Abstract
Objective
The aim of this study was to evaluate obstetric outcomes of external cephalic version (ECV) performed at or near term.
Methods
Single pregnant woman with breech presentation at or near term (n=145), who experienced ECV by one obstetrician from November 2009 to July 2014 in our institution were included in the study. Maternal baseline characteristic and fetal ultrasonographic variables were checked before the procedure. After ECV, the delivery outcomes of the women were gathered. Variables affecting the success or failure of ECV were evaluated.
Results
Success rate of ECV was 71.0% (n=103). Four variables (parity, amniotic fluid index, fetal spine position and rotational direction) were observed to be in correlation with success or failure of ECV. In contactable 83 individuals experienced successful ECV, cesarean delivery rates were 18.1%, 28.9%, and 5.3% in total, nulliparas, and multiparas, respectively.
In many developing and developed countries, a high cesarean delivery rate has become a public health problem. In 2012, the cesarean delivery rate in the United States was 32.8%, and in Korea was 36.9% [12]. Many people agree that such a high rate exceeds the limit of necessity and various means have been devised to reduce it. For example, institutional cesarean delivery rates have been released to public in Korea from 2010, but no change in the cesarean delivery rate in Korea has been seen for several years [2].
Breech presentation is found in 3% to 4% of term single pregnancy [3]. A large proportion of women with breech presentation undergo cesarean section that leads to repeat surgery at following pregnancy in many cases. External cephalic version (ECV) is a procedure to change a fetal presentation from breech to cephalic by external pressure that obstetricians exert through maternal abdominal wall. In the American College of Obstetricians and Gynecologists practice bulletin, ECV for all pregnant women with singleton and breech presentation at term has been recommended [4]. Women, who once achieve cephalic presentation through ECV, have higher chance for vaginal delivery than they remained breech presentation. In some countries including Korea, however, ECV is an unfamiliar procedure and until now, there are only few skilled physicians. This article is aimed to report the results of ECV performed near or at term and obstetric outcomes after successful ECV in a hospital in Korea.
This retrospective study was performed between November 2009 and July 2014 at Chung-Ang University Hospital. The healthy women with uncomplicated breech presentation near or at term (≥36 weeks) were considered as suitable candidates for ECV. However, some women with 35 completed weeks of gestation were exceptionally included because of their personal reasons. Basic information was gathered including the women's age, parity, height, weight and history of prior uterine operation. Fetal weight and position, amniotic fluid index, placental location, breech type, presence of cord neck, and engagement status were checked with ultrasonography. Electric fetal monitoring was performed to confirm fetal well-being.
Our exclusion criteria were history of prior uterine operation, multiple pregnancy, intrauterine growth restriction, abnormal amniotic fluid (deepest vertical pocket ≤1 cm), placenta previa, premature rupture of membrane and non-reassuring fetal monitoring.
The candidates of ECV agreed to undergo the procedure after they were informed about the failure probability and risk of the procedure including fetal distress and emergency cesarean delivery. Before the procedure, the women were prepared for emergency surgery; they ensured all the tests necessary for anesthesia and maintained fasting state.
ECV was performed by a single obstetrician at labor unit of our hospital. The subjects were placed in supine position. Electric fetal monitoring and ultrasonography were checked before and after the ECV to verify fetal condition, including presentation during procedure, fetal condition and position was checked with real time ultrasonography. Intravenous ritodrine was infused as tocolytics when uterus was too hard to rotate the fetus. The performer's one hand push fetal buttock toward maternal head and the other hand pull the fetal head downward. Fig. 1 shows counterclockwise version. During the procedure, if fetal bradycardia was detected, the procedure was stopped until fetal heart rate was recovered.
If the fetal head was placed in the maternal pelvis after the procedure, the procedure was considered as successful. After confirmation of fetal condition with electric fetal monitoring and ultrasonography, patients were discharged. The delivery outcomes of each patient undergoing ECV such as weight and gender of the baby, delivery mode (vaginal or cesarean) and gestational age at delivery were collected by direct phone call with patients.
All statistical analysis including baseline characteristics was done with IBM SPSS ver. 22.0 (IBM Corp., Armonk, NY, USA