Abstract
Objective
To determine whether late preterm twin neonates have a more favorable perinatal outcome than singleton late preterm neonates.
Methods
We studied 401 late preterm births between 34+0 and 36+6 weeks of gestation, from January 2011 to December 2014 in our institution. We compared the maternal and neonatal characteristics and perinatal outcomes between singleton and twin pregnancies. Perinatal outcomes included Apgar score, admission to the neonatal intensive care unit (NICU) or special care nursery, duration of NICU stay, and the rate of composite morbidity (antibiotic use, hypoglycemia, hypocalcemia, hyperbilirubinemia requiring phototherapy, respiratory support, and respiratory distress syndrome).
Results
A total of 289 neonates were in the singleton group and 112 in the twin group. The twin group showed smaller mean birth weight despite of longer gestational age at delivery. In addition, there were significant differences in the indication of delivery and cesarean section rate between the 2 groups. Overall, the risk of composite morbidity was similar between 2 groups (odds ratio, 1.4; 95% confidence interval, 0.8 to 2.4).
Recently, the incidence of twin pregnancy increased from 2.2% in 2005 to 3.6% by 2015 and about 60% of them were delivered before 37 complete weeks of gestation in Korea [1]. In addition, the majority of twins are known to be delivered in late preterm period [2]. It is known that late preterm births are associated with poor perinatal outcomes including respiratory distress syndrome (RDS), apnea, transient tachypnea of the newborns (TTN), hypoglycemia, hypothermia, hyperbilirubinemia, and feeding difficulties compared to term births [3456]. However, about 20% of late preterm births in twin pregnancies did not have any definitive maternal or fetal indication for delivery [6]. This practice may be based on the clinical impression that twin fetuses have more rapid pulmonary maturation than singleton [7] and on several epidemiologic studies showing that the lowest perinatal mortality rate for twins occurs at an earlier gestational age, and preventing unexplained fetal death in twin pregnancies [891011].
Meanwhile, many studies on late preterm births have focused on only singleton pregnancies and those on twin pregnancies have focused on the optimal timing of delivery or compared perinatal outcomes to term twin pregnancies [1012131415]. Also, studies on comparison of perinatal outcome between twin and singleton have been about extremely premature neonates [16]. Moreover, there have been sparse studies comparing twin and singleton pregnancies in the late preterm period showing conflict conclusions [717]. Therefore, in this study we aimed to determine whether late preterm twin neonates have a more favorable perinatal outcome than singleton late preterm neonates.
This was a retrospective study of singleton and twin late preterm births from January 2011 to December 2014 in our institution. We identified patients and collected clinical information from electronic medical records. We included late preterm births who delivered between a gestational age between 34+0 and 36+6 weeks. We excluded multiple pregnancies beyond twin, major structural anomalies, chromosomal anomalies, and stillbirths. The gestational age was calculated from the first day of the last menstrual period or by fetal ultrasound in the 1st trimester.
The indication of delivery consisted of spontaneous and indicated late preterm birth. Spontaneous late preterm birth included preterm labor with intact membranes and preterm premature rupture of membranes (PPROM); indicated late preterm births included hypertensive disorders such as gestational hypertension, preeclampsia and superimposed preeclampsia, placental causes (placental abruption and placenta previa), fetal causes (intrauterine growth restriction, oligohydramnios, and fetal distress) and maternal medical disease including cardiopulmonary or rheumatic diseases. In addition, we categorized the late preterm births without definitive delivery indication into an elective group.
We assessed the baseline maternal and neonatal characteristics including age, gestational age at delivery (GAD), parity, mode of delivery and birth weight between 2 groups. Additionally, we reviewed Apgar score at 1 and 5 minutes after each birth, admission to neonatal intensive care unit (NICU) or special care nursery , duration of NICU stay, and the rate of composite morbidity. Criteria for NICU or special care nursery admission were as follows: gestational age of less than 35 weeks, birth weight of less than 2.3 kg, or a need for close observation by a neonatologist. Composite morbidity is defined as having more than one of the following: antibiotic use, hypoglycemia, hyperbilirubinemia requiring phototherapy, respiratory support, and RDS. The indications of antibiotic use were as follows: cases of PPROM, maternal fever, or suspicion of perinatal acquired infection. After confirmations of a negative culture test, antibiotics were stopped. Hypoglycemia was defined as plasma glucose less than 40 mg/dL and hypocalcemia as an ionized calcium concentration of less than 4 mg/dL. We defined respiratory support as use of a continuous positive airway pressure (CPAP) or medical ventilator. RDS was defined as the presence of diagnostic radiographic chest findings plus 1 or more clinical signs of respiratory distress including respiratory grunting, retracting, and increased oxygen requirement (a fraction of inspired oxygen >0.4), or administration of exogenous pulmonary surfactant.
