Abstract
Objective
To assess the predictive capacity of cervical length (CL) measurement underwent during the second trimester ultrasound for prediction preterm birth <32, 34, and 37 weeks of gestation in an unselected risk population.
Methods
A retrospective cohort study was performed with 751 singleton pregnancies between 20 and 24+6 weeks of gestation. The CL measurement (mm) using the transvaginal route was obtained in a sagittal view and the calipers positioned to measure the linear distance between the triangular area of echodensity at the external os and the internal os. To compare the preterm (<37 weeks) and term births (≥37 weeks), we used unpaired t test. We assessed whether the CL measurement was dependent of gestational age by performing a linear regression and assessing the coefficient of determination (R2). We additionally assessed the accuracy of CL measurement to predict preterm birth by assessing the area under receiver operating characteristics curves with its respective confidence intervals (CIs) 95%.
Results
Preterm birth <37 weeks was found in 13.6% (102/751) of pregnant women. Short cervix (≤25 mm) was found in 2.7% (20/751) of pregnancies. Only 30% (6/20) of pregnant women with short cervix have used progesterone to prevent preterm birth. There was a weak correlation between CL measurement and gestational age at delivery (R2=0.01, P=0.002). Receiver operating characteristics curve analysis of the ability of CL measurement to predict preterm birth <32, 34, and 37 weeks, showed an area under the curve of 0.693 (95% CI, 0.512 to 0.874), 0.472 (95% CI, 0.353 to 0.591), 0.490 (95% CI, 0.426 to 0.555), respectively.
Spontaneous preterm birth is a complex obstetric and perinatal problem and represents the main cause of perinatal morbidity and mortality [1]. Great efforts have been done to identify high-risk groups for Preterm birth and improve the perinatal outcomes.
Neonatal death of preterm births is mainly dependent on gestational age at delivery and decreases from less than 44.2% for those born at 23 weeks to 0% by 34 weeks [2]. The risk of severe neonatal morbidity decreases from 44.2% for those born at 23 weeks to less than 4.4% by 34 weeks [2]. Consequently, prediction of the high-risk groups for preterm birth, especially at ≤34 weeks, and useful intervention to prevent this complication of pregnancy constitute major challenges in obstetrics.
Cervical length (CL) measurement in the second trimester ultrasound has been studied extensively and has been inversely correlated with spontaneous preterm birth [3]. Although controversial, a universal CL measurement screening has been proposed, after a publication of randomized controlled trial demonstrating that vaginal progesterone significantly reduced the risk of preterm birth in pregnant women with short cervix in the second trimester ultrasound [456].
Our main objective was evaluating the predictive capacity of CL measurement to premature birth <32, 34, and 37 weeks of gestation in an unselected risk population. The secondary objective was describing the local demographic characteristics and time of delivery of short cervix population.
We performed a retrospective cohort study between January 2012 and May 2016 with singleton pregnant women underwent routine second trimester ultrasound between 20 and 24+6 weeks of gestation from public and private health services of Uberaba-MG, Brazil. The option of transvaginal ultrasound for assessment of CL measurement was offered for all pregnant women at that moment. This study was approved by the ethics committee of Uberaba University, and a consent form was not necessary secondary to the retrospective nature of this study.
The inclusion criteria were the following: singleton pregnancies, gestational age at 20 to 24 weeks determined by last menstrual period and confirmed by ultrasound examination performed <20 weeks (crown-rump length between 11 and 13+6 weeks, and biparietal diameter between 14 and 20+6 weeks of gestation). The exclusion criteria were the following: premature rupture of membranes before inclusion, known or suspected chorioamnionitis, fetal demise, planned cervical cerclage, uterine Müllerian anomalies, Preterm delivery for medical reasons and absence of perinatal outcome information in our electronic database. The CL was assessed only once during the study and postnatal outcomes were checked using the Astraia database (Astraia Software, Munich, Germany).
