Abstract
Objective
To assess the role of preoperative and postoperative serum C-reactive protein (CRP) level on the prediction of pregnancy outcomes following ultrasound-indicated cerclage (UIC).
Methods
We retrospectively reviewed the medical records 44 women who underwent UIC between January 2011 and December 2011. UIC was performed between 14 and 24 weeks of gestation in women with short cervix. We divided UIC patients into two groups according to the gestational age at delivery (34 weeks) and compared the two groups. Group A was defined as patients who delivered ≥34 weeks of gestation, and group B as patients delivered <34 weeks. Correlation and receiver-operating characteristic curves were also analyzed for the prediction of preterm birth after UIC.
Results
Thirty women delivered ≥34 weeks (group A) and 14 women delivered <34 weeks (group B). Pre- and post-cerclage CRP were significantly lower in group A (pre-cerclage CRP, 1.1±1.0 vs. 11.4±6.2 mg/dL, P<0.001; post-cerclage CRP, 0.6±0.5 vs. 7.4±7.2 mg/dL, P<0.001). The mean gestational age at delivery in group A was 37.7±1.8 weeks and that in group B was 26.9±4.3 weeks (P<0.001). There were significant negative correlations between pre- and post-cerclage CRP and latency from UIC to delivery (r=-0.82, P<0.001; r=-0.70, P<0.001, respectively).
C-reactive protein (CRP) is a widely used marker which reflect inflammation and tissue damage [1]. The measurement of CRP is quick, safe, and relatively inexpensive method. The increase in serum CRP accompanies inflammatory diseases such as cancer, asthma, and neonatal intrapulmonary disease [2]. In obstetrics, the elevated serum level of CRP is associated with adverse pregnancy outcomes which include preeclampsia, chorioamnionitis, intrauterine growth restriction and preterm birth [13456].
Ultrasound-indicated cerclage (UIC) is beneficial for prolonging pregnancy in women with prior preterm birth and short cervix (<25 mm) [7]. There are some reports on the outcomes of UIC [89]. The authors demonstrated that UIC significantly prolonged pregnancy and resulted in favorable pregnancy outcomes. However, the predicting factors for the success of UIC have not been thoroughly evaluated. There is a need to develop biomarkers predicting the outcome of UIC. In this study, we investigated the relation between the preoperative and postoperative serum CRP levels and the efficacy of UIC.
This was a retrospective study of 44 women with UIC between January 2011 and December 2011. All women underwent UIC at Kangnam Sacred Heart Hospital, Hallym University Medical Center. UIC was performed between 14 and 24 weeks of gestation in singleton pregnant women with short cervix (<25 mm) and previous preterm birth. Short cervix was diagnosed by cervical sonographic screening using a standard method [10]. Women with visible bulging membrane into vagina, multiple pregnancy, fetus with structural anomalies, fetal chromosomal anomalies, vaginal bleeding, preterm premature rupture of membranes, preterm labor pain, chorioamnionitis, or women with chronic medical diseases were excluded. Prior to the UIC, microbiological analyses were performed by vaginal swabs with sterile swabs. The maternal serum CRP levels were measured twice at pre- and post-cerclage day 1.
UIC was performed using McDonald technique with Mersilene tape (Braun, Tuttlingen, Germany) under spinal anesthesia. UIC was technically successful in all patients. Prophylactic antibiotics, 1.0 g intravenous cefotiam twice a day, were given at least 3 days after admission. Tocolytics were not routinely administered after UIC. Cerclage sutures were routinely removed at 37 weeks of gestation if patients have no complications. When combined with preterm labor, premature rupture of membranes, or chorioamnionitis, cervical cerclages were removed at the discretion of maternal-fetal medicine specialists.
Maternal demographics and pregnancy outcomes following UIC were reviewed from patients' medical records. Patients with UIC were divided into two groups: one group is consisted of women who delivered at ≥34 weeks of gestation; the other group is consisted of women who delivered at <34 weeks of gestation. We compared the maternal demographics , preoperative and postoperative laboratory findings, and pregnancy outcomes between two groups.
Statistical analysis was performed with the IBM SPSS ver. 22.0 (IBM Corp., Armonk, NY, USA). Data are represented either as number and percent, or mean±standard deviation for continuous variables. Continuous variables were evaluated by Student's t-test or Mann-Whitney U-test, where appropriate. Chi-square analysis was used for categorical data. Correlations for continuous variables were assessed using either the Pearson or the Spearman test, depending on normal distribution. Receiver-operating characteristic curves were analyzed to predict preterm birth after UIC.