Then, we compared the maternal characteristics and perinatal outcomes in singleton and twin neonates. This study used the Pearson χ2 test for categorical variables and Student's t-test for continuous variables. Multiple logistic regression analysis was performed in comparison of composite morbidity between 2 groups controlling for GAD, indication and mode of delivery. Statistical analysis was performed using SPSS software version 19.0 (SPSS Inc., Chicago, IL, USA). This study was approved by institutional review board (IRB) from Kyungpook National University Hospital and Kyungpook National University School of Medicine, Korea (IRB No. 2016-07-011).
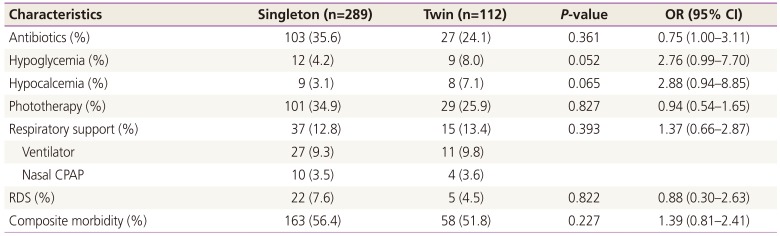
A total of 394 women with late preterm births were recorded during the study period (334 singleton, 60 multiple pregnancy pregnant women). Among them, 45 singletons and 4 multiple pregnancies were excluded based on the aforementioned criteria; 401 late preterm neonates (289 singletons and 112 twin neonates) were finally included. The comparison of maternal characteristics and pregnancy outcomes are shown in Table 1. The twin group showed a longer GAD and, there were significant differences in the delivery indications and the rate of cesarean delivery. The twin group had higher rate of elective late preterm births (0% vs. 16.1%, P<0.001) and cesarean section compared to the singleton group (57.8% vs. 91.1%, P<0.001). Most twin in our twin group (94.6%) were dichorionic. Neonatal outcomes are described in Table 2. Birth weight was significantly smaller in the twin group (2.40±0.40 vs. 2.29±0.38, P=0.018) despite a longer gestational age; however, there was no significant difference in Apgar score or NICU admission rate between 2 groups. Overall, there was no difference in composite morbidity between 2 groups in multiple logistic regression analysis (Table 3).
In this study, we reviewed 401 late preterm neonates to compare maternal characteristics and neonatal outcomes between singleton and twin pregnancies. Our results showed that there were differences in GAD, mean birth weight, the indication and mode of delivery between the 2 groups. However, the rate of composite morbidity was similar between the 2 groups.
Similar to previous studies, about two-thirds of our study group outcomes were related to spontaneous preterm births and one third related to indicated or elective preterm births [51819]. Importantly, 16.1% of late preterm twins had no definitive indication; however, there were no deliveries without indication in the singleton group. Since the beginning of this study on deliveries occurring after January 2011, concerns regarding late preterm births have emerged, and discretionary late preterm birth in singleton pregnancy was absent. Moreover, the rate of discretionary delivery in the twin group was lower than that in a previous report (22%, 716/3,252) [18]. Compared to twin pregnancies, singleton pregnancy showed higher rate of indicated late preterm birth and it would be associated with shorter GAD in singleton group.
Our twin group showed a significantly higher rate of cesarean delivery without differences in maternal age or parity compared to the singleton group. Other previous studies in Korea showed a roughly 90% to 98% rate of cesarean delivery in late preterm births [2021]. The mode of delivery in twin pregnancy is still controversial [101920]; however, cesarean section is preferred in our institution because of safety concerns. In neonatal characteristics, mean birth weight was smaller in twin groups similar to previous studies [717]. The growth of twins differed from that of singleton after 33 weeks of gestation [22] and twin fetuses were expected to be approximately 121 go lighter than singleton on average [23]. Meanwhile, our study group showed a higher rate of NICU admission compared to previous studies [1215]; because neonates who require for close observation by a neonatologist admitted to the NICU or special care nursery in our institution.