The ultrasound examinations were performed in the Mario Palmério University Hospital. Pregnant women are asked to empty their bladder and are placed in the dorsal lithotomy position. Ultrasound examinations were performed using the transvaginal approach with an Accuvix V20 (Samsung, Seoul, Korea) or a Voluson E6 (General Electric, Milwaukee, WI, USA) apparatus. All ultrasound examinations were carried out by only two examiners (ABP and TMRCC), both with Fetal Medicine Foundation Certificate accreditation for competence in cervical assessment. The probe was placed in the anterior fornix of the vagina and care was taken to avoid exerting undue pressure on the cervix, which might artificially lengthen it. A sagittal view of the cervix was obtained and the sonolucent endocervical mucosa (cervical gland area) was used as a guide to the true position of the internal os, thereby avoiding confusion with the lower segment of the uterus [7]. The calipers were used to measure the linear distance between the triangular area of echodensity at the external os and the internal os. Each ultrasound examination was performed over a period of about 3 minutes in order to observe any dynamic changes in the CL (Fig. 1A). Short cervix was considered when CL measurement ≤25 mm at 20 to 24+6 weeks of gestation (Fig. 1B). All pregnant women with CL measurement ≤25 mm were recommended to receive 200 mg daily vaginal proges-terone treatment until 37 weeks.
The data was transferred to an Excel spread sheet (Microsoft Corp., Redmond, WA, USA) and analysed by one of the authors (WPM) using PASW ver. 18.0 (SPSS Inc., Chicago, IL, USA) and GraphPad ver. 5.0 (GraphPad Software, San Diego, CA, USA). The maternal characteristics as height, weight, body mass index, number of pregnancies, parity and gestational age at ultrasound examination were expressed by median and ranges. We assessed whether the CL measurement was dependent of gestational age by performing a linear regression and assessing the coefficient of determination (R2). We additionally assessed the accuracy of CL measurment to predict preterm birth (<32, 34, and 37 weeks) by assessing the area under receiver operating characteristic (ROC) curves. For the interpretation we considered a test with an area under ROC curve <0.75 as being unlikely to be clinically useful [8].
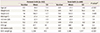
During the study period, 2,769 pregnant women were underwent routine second trimester ultrasound between 20 and 24+6 weeks of gestation. A total of 2,018 pregnant women were excluded from our study as following: 9 fetal demise, 911 absence of CL measurement for different reasons, and 1,098 absence of perinatal outcomes. For statistical analyzes, 751 pregnant women fulfilled the inclusion criteria. The demographic characteristics of the patients are demonstrated in Table 1.
Preterm birth <37 weeks was found in 13.7% (102/751), while short cervix was found in 2.7% (20/751) of pregnant women. Short cervix and preterm birth <37 weeks was found in 2.9% (03/102), while short cervix and birth >37 weeks was found in 2.6% (17/649).
Progesterone has been advice for all pregnant women with short cervix underwent CL screen between 20 and 24+6 weeks of gestation. Unfortunately, 70% (14/20) of pregnant women referred have not used progesterone according the medical advice. Among these patients, 7.1% (1/14) and 92.9 % (13/14) have had birth <37 and >37 weeks, respectively. Correct use of progesterone was found in 30% (6/20) of pregnant women with short cervix. Among progesterone users, 33.3% (2/6) and 66.6% (4/6) have had birth <37 and >37 weeks, respectively.
We have found a weak correlation between CL measurement and gestational age of delivery (R2=0.01, P=0.002). When all pregnant women who have administered vaginal progesterone were excluded, a non-significant weak correlation have been found between CL measurement and gestational age of delivery (R2<0.001, P=0.92) (Fig. 2).
ROC curve analysis of the ability of CL measurement to predict preterm birth <32, 34, and 37 weeks of gestation, showed an area under the curve of 0.693 (95% confidence interval [CI], 0.512 to 0.874), 0.472 (95% CI, 0.353 to 0.591), 0.490 (95% CI, 0.426 to 0.555), respectively (Fig. 3).
Despite of the great efforts to avoid the preterm birth, birth rate <37 weeks is still rising. The rate of preterm birth in the USA, Europe, and Brazil is around 12.8%, 10.0%, and 11.5%, respectively [910]. In our study, the rate of preterm birth was 13.7%. Our findings are in agreement to the USA data but slightly higher than Brazilian preterm birth rate. A possible explanation for this finding might be the tertiary characteristics of our university hospital or underreported cases of preterm delivery in Brazil.