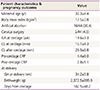
Table 1 demonstrates maternal demographics and pregnancy outcomes after UIC. The mean gestational age at cerclage was 20.5 weeks, and the mean cervical length at cerclage was 15.1 mm. Maternal serum CRP at post-cerclage was decreased compared to pre-cerclage CRP (pre-cerclage CRP, 4.4 mg/dL vs. post-cerclage CRP, 2.8 mg/dL). However, there was no statistically significant difference between pre- and post-cerclage CRP. Pregnancy outcomes following UIC were favorable. All 44 patients had live births and there was no neonatal death. The mean gestational age at delivery was 34.2 weeks, and the average birthweight was 2,372.5 g. The mean prolongation days after UIC were 102.5 days.
Thirty women delivered ≥34 weeks of gestation (group A), and 14 women delivered <34 weeks of gestation (group B). Table 2 shows the comparison of maternal demographics and pregnancy outcomes between two groups. There were no statistical differences in maternal demographics between two groups. Gestational age at cerclage, cervical length at cerclage, and cervical length at post-cerclage showed no significant differences between two groups. No significant difference in pre-cerclage labs was detected between two groups. The mean gestation age at delivery in group A was 37.7 weeks, whereas that in group B was 26.9 weeks. The major causes of preterm birth in group B were preterm premature rupture of membrane, chorioamnionitis, and preterm labor. There were significant differences in pre- and post-cerclage CRP between two groups: The mean pre-cerclage CRP in group A was 1.1 mg/dL, whereas that in group B was 11.4 mg/dL (P<0.001); The average post-cerclage CRP in group A was 0.6 mg/dL, whereas that in group B was 7.4 mg/dL (P<0.001). Both group showed decreased post-cerclage CRP level compared to pre-cerclage CRP level. However, it was not a statistically significant decrease (P=0.07). Fig. 1 demonstrates the negative correlations between pre- and post-cerclage CRP and latency from cerclage to delivery (r=-0.82, P<0.001; r=-0.70, P<0.001, respectively). Patients with lower pre- and post-cerclage CRP showed less preterm birth following UIC. We constructed receiver-operating characteristic curves of pre- and post-cerclage CRP to predict delivery <34 weeks of gestation. Area under curves of both pre- and post-cerclage CRP were significantly large (Fig. 2). Both pre- and post-cerclage CRP were useful in the prediction of preterm birth after UIC.
The present study suggests that both of pre- and post-cerclage CRP are useful in predicting the risk of preterm birth following UIC. Women with lower pre- and post-cerclage CRP is likely to prolong pregnancy after UIC.
It is widely known that a short cervix less than 25 mm in mid-trimester is high risk for preterm birth [11]. There were debates on the efficacy of UIC, but a meta-analysis demonstrated that UIC in women with prior preterm birth and short cervix (<25 mm) is beneficial in reducing preterm birth [12]. There have been some reports on the pregnancy outcomes following UIC. The authors reported that UIC resulted in favorable pregnancy outcome with high incidence of live births [1314].
However, the predicting factors for the pregnancy outcome after UIC have not been thoroughly studied. There was a report on cervical mucus interleukin (IL)-8 in UIC. The increase of cervical mucus IL-8 was associated with preterm birth following UIC [15]. There are some limitations on cervical mucus IL-8; it is not a widely used lab and obstetricians could not get the prompt result of cervical mucus IL-8. CRP is stable, inexpensive, quick marker for inflammation. In this respect, serum CRP is more advantageous than cervical mucus IL-8.
There were two reports on serum CRP in patients with emergency cerclage [1617]. The authors demonstrated that serum CRP predicted the outcome of emergency cerclage in women with dilated cervix and bulging membrane [1617]. The study participants in the current study were different from those studies; The present study mainly focused on women with sonographically short cervix and prior preterm birth. We excluded women with dilated cervix and bulging membrane in this study. To our knowledge, our study is the first report to evaluate the efficacy of serum CRP in UIC.
Interestingly, there were no significant differences in pre-cerclage microbiologic labs between group A and group B in this study. It may represent that cervical shortening in women with previous preterm birth is affected by other inflammatory process in cervix itself. In the current study, post-cerclage CRP is decreased compared to pre-cerclage CRP. Although the difference between pre- and post-cerclage CRP was not statistically significant, it may suggest that UIC and perioperative antibiotics prevent further inflammatory process in women with short cervix. Our study showed that women with high level of pre-cerclage CRP tended to deliver more prematurely. It may be beneficial for women with high level of preoperative CRP to have cerclage after confirming decreased level of CRP with antibiotic therapy.
Although our study was limited by the small sample size and retrospective study design, the present study suggests the efficacy of pre- and post-cerclage serum CRP for the prediction of preterm birth after UIC in women with short cervix and prior preterm birth. In the future prospective randomized trial is need.
