Abstract
Objective
Premenstrual syndrome (PMS) affects millions of women and is known as the most important disorder among them. The very aim of the present study was to evaluate the effects of low dose calcium on severity of PMS.
Methods
This study can be considered as a double-blind randomized clinical trial. Female students of Hamadan University of Medical Sciences diagnosed with PMS in 2014 participated in the present study. Sixty-six female students diagnosed with PMS were involved in the experimental and control groups. The participants were randomly assigned into two groups to receive 500 mg of calcium daily or placebo for two months. Severity of PMS was detected by Daily Record of Severity of Problems, which was used to measure symptoms during one menstrual cycle before and two menstrual cycles after the intervention.
Results
No signifcant differences were observed in the mean scores of PMS symptoms between calcium and placebo groups before the treatment (P=0.74). However, signifcant differences were noticed between the two intervention groups in the first (P=0.01) and second menstrual cycles (P=0.001) after the intervention. The differences were significant in subgroups of anxiety, depression, emotional changes, water retention, and somatic changes in calcium group compared with placebo group in the menstrual cycle before the intervention and two menstrual cycles after the intervention and among menstrual cycles (0, cycle 1, cycle 2) in calcium group (P=0.01).
Premenstrual syndrome (PMS) affects millions of women and is recognized as the most significant disorder among women [1]. Several days to 2 weeks before menses, a range of emotional, behavioral, and physical symptoms can occur. These symptoms known as PMS are decreased following the menstrual period [2]. Prevalence of PMS during the reproductive period has been reported to be between 70% to 90% [3].
The most common symptoms in PMS include abdominal bloating, breast tenderness, anxiety, crying spells, depression, fatigue, lack of energy, anger and irritability, changes in appetite, and varying degrees of edema [4]. Etiology of PMS still remains unknown; however, it is understood as a psychoendocrine disorder. Involvement of sex steroids is supported by the relief of PMS symptoms with the suppression of ovulation; however, no strong evidence is provided to confirm that reproductive hormones are the sole cause of PMS [5].
A number of studies have suggested that administration of supplements including vitamin D and E, thiamin, and riboflavin is associated with decreased development of PMS [678910]. Shamberger [11] revealed that levels of calcium and some trace elements in red blood cells were lower than normal in women with PMS. Some studies have reported significant effect of 1,000 mg of calcium supplement on decrease of PMS [41213]. The calcium effect on PMS is correlated to the production of serotonin and tryptophan metabolism [14].
With consideration of the mentioned findings, the present study examined the efficacy of 500 mg of calcium per day for two months on reduction of PMS symptoms among students of Hamadan University of Medical Sciences, in west of Iran.
The present double-blind randomized clinical trial was conducted from January 10 to March 18, 2014 among female students of Hamadan University of Medical Sciences in west of Iran. The study was registered in the www.irct.ir as IRCT 201309296888 after taking approval from the Research Ethics Committee of Hamadan University of Medical Sciences.
Written informed consent was received from all the participants. Inclusion criteria applied for all students were as follows: (1) no ongoing hormone therapy; having moderate to severe PMS specified based on Diagnostic and Statistical Manual of Mental Disorders, 4th edition criteria. This syndrome was defined by the presence of at least 5 symptoms problematic enough to warrant treatment, one of which is a functionally impairing affective symptom and (2) no clinical history of major psychological problems. According to calculations performed to determine the differences about 30% and pain reduction according to 80% power scale and significance level 0.05, 33 patients in each group were required Which is justified the sample size of 66 subjects in this study.
The eligible women were randomly assigned into two groups using the balance block randomization method. To do so, four sheets of paper were prepared. “C” was written for calcium on two of the prepared sheets, and on the other two sheets, “P” was written for placebo. The sheets were pooled, placed in a container, and randomly drawn one at a time for each patient without replacement until all 4 sheets were drawn. The four sheets were then placed back into the container, and this action was repeated until the sample size was reached. The allocations remained concealed during the study. For this purpose, random allocation was conducted and labeled by a pharmacologist, so that neither the students nor the distributer who evaluated the effect of the interventions was aware of the administered drugs until the data was analyzed, and the labels were decoded.
Calcium tablets of 500 mg daily were provided after lunch for two cycles. Participants in the placebo group received placebo tablet of 500 mg (starch), which was identical to the calcium tablet. Both calcium and placebo tablets were packed in similar packages and were given to a person to be distributed, so that neither the distributer nor the students were aware of the package contents.