Short cervix, traditionally defined as a transvaginal ultrasound measurement <25 mm in midtrimester of pregnancy, is an important risk factor for preterm birth and has emerged as one of strongest and most consistent predictors of preterm birth in asymptomatic pregnant women [311]. In singleton pregnant women without prior history of preterm birth, the rate of cervical shortening has been reported to be 2% (<25 mm) and 1.2% (<20 mm) [121314]. However, Miller et al. [4] found lower rate (0.9%) of CL <25 mm among 18,250 pregnant women undergoing CL measurement screening. These authors suggested that limiting CL measurement to those with risk factors for short cervix could improve overall specificity of screening [4]. In our population, the rate of short cervix was slightly higher (2.7%) than previous reports [4121314]. The incidence of short cervix in our population could be an important tool to assess the overall cost effectiveness of a local screening program.
In a randomized controlled trial, Fonseca et al. [5] found that vaginal progesterone (200 mg capsules) administered to pregnant women with a CL measurement ≤15 mm at median gestational age of 23 weeks decreased the rate of spontaneous preterm birth (<34 weeks of gestation) in 44%. In other randomized controlled trial, vaginal progesterone (90 mg gel) was administered to pregnant women with CL measurement <20 mm and occurred 45% of reduction in the rate of preterm birth <33 weeks of gestation [15]. A very recent updated meta-analysis, including data from the OPPTIMUM study, reaffirms that vaginal progesterone reduces the risk of preterm birth and neonatal morbidity and mortality in women with a singleton gestation and a mid-trimester CL ≤25 mm, without any deleterious effects on neurodevelopment outcome. Differently of these trials, we have administered 200 mg vaginal progesterone to pregnant women with CL measurement <25 mm. We cannot evaluate the effect of progesterone in the reduction rate of preterm birth because of the small sample size and low adherence of pregnant women participants. In Brazil, vaginal progesterone is an expensive drug and it is not available in public health units for the pregnant women with short cervix.
There was a weak correlation between CL measurement and gestational age at delivery even after exclude all pregnant women who have used progesterone. This unusual finding could be related with the small sample size of our study or different characteristics of our population. In a recent study from our group which established reference values for CL measurement between 20 and 24+6 weeks of gestation in 996 singleton pregnancies, CL measurement did not modify significantly with gestational age [16].
According to Society of Maternal-Fetal Medicine, the issue of universal transvaginal CL measurement screening of singleton pregnancies without previous history of preterm birth remains controversial [12]. It can be viewed as reasonable and considered by individual practitioners [12]. Although, some studies have been demonstrated that the universal screening can be implemented successfully with 85% of pregnant women screened and associated with a reduction in the rate of preterm birth [1314].
We have found that CL measurement <25 mm was not a predictor of preterm birth <32 weeks of gestation with unlikely clinical application for our population. Furthermore, CL measurement <25 mm was not significantly associated with preterm birth <34 and 37 weeks of gestation in our study. In a recent editorial, single CL measurement seems unreasonable serve as a universal predictor of preterm birth when multiple mechanisms are involved [17]. Differently, Celik et al. [18] analyzing 59,313 women with CL measurement <15 mm, demonstrated that the best predictor of spontaneous preterm birth was provided by CL measurement adding obstetric history. Because of the small sample size, CL measurement cut off and the non-addition of maternal characteristics could compromise our results when compared with Celik's study.
In summary, there was a weak correlation between CL measurement and gestational age at delivery. In an unselected risk population, CL measurement screening at 20 to 24+6 weeks does not seem to be a good predictor of preterm birth. Larger prospective studies are necessary to confirm our findings.
Figures and Tables
 | Fig. 1Transvaginal ultrasound examination showing the cervical length measurement at 22 weeks of gestation. (A) Normal cervical length measurement and (B) short cervix with funneling. |
 | Fig. 2Scatter plot of the correlation between cervical length measurement (mm) and gestational age (weeks) at delivery. |
 | Fig. 3Receiver operating characteristics curves to display the cervical length measurement ability to predict preterm birth (A) <32, (B) 34, and (C) 37 weeks of gestation. Diagonal segments are produced by ties. |
Table 1
Demographic characteristics of study population
References
1. Iams JD, Romero R, Culhane JF, Goldenberg RL. Primary, secondary, and tertiary interventions to reduce the morbidity and mortality of preterm birth. Lancet. 2008; 371:164–175.