Since, our study group showed difference in GAD, indication and mode of delivery, we compared the rate of composite morbidity by using multiple logistic regression analysis controlling for these differences. A previous study did not show a difference in the rate of early or late onset neonatal sepsis between singleton and twin late preterm births [24]. Our results also showed that the rate of antibiotic use was also similar in 2 groups. It would be ideal to review the rate of neonatal sepsis rather than antibiotic use; however, the administration of antibiotics usually preceded culture test when neonates had clinical symptoms, such as tachypnea or respiratory difficulty. Peculiarly, the rate of ventilator use was higher than that of CPAP within each group. This phenomenon would be associated with the fact that cases using a ventilator even very shortly were also regarded as the ventilator group.
Although cesarean delivery may be associated with the risk of RDS or respiratory support [25], our twin group showed a similar rate in these morbidities despite a higher cesarean delivery rate. Simchen et al. [17] reported that there was no difference in the rate of RDS between singleton and twin late preterm infants but O2 administration >1 day was significantly higher in singleton pregnancy after controlling for mode of delivery, fetal gender and PPROM. And the authors suggested that this result would be associated with acceleration of lung maturation and higher rate of antenatal corticosteroid administration in twin group [17]. On the other hand, Ribicic et al. [7] reported there were no differences in the rate of TTN and RDS despite of higher rate of cesarean delivery in twin group. And they also suggested this result would be a higher rate of antenatal corticosteroid administration and of higher rate female gender in twin group. Our study showed there was no difference in the rate of RDS and respiratory support after controlling for mode of delivery that meant twin itself was neither a risk factor nor protective factor for RDS. Although antenatal corticosteroid is very important factor for respiratory outcomes, we could not investigate the rate of antenatal corticosteroid administration in our study group; because most of our study subjects were transferred from other clinics to our institution for managements of impending late preterm births. In also, oxygen supplementation or surfactant use may be more proper variables in studies about lat -preterm infants than RDS, endotracheal intubation or CPAP; however, most of neonates in who required endotracheal intubation were administered surfactant before definitive diagnosis of RDS. And, the exact period of O2 supplementation was not difficult to review through electronic medical record.
Several metabolic morbidities such as hypoglycemia, hypocalcemia, and hyperbilirubinemia are known to be increased in late preterm [26]. There was no difference in these morbidities between the singleton and twin groups; however, the rate of hypoglycemia and hypocalcemia tended to be lower in the twin groups compared to singleton group. We presumed this result would be associated with smaller birth weight in twin pregnancy. Hypoglycemia could be associated with gestational diabetes mellitus (GDM) and glucose intolerance rate are known to be higher in multiple gestation [27]. However, there were only 4 cases of GDM in our twin groups; therefore, we did not include GDM as variables. Previous studies showed the rate of hyperbilirubinemia requiring phototherapy was higher in the singleton group and the authors it would be related with higher rate of breastfeeding in singleton group [717]. We considered only neonatal outcomes (not infantile outcomes) and we presumed breastfeeding rate was similar in the first few weeks of life; therefore, the rate of phototherapy was similar between 2 groups in our study.
There are several limitations in our study. We could not evaluate important composite morbidities, such as bronchopulmonary dysplasia , necrotizing enterocolitis or intraventricular hemorrhage, and mortality rate due to the limitation of retrospective study and small sample size. In addition, most cases of twin pregnancy were dichorionic resulting in a poor reflection of the neonatal outcomes in monochorionic late preterm births in this study. However, the objective of the study was to compare the neonatal outcomes between singleton and twin pregnancies in late preterm birth; therefore, the consideration of chorionicity may not be beyond the scope in our study.
In conclusion, our findings suggest that the twin neonates are not mature faster compared to singleton neonates in late preterm period. Therefore, late preterm delivery in twin as well as singleton pregnancies should be considered carefully.
References
1. Korean Statistical Information Service. Future population estimation [Internet]. Daejeon (KR): Statistics Korea;2015. 2017.08.11.Available from: http://kosis.kr/ups/ups_01List.jsp?pubcode=PJ.
2. Martin JA, Kung HC, Mathews TJ, Hoyert DL, Strobino DM, Guyer B, et al. Annual summary of vital statistics: 2006. Pediatrics. 2008; 121:788–801. PMID: 18381544.

3. Loftin RW, Habli M, Snyder CC, Cormier CM, Lewis DF, Defranco EA. Late preterm birth. Rev Obstet Gynecol. 2010; 3:10–19. PMID: 20508778.
4. Newman RB, Unal ER. Multiple gestations: timing of indicated late preterm and early-term births in uncomplicated dichorionic, monochorionic, and monoamniotic twins. Semin Perinatol. 2011; 35:277–285. PMID: 21962627.

5. Tomashek KM, Shapiro-Mendoza CK, Davidoff MJ, Petrini JR. Differences in mortality between late preterm and term singleton infants in the United States, 1995–2002. J Pediatr. 2007; 151:450–456.e1. PMID: 17961684.
6. Brown HK, Speechley KN, Macnab J, Natale R, Campbell MK. Neonatal morbidity associated with late preterm and early term birth: the roles of gestational age and biological determinants of preterm birth. Int J Epidemiol. 2014; 43:802–814. PMID: 24374829.

7. Ribicic R, Kranjcec I, Borosak J, Tumbri J, Mihovilovic Prajz L, Ribicic T. Perinatal outcome of singleton versus twin late preterm infants: do twins mature faster than singletons? J Matern Fetal Neonatal Med. 2016; 29:1520–1524. PMID: 26103779.

8. Spong CY, Mercer BM, D'alton M, Kilpatrick S, Blackwell S, Saade G. Timing of indicated late preterm and early-term birth. Obstet Gynecol. 2011; 118:323–333. PMID: 21775849.
9. Jakiel G, Wilińska M, Bińkowska M, Kowal A, Rumowska S, Ciebiera M. Late preterm infants - impact of perinatal factors on neonatal results. A clinical study. Ann Agric Environ Med. 2015; 22:536–541. PMID: 26403130.
10. Tsai ML, Lien R, Chiang MC, Hsu JF, Fu RH, Chu SM, et al. Prevalence and morbidity of late preterm infants: current status in a medical center of Northern Taiwan. Pediatr Neonatol. 2012; 53:171–177. PMID: 22770105.

11. Davidoff MJ, Dias T, Damus K, Russell R, Bettegowda VR, Dolan S, et al. Changes in the gestational age distribution among U.S. singleton births: impact on rates of late preterm birth, 1992 to 2002. Semin Perinatol. 2006; 30:8–15. PMID: 16549207.

12. Büscher U, Horstkamp B, Wessel J, Chen FC, Dudenhausen JW. Frequency and significance of preterm delivery in twin pregnancies. Int J Gynaecol Obstet. 2000; 69:1–7. PMID: 10760526.

13. Elliott JP, Istwan NB, Collins A, Rhea D, Stanziano G. Indicated and non-indicated preterm delivery in twin gestations: impact on neonatal outcome and cost. J Perinatol. 2005; 25:4–7. PMID: 15496871.

14. Christopher D, Robinson BK, Peaceman AM. An evidence-based approach to determining route of delivery for twin gestations. Rev Obstet Gynecol. 2011; 4:109–116. PMID: 22229063.
15. Friedman SA, Schiff E, Kao L, Kuint J, Sibai BM. Do twins mature earlier than singletons? Results from a matched cohort study. Am J Obstet Gynecol. 1997; 176:1193–1196. discusstion 6-9. PMID: 9215173.

16. Shinwell ES, Haklai T, Eventov-Friedman S. Outcomes of multiplets. Neonatology. 2009; 95:6–14. PMID: 18832859.

17. Simchen MJ, Okrent Smolar AL, Dulitzky M, Sivan E, Morag I. Neonatal morbidities and need for intervention in twins and singletons born at 34–35 weeks of gestation. J Perinat Med. 2016; 44:887–892. PMID: 26677882.

18. Engle WA, Kominiarek MA. Late preterm infants, early term infants, and timing of elective deliveries. Clin Perinatol. 2008; 35:325–341. viPMID: 18456072.

19. Kilpatrick SJ, Jackson R, Croughan-Minihane MS. Perinatal mortality in twins and singletons matched for gestational age at delivery at > or = 30 weeks. Am J Obstet Gynecol. 1996; 174:66–71. PMID: 8572036.
20. Lee HJ, Kim SH, Chang KH, Sung JH, Choi SJ, Oh SY, et al. Gestational age at delivery and neonatal outcome in uncomplicated twin pregnancies: what is the optimal gestational age for delivery according to chorionicity? Obstet Gynecol Sci. 2016; 59:9–16. PMID: 26866030.

21. Lee JH, Jun JK. Management of twin delivery. Korean J Perinatol. 2007; 18:95–100.
22. Gielen M, Lindsey PJ, Derom C, Loos RJ, Souren NY, Paulussen AD, et al. Twin-specific intrauterine ‘growth’ charts based on cross-sectional birthweight data. Twin Res Hum Genet. 2008; 11:224–235. PMID: 18361725.

23. Odibo AO, Cahill AG, Goetzinger KR, Harper LM, Tuuli MG, Macones GA. Customized growth charts for twin gestations to optimize identification of small-for-gestational age fetuses at risk of intrauterine fetal death. Ultrasound Obstet Gynecol. 2013; 41:637–642. PMID: 23334992.

24. Ballabh P, Kumari J, AlKouatly HB, Yih M, Arevalo R, Rosenwaks Z, et al. Neonatal outcome of triplet versus twin and singleton pregnancies: a matched case control study. Eur J Obstet Gynecol Reprod Biol. 2003; 107:28–36. PMID: 12593890.

25. Feldman K, Woolcott C, O'Connell C, Jangaard K. Neonatal outcomes in spontaneous versus obstetrically indicated late preterm births in a nova scotia population. J Obstet Gynaecol Can. 2012; 34:1158–1166. PMID: 23231798.

26. Burgess JL, Unal ER, Nietert PJ, Newman RB. Risk of late preterm stillbirth and neonatal morbidity for monochorionic and dichorionic twins. Am J Obstet Gynecol. 2014; 210:578. PMID: 24607757.
27. Jung YJ, Kwon JY, Cho HY, Park YW, Kim YH. Comparison of the performance of screening test for gestational diabetes in singleton versus twin pregnancies. Obstet Gynecol Sci. 2015; 58:439–445. PMID: 26623406.

Table 1
Maternal characteristics and pregnancy outcome
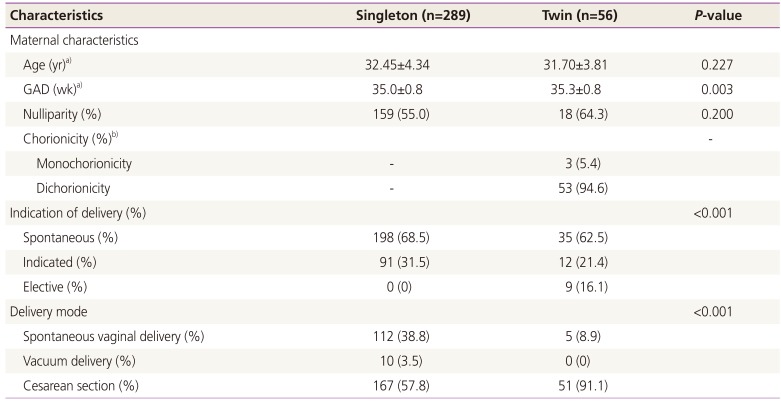
Table 2
Neonatal characteristics
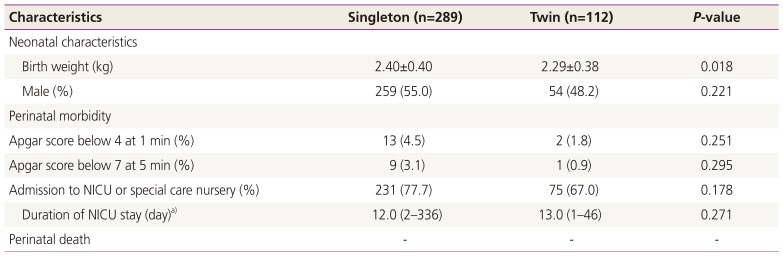
Table 3
Composite morbidity in late preterm birthsa)




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download