Severity of symptoms was determined based on Daily Record of Severity of Problems scale in one menstrual cycle before the intervention and two menstrual cycles after the intervention. Participants rated the severity of symptoms as 0 to 3 in their forms. While absence of the symptom was scored as 0, score of 1indicated mild symptoms, which did not interfere with daily activities such as education and work. Score of 2 represented moderate symptoms, which affected daily activities to some extent. However, score of 3 was indicative of severe symptoms, which prevented the patient from daily activities. To simplify the comparisons between groups in terms of the effectiveness of calcium on reducing each of the symptoms, the overall 30 symptoms of the menstrual diary were divided into 5 subgroups according to the Abraham's classification system [815]. The effectiveness of each compound on the symptoms was then evaluated in detail. The subgroups were as follows: anxiety (stress, irritability, and anxiety); depression (depression and seclusion, social inactivity, crying, impatience, desire to stay at home, anger, forgetfulness, insomnia, and lack of concentration); emotional changes (cravings for sweets, palpitation, weakness, decreased energy, increased appetite, and fatigue); water retention (pain and breast tenderness, swelling of legs, abdominal bloating, pain, and discomfort); and somatic changes (feeling cold, nausea, frequent urination, hot flashes, back pain, headaches, acne, oily skin, joint pain, and muscle pain).
Two groups' severity of symptoms was compared with t-test. Analysis of variance was applied to compare the values of menstrual cycles (0, cycle 1, cycle 2) in calcium and placebo groups. All the hypotheses were two-sided, and P-values <0.05 were considered to be statistically significant. SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analyses.
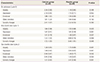
From 66 involved participants, one in the calcium group and one in the placebo group did not return to complete the follow-up data. Hence, they were excluded from the study (Fig. 1). In the current study, the mean age of participants in the intervention and placebo groups was 21.09 and 20.81 years, respectively. The two groups were similar in terms of the age of menarche, dysmenorrheal age, duration of menstruation, interval of menstruation, body mass index, regular menstrual cycle, and regular exercise activity (Table 1).
In Table 2, significant differences in the mean scores of PMS symptoms were not found between the intervention and placebo groups before treatment (P=0.74). However, significant difference was observed between two groups in the first menstrual cycle (P=0.01) and the second menstrual cycle (P=0.001) after the intervention and among menstrual cycles (0, cycle 1, cycle 2) in calcium group (P=0.01). The differences among menstrual cycles (0, cycle 1, cycle 2) in placebo group were not statistically significant (P=0.2).
Comparisons of changes in the mean scores of PMS before and after the intervention in placebo and calcium groups are summarized in Table 3. The differences were significant in subgroups of depression, emotional changes, and somatic changes in calcium group compared with placebo group in the menstrual cycle before the intervention and in two menstrual cycles after the intervention. The comparisons were not significant between two groups in the subgroup of water retention in two menstrual cycles after the intervention. The side effect in two groups was not reported.
The findings of this study demonstrated significant effects of low dose calcium (500 mg) on reduction of PMS symptoms and among menstrual cycles (0, cycle 1, cycle 2). The obtained results corroborate those of previous studies regarding the positive effect of calcium supplementation on premenstrual symptoms (2, 4, 5, 12, 13). Ghanbari et al. [16] reported that comparison of the results obtained before and after intervention revealed that depression and sadness were significantly reduced in the women receiving calcium 1,000 mg/day (27%) in comparison with those receiving placebo (7%) (P<0.002). These results were similar to those reported by Penland and Johnson [17]. The mentioned study revealed that calcium supplements alleviated concentration problems, and affective and behavioral variations related to PMS (P=0.01).
In another study conducted in this regard, intake of calcium (500 mg) plus vitamin D (200 mg) supplement modestly reduced PMS symptoms, although the improvements did not exceed the placebo [2]. In a larger placebo-controlled study, calcium supplementation (1,200 mg/day) significantly reduced premenstrual depression, fatigue, edema, and pain in women with PMS [3].
In a review study conducted in 2015, numerous non-pharmacologic treatments were utilized; however, efficacy was reported only for calcium supplements [5]. The other study was performed in 2016 that students in a group received combined vitamin B6 (40 mg) and calcium (500 mg) and in other group only vitamin B6 twice a day. The result showed that although the severity of symptoms decreased in both groups, this reduction was more significant in the combined calcium and vitamin B6 group [14].