Figures and Tables
Fig. 1
Correlations between pre- and post-cerclage C-reactive protein (CRP) and latency from ultrasound-indicated cerclage (UIC) to delivery. (A) Negative correlation between pre-cerclage CRP and prolongation days after UIC. (B) Negative correlation between post-cerclage CRP and latency from UIC to delivery.

Fig. 2
Receiver-operating characteristic curves of pre- and post-cerclage C-reactive protein (CRP) to predict delivery <34 weeks of gestation. The areas under curve (AUCs) are demonstrated in the charts.

References
1. Kwak DW, Cho HY, Kwon JY, Park YW, Kim YH. Usefulness of maternal serum C-reactive protein with vaginal Ureaplasma urealyticum as a marker for prediction of imminent preterm delivery and chorioamnionitis in patients with preterm labor or preterm premature rupture of membranes. J Perinat Med. 2015; 43:409–415.
2. Ahmed SK, Mahmood N, Malalla ZH, Alsobyani FM, Al-Kiyumi IS, Almawi WY. C-reactive protein gene variants associated with recurrent pregnancy loss independent of CRP serum levels: a case-control study. Gene. 2015; 569:136–140.
3. Lohsoonthorn V, Qiu C, Williams MA. Maternal serum C-reactive protein concentrations in early pregnancy and subsequent risk of preterm delivery. Clin Biochem. 2007; 40(5-6):330–335.
4. Best LG, Saxena R, Anderson CM, Barnes MR, Hakonarson H, Falcon G, et al. Two variants of the C-reactive protein gene are associated with risk of pre-eclampsia in an American Indian population. PLoS One. 2013; 8:e71231.
5. Tjoa ML, van Vugt JM, Go AT, Blankenstein MA, Oudejans CB, van Wijk IJ. Elevated C-reactive protein levels during first trimester of pregnancy are indicative of preeclampsia and intrauterine growth restriction. J Reprod Immunol. 2003; 59:29–37.
6. Morales E, Guerra S, Garcia-Esteban R, Guxens M, Alvarez-Pedrerol M, Bustamante M, et al. Maternal C-reactive protein levels in pregnancy are associated with wheezing and lower respiratory tract infections in the offspring. Am J Obstet Gynecol. 2011; 204:164.e1–164.e9.
7. Berghella V, Rafael TJ, Szychowski JM, Rust OA, Owen J. Cerclage for short cervix on ultrasonography in women with singleton gestations and previous preterm birth: a meta-analysis. Obstet Gynecol. 2011; 117:663–671.
8. Nelson L, Dola T, Tran T, Carter M, Luu H, Dola C. Pregnancy outcomes following placement of elective, urgent and emergent cerclage. J Matern Fetal Neonatal Med. 2009; 22:269–273.
9. Chan LL, Leung TW, Lo TK, Lau WL, Leung WC. Indications for and pregnancy outcomes of cervical cerclage: 11-year comparison of patients undergoing history-indicated, ultrasound-indicated, or rescue cerclage. Hong Kong Med J. 2015; 21:310–317.
10. Berghella V, Bega G. Ultrasound evaluation of the cervix. In : Callen PW, editor. Ultrasonography in obstetrics and gynecology. 5th ed. Philadelphia (PA): Saunders/Elsevier;2008. p. 698–720.
11. Iams JD, Goldenberg RL, Meis PJ, Mercer BM, Moawad A, Das A, et al. The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med. 1996; 334:567–572.
12. Berghella V, Odibo AO, To MS, Rust OA, Althuisius SM. Cerclage for short cervix on ultrasonography: meta-analysis of trials using individual patient-level data. Obstet Gynecol. 2005; 106:181–189.
13. Berghella V. Transvaginal ultrasound assessment of the cervix and prediction of spontaneous preterm birth [Internet]. [place unknown]: cited 2016 Feb 6. Available from: http://www.uptodate.com.
14. Skupski DW, Lin SN, Reiss J, Eglinton GS. Extremely short cervix in the second trimester: bed rest or modified Shirodkar cerclage? J Perinat Med. 2014; 42:55–59.
15. Sakai M, Shiozaki A, Tabata M, Sasaki Y, Yoneda S, Arai T, et al. Evaluation of effectiveness of prophylactic cerclage of a short cervix according to interleukin-8 in cervical mucus. Am J Obstet Gynecol. 2006; 194:14–19.
16. Kobayashi M, Ohkuchi A, Matsubara S, Izumi A, Hirashima C, Suzuki M. C-reactive protein levels at pre-/post-indicated cervical cerclage predict very preterm birth. J Perinat Med. 2011; 39:151–155.
17. Minakami H, Matsubara S, Izumi A, Kosuge S, Watanabe T, Iwasaki R, et al. Emergency cervical cerclage: relation between its success, preoperative serum level of C-reactive protein and WBC count, and degree of cervical dilatation. Gynecol Obstet Invest. 1999; 47:157–161.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download