2. Manuck TA, Rice MM, Bailit JL, Grobman WA, Reddy UM, Wapner RJ, et al. Preterm neonatal morbidity and mortality by gestational age: a contemporary cohort. Am J Obstet Gynecol. 2016; 215:103.
3. Heath VC, Southall TR, Souka AP, Elisseou A, Nicolaides KH. Cervical length at 23 weeks of gestation: prediction of spontaneous preterm delivery. Ultrasound Obstet Gynecol. 1998; 12:312–317.
4. Miller ES, Tita AT, Grobman WA. Second-trimester cervical length screening among asymptomatic women: an evaluation of risk-based strategies. Obstet Gynecol. 2015; 126:61–66.
5. Fonseca EB, Celik E, Parra M, Singh M, Nicolaides KH. Fetal Medicine Foundation Second Trimester Screening Group. Progesterone and the risk of preterm birth among women with a short cervix. N Engl J Med. 2007; 357:462–469.
6. Cahill AG, Odibo AO, Caughey AB, Stamilio DM, Hassan SS, Macones GA, et al. Universal cervical length screening and treatment with vaginal progesterone to prevent preterm birth: a decision and economic analysis. Am J Obstet Gynecol. 2010; 202:548.
7. Sonek J, Shellhaas C. Cervical sonography: a review. Ultrasound Obstet Gynecol. 1998; 11:71–78.
8. Sotiriadis A, Papatheodorou SI, Martins WP. Synthesizing Evidence from Diagnostic Accuracy TEsts: the SEDATE guideline. Ultrasound Obstet Gynecol. 2016; 47:386–395.
9. Hamilton BE, Martin JA, Ventura SJ. Births: preliminary data for 2006. Natl Vital Stat Rep. 2007; 56:1–18.
10. Leal MD, Esteves-Pereira AP, Nakamura-Pereira M, Torres JA, Theme-Filha M, Domingues RM, et al. Prevalence and risk factors related to preterm birth in Brazil. Reprod Health. 2016; 13:Suppl 3. 127.
11. Romero R, Nicolaides KH, Conde-Agudelo A, O'Brien JM, Cetingoz E, Da Fonseca E, et al. Vaginal progesterone decreases preterm birth ≤ 34 weeks of gestation in women with a singleton pregnancy and a short cervix: an updated meta-analysis including data from the OPPTIMUM study. Ultrasound Obstet Gynecol. 2016; 48:308–317.
12. Society for Maternal-Fetal Medicine (SMFM). McIntosh J, Feltovich H, Berghella V, Manuck T. The role of routine cervical length screening in selected high- and low-risk women for preterm birth prevention. Am J Obstet Gynecol. 2016; 215:B2–B7.
13. Temming LA, Durst JK, Tuuli MG, Stout MJ, Dicke JM, Macones GA, et al. Universal cervical length screening: implementation and outcomes. Am J Obstet Gynecol. 2016; 214:523.
14. Son M, Grobman WA, Ayala NK, Miller ES. A universal mid-trimester transvaginal cervical length screening program and its associated reduced preterm birth rate. Am J Obstet Gynecol. 2016; 214:365.
15. Hassan SS, Romero R, Vidyadhari D, Fusey S, Baxter JK, Khandelwal M, et al. Vaginal progesterone reduces the rate of preterm birth in women with a sonographic short cervix: a multicenter, randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol. 2011; 38:18–31.
16. Peixoto AB, da Cunha Caldas TM, Alamy AH, Martins WP, Bruns RF, Araujo Junior E. Reference values for the cervical length measurement in the second trimester of pregnancy using the transvaginal ultrasound in a large Brazilian population. Obstet Gynecol Sci. 2016; 59:303–306.
17. Hughes K, Kane SC, Araujo Junior E, Da Silva Costa F, Sheehan PM. Cervical length as a predictor for spontaneous preterm birth in high-risk singleton pregnancy: current knowledge. Ultrasound Obstet Gynecol. 2016; 48:7–15.
18. Celik E, To M, Gajewska K, Smith GC, Nicolaides KH. Fetal Medicine Foundation Second Trimester Screening Group. Cervical length and obstetric history predict spontaneous preterm birth: development and validation of a model to provide individualized risk assessment. Ultrasound Obstet Gynecol. 2008; 31:549–554.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download