Previous studies indicated that daily intake of 1,000 mg calcium reduced PMS symptoms [121316]. The present study reported that daily intake of 500 mg calcium was effective in reducing PMS symptoms. Therefore, intake of lower doses of calcium can decrease PMS symptoms similar to the reduction occurring in 1,000 mg dose of calcium intake. Furthermore, daily intake of calcium for longer duration was caused that the symptoms more were relieved. Overall, the results of the mentioned studies suggest that treatment with calcium supplements is an effective technique for reducing mood disorders observed in PMS. Furthermore, calcium supplementation is a cost-effective, beneficial, and effective treatment for reducing symptoms of PMS.
The main limitation of the present study was small sample size of the study groups. If the sample size was large enough, the differences between the trial groups would be indicated more clearly with less random error. In addition, the present study was conducted addressing a single group of adolescents; therefore, the results may not be generalizable to females outside that age range.
Figures and Tables
Table 1
Baseline characteristics and clinical data of the study population

Table 2
Scores of premenstrual syndrome before and after the intervention in the two groups

Table 3
Comparison of changes in mean premenstrual syndrome scores before and after the intervention in two groups
References
1. Fathizadeh N, Ebrahimi E, Valiani M, Tavakoli N, Yar MH. Evaluating the effect of magnesium and magnesium plus vitamin B6 supplement on the severity of premenstrual syndrome. Iran J Nurs Midwifery Res. 2010; 15:Suppl 1. 401–405.
2. Khajehei M, Abdali K, Parsanezhad ME, Tabatabaee HR. Effect of treatment with dydrogesterone or calcium plus vitamin D on the severity of premenstrual syndrome. Int J Gynaecol Obstet. 2009; 105:158–161.
3. Thys-Jacobs S, Starkey P, Bernstein D, Tian J. Calcium carbonate and the premenstrual syndrome: effects on premenstrual and menstrual symptoms. Premenstrual Syndrome Study Group. Am J Obstet Gynecol. 1998; 179:444–452.
4. Ghanbari Z, Haghollahi F, Shariat M, Foroshani AR, Ashrafi M. Effects of calcium supplement therapy in women with premenstrual syndrome. Taiwan J Obstet Gynecol. 2009; 48:124–129.
5. Freeman EW. Therapeutic management of premenstrual syndrome. Expert Opin Pharmacother. 2010; 11:2879–2889.
6. Chocano-Bedoya PO, Manson JE, Hankinson SE, Johnson SR, Chasan-Taber L, Ronnenberg AG, et al. Intake of selected minerals and risk of premenstrual syndrome. Am J Epidemiol. 2013; 177:1118–1127.
7. Salamat S, Ismail KM, O'Brien S. Premenstrual syndrome. Obstet Gynecol Reprod Med. 2008; 18:29–32.
8. Abraham GE. Nutritional factors in the etiology of the premenstrual tension syndromes. J Reprod Med. 1983; 28:446–464.
9. Shobeiri F, Jenabi E. The effects of vitamin E on muscular pain reduction in students affected by premenstrual syndrome. Iran J Obstet Gynecol Infertil. 2014; 17:1–5.
10. Shobeiri F, Oshvandi K, Nazari M. Clinical effectiveness of vitamin E and vitamin B6 for improving pain severity in cyclic mastalgia. Iran J Nurs Midwifery Res. 2015; 20:723–727.
11. Shamberger RJ. Calcium, magnesium, and other elements in the red blood cells and hair of normals and patients with premenstrual syndrome. Biol Trace Elem Res. 2003; 94:123–129.
12. Akhlaghi F, Hamedi A, Javadi Z, Hosseinipoor F. Effects of calcium supplementation on premenstrual syndrome. Razi J Med Sci. 2004; 10:669–675.
13. Kermani AZ, Taavoni S, Hosseini AF. Effect of combined calcium and vitamin E consumption on premenstrual syndrome. Iran J Nurs. 2010; 23:8–14.
14. Masoumi SZ, Ataollahi M, Oshvandi K. Effect of combined use of calcium and vitamin B6 on premenstrual syndrome symptoms: a randomized clinical trial. J Caring Sci. 2016; 5:67–73.
15. Ebrahimi E, Khayati Motlagh S, Nemati S, Tavakoli Z. Effects of magnesium and vitamin b6 on the severity of premenstrual syndrome symptoms. J Caring Sci. 2012; 1:183–189.
16. Ghanbari Z, Manshavi FD, Jafarabadi M. The effect of three months regular aerobic exercise on premenstrual syndrome. J Family Reprod Health. 2008; 2:167–171.
17. Penland JG, Johnson PE. Dietary calcium and manganese effects on menstrual cycle symptoms. Am J Obstet Gynecol. 1993; 168:1417–1423.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download