embryonic characteristics were summarized according to the outcome of abortion using descriptive statistics: mean (±standard deviation) or median (Q1–Q3) for continuous variables and frequency (percent) for categorical variables. Student's t-test or Mann-Whitney U-test was utilized for comparison between success and failure groups in continuous variables according to the normality of data. The χ2 test or Fisher's exact test was utilized for comparison between 2 groups in categorical variables. The screening performance of the significant continuous variables was determined by the receiver operating characteristic (ROC) curve. Multiple logistic regression analysis was carried out to determine the performance of significant dependent variables in predicting success of abortion within 24 hours. A P-value less than 0.05 indicated statistical significance. SPSS (version 12.0; SPSS Inc., Chicago, IL, USA) was used for statistical analysis.
Go to :

Results
Of the cohort of 228 patients, 14 women underwent surgical curettage during the process of medical abortion. Eleven women changed their choice about treatment method due to long waiting time — 6 women in the 12 to 24 hours period and 5 women in the 24 to 36 hours period following administration of misoprostol. Three women underwent surgical curettage due to failure of medical abortion 36 hours later. Among women who continued the process of medical abortion until 12, 24, and 36 hours later, 135 among 228 (59.2%) women achieved successful abortion in 12 hours, 209 among 222 (94.1%) women in 24 hours, and 214 among 217 (98.6%) women in 36 hours.
The most common side effects were abdominal pain (62.8%) followed by fever for a few hours (35.1%). Mild diarrhea was also observed in 8 (3.5%) women and nausea in 7 (3.1%) women. Analgesics or antiemetic metoclopramide was given, and all side effects resolved after completion of abortion.
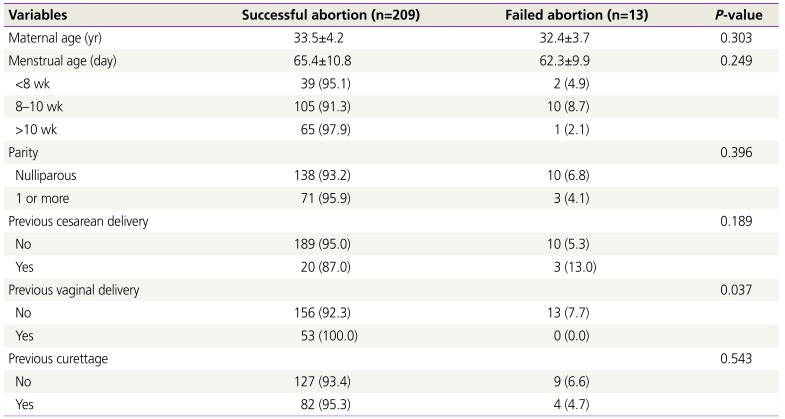
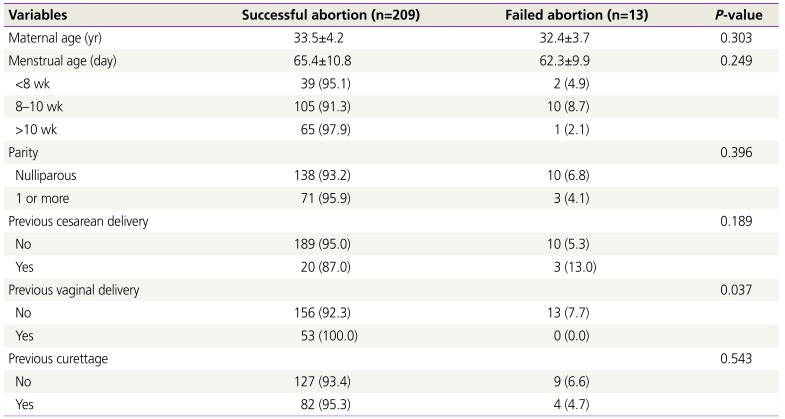
To evaluate the factors for successful medical abortion within 24 hours, we analyzed 222 women who continued the process until 24 hours following administration of misoprostol. The comparison of maternal characteristics between the successful abortion group and failed abortion group showed that history of vaginal delivery was significantly associated with successful abortion (
P=0.037) (
Table 1). None of the 53 women who had a history of vaginal delivery experienced a failed medical abortion within 24 hours. History of cesarean delivery and curettage was not associated with successful abortion within 24 hours. Menstrual age was not a significant factor associated with success of abortion within 24 hours.
Table 1
Baseline characteristics of women who had successful or failed medical abortion in 24 hours
|
Variables |
Successful abortion (n=209) |
Failed abortion (n=13) |
P-value |
|
Maternal age (yr) |
33.5±4.2 |
32.4±3.7 |
0.303 |
|
Menstrual age (day) |
65.4±10.8 |
62.3±9.9 |
0.249 |
|
<8 wk |
39 (95.1) |
2 (4.9) |
|
|
8–10 wk |
105 (91.3) |
10 (8.7) |
|
|
>10 wk |
65 (97.9) |
1 (2.1) |
|
|
Parity |
|
|
0.396 |
|
Nulliparous |
138 (93.2) |
10 (6.8) |
|
|
1 or more |
71 (95.9) |
3 (4.1) |
|
|
Previous cesarean delivery |
|
|
0.189 |
|
No |
189 (95.0) |
10 (5.3) |
|
|
Yes |
20 (87.0) |
3 (13.0) |
|
|
Previous vaginal delivery |
|
|
0.037 |
|
No |
156 (92.3) |
13 (7.7) |
|
|
Yes |
53 (100.0) |
0 (0.0) |
|
|
Previous curettage |
|
|
0.543 |
|
No |
127 (93.4) |
9 (6.6) |
|
|
Yes |
82 (95.3) |
4 (4.7) |
|

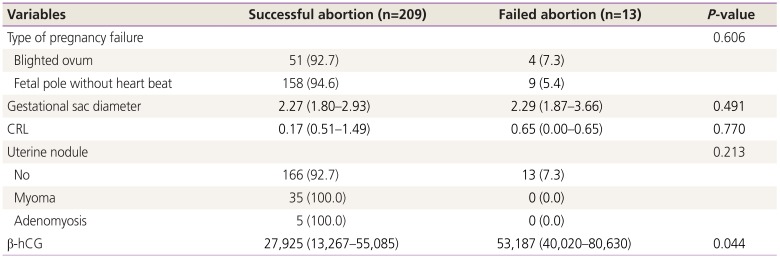
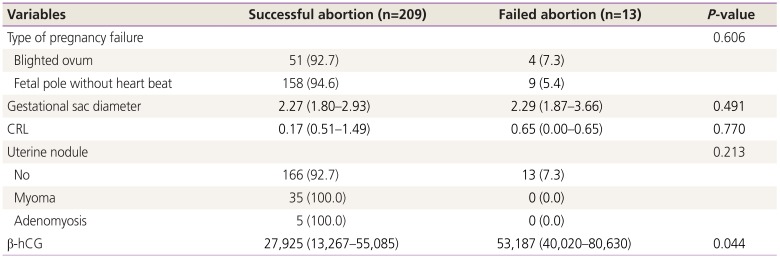
Table 2 shows the laboratory and ultrasonographic factors associated with success of abortion. Serum β-hCG level was a significant factor associated with success of abortion within 24 hours (
P=0.044). However, ultrasonographic factors were not associated with successful abortion. Presence of fetal pole, GS diameter, and CRL were not significant factors. Myoma or adenomyosis was not associated with failed medical abortion.
Table 2
Laboratory and ultrasonographic factors of women who had successful or failed medical abortion in 24 hours
|
Variables |
Successful abortion (n=209) |
Failed abortion (n=13) |
P-value |
|
Type of pregnancy failure |
|
|
0.606 |
|
Blighted ovum |
51 (92.7) |
4 (7.3) |
|
|
Fetal pole without heart beat |
158 (94.6) |
9 (5.4) |
|
|
Gestational sac diameter |
2.27 (1.80–2.93) |
2.29 (1.87–3.66) |
0.491 |
|
CRL |
0.17 (0.51–1.49) |
0.65 (0.00–0.65) |
0.770 |
|
Uterine nodule |
|
|
0.213 |
|
No |
166 (92.7) |
13 (7.3) |
|
|
Myoma |
35 (100.0) |
0 (0.0) |
|
|
Adenomyosis |
5 (100.0) |
0 (0.0) |
|
|
β-hCG |
27,925 (13,267–55,085) |
53,187 (40,020–80,630) |
0.044 |

The area under the ROC curve for factors associated with success of abortion was 0.705 (95% confidence interval [CI], 0.63–0.77; P=0.007) according to β-hCG level. A β-hCG concentration >40,000 mIU/mL had sensitivity of 81.8% (95% CI, 48.2–97.7) and specificity of 63.3% (95% CI, 55.6–70.6) for prediction of failed medical abortion within 24 hours following misoprostol administration.
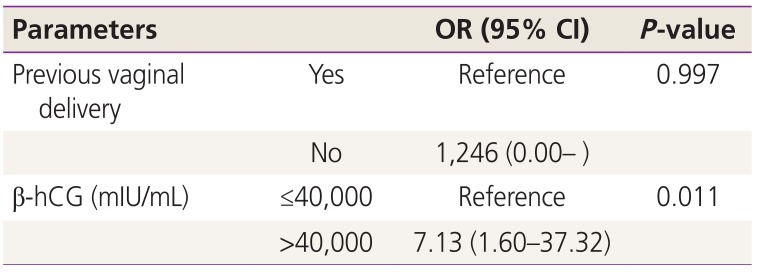
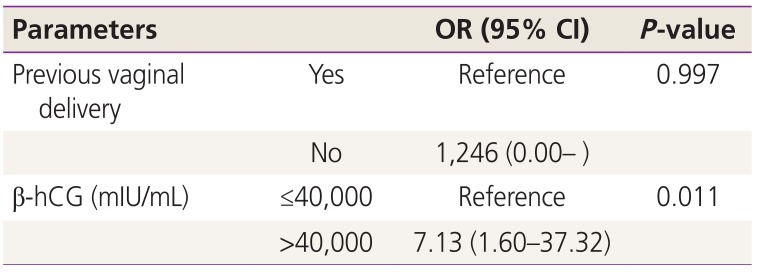
Multiple logistic regression analysis including previous vaginal delivery and β-hCG above 40,000 mIU/mL showed that β-hCG above 40,000 mIU/mL was a significant factor for failed medical abortion within 24 hours after adjusting for previous vaginal delivery (odds ratio [OR], 7.13; 95% CI, 1.60–37.32;
P=0.011) (
Table 3).
Table 3
Multivariate analysis of obstetric factors for failed medical abortion
|
Parameters |
|
OR (95% CI) |
P-value |
|
Previous vaginal delivery |
Yes |
Reference |
0.997 |
|
No |
1,246 (0.00– ) |
|
|
β-hCG (mIU/mL) |
≤40,000 |
Reference |
0.011 |
|
>40,000 |
7.13 (1.60–37.32) |
|

Go to :

Discussion
One dosing option of misoprostol monotherapy for medical abortion is the protocol of intravaginal 800 µg misoprostol every 12 hours for a maximum of 3 doses. The overall success rate of this protocol was 98.6% for pregnancy up to 11 weeks gestational age in this study. The success rate after ≤2 doses of misoprostol was 91.7%. In addition, this study showed that serum β-hCG below 40,000 mIU/mL increased the probability of abortion success within 24 hours with 2 doses of intravaginal misoprostol. Although there have been several studies on predictors associated with successful medical abortion, few studies have considered factors associated with short time of expulsion. Therefore, this finding that women with low β-hCG have a possibility of successful abortion within 24 hours with misoprostol is helpful data for the choice of abortion method.
Considering the high success rate of medical abortion in first trimester termination, medical abortion can be a treatment of choice instead of surgical abortion. However, many doctors and patients still prefer the surgical method. According to a previous report, post-abortion satisfaction is high in both surgical and medical methods among women who chose their method of abortion, but surgical abortion seems to be more acceptable in women who do not select the treatment method themselves [
78]. The biggest factor in women selecting medical abortion is the belief that they are safer, more natural, and private because they can avoid surgery compared to surgical abortion [
39]. However, fear of failure and fear of pain and vaginal bleeding during the treatment process are negative factors that cause hesitation in selection of medical abortion. The relatively long time of expulsion can affect women's choice of treatment. With longer time of expulsion, more emotional difficulties associated with the abortion can continue, and the patient can experience pain and bleeding. The longer is the time interval, the greater is the likelihood that patients will withdraw from the medical method, which makes them feel dissatisfied with the treatment. However, reports to date have no predictive factors for the time for expulsion, so that we cannot fully advise patients. This uncertainty leads many women experiencing miscarriage to choose surgical abortion. Therefore, if patients can be provided with the possibility of more rapidly timed expulsion by the medical method during counseling, it could be highly valuable for the patient to determine the abortion method.
In this study, we found that β-hCG lower than 40,000 mIU/mL may be a predictive factor of successful abortion within 24 hours after misoprostol administration. Usually, early gestational age is known to be related to the high success rate of medical abortion [
1011]. However, in this study, menstrual age was not significantly related to the success of the abortion treatment within the first 24 hours. Menstrual age is not the same as gestational age, but is an approximation. As gestational age is difficult to establish accurately in the case of first trimester miscarriage, menstrual age may have to be used in many clinical cases. Generally, CRL reflects gestational age relatively accurately at the first trimester of pregnancy. Therefore, the present study analyzed the effect of CRL on success rate of medical abortion, but there was no significant correlation. GS diameter was not related to the success rate of abortion treatment within 24 hours. Therefore, this study showed that serum β-hCG rather than gestational age may be significantly related to the success rate of abortion treatment within 24 hours.
Serum β-hCG concentration is a hormone secreted by the placenta, which increases as pregnancy progresses until 9 to 11 weeks of gestation but decreases in the event of a miscarriage. When drug administration for medical abortion is delayed due to late diagnosis of miscarriage, serum β-hCG is decreased compared to gestational age. In this case, serum β-hCG may be a more effective factor in predicting the success rate of abortion than gestational age. The role of serum β-hCG as a predictor of successful misoprostol management of early miscarriage has been reported by Schreiber et al. [
12]. In 49 early miscarriage patients with serum β-hCG level over 4,000 mIU/mL, a single-dose of misoprostol was more likely to be successful in abortion than cases with high level of β-hCG [
12]. In our study, when β-hCG level was less than 40,000 mIU/mL, successful abortion was likely to be completed after 1 or 2 doses of misoprostol. Regimens of medical abortion using misoprostol have been variously applied. In each regimen, future studies should be conducted to determine how β-hCG level relates to the success of abortion and the cut-off value at that time.
This study suggests that patients with previous vaginal delivery may be associated with success of rapid medical abortion by misoprostol within 24 hours. All 53 women with more than one vaginal delivery experienced significantly successful abortion within 24 hours compared with nulliparous women. Because this factor did not remain significant in multivariate analysis, more data needs to be analyzed in the future. Previous studies on the relationship between vaginal delivery and successful abortion showed results contradictory to those of this study. Chien et al. [
13] evaluated medical abortion by oral mifepristone combined with misoprostol; after 14 to 21 days, parous women were more at risk of failed medical abortion than nulliparous women. These results are the same as those of Bartley et al. [
14]. The response of the uterus to early pregnancy for mifepristone and misoprostol seems to be due to parity. Further studies are necessary to evaluate how the outcome of medical abortion varies with previous vaginal delivery.
In this study, the regimen of 800 µg intravaginal misoprostol every 12 hours, for a maximum of 3 doses, resulted in 98.6% successful termination of early miscarriage. However, 4.8% of women gave up the process in the middle of waiting and underwent surgical curettage. This change of mind may be caused by anxiety about side effects such as abdominal pain and fever and unpredictable time to expulsion [
310]. In this study, abdominal pain occurred in 62% and fever occurred in 35%. These complications resolved with the passage of conceptus without specific treatment but could be a factor in the acceptability of the misoprostol method. To increase the acceptability of abortion by misoprostol, prophylactic antipyretics and analgesics may be administered in advance. Above all, it is necessary to relieve the patient emotionally by informing her of the high success rate of medical abortion. Women with a high likelihood of successful abortion within 24 hours of drug administration may have high acceptability for the procedure. It is therefore advisable to evaluate these women beforehand and is helpful to conduct a serum β-hCG test.
This study confirmed that misoprostol monotherapy in the first trimester of pregnancy has a high success rate and may be a good alternative to surgical uterine curettage. In particular, when serum β-hCG is less than 40,000 mIU/mL, successful abortion has high likelihood within 24 hours. These results can be used as a good basis for future study of abortion methods in women experiencing miscarriage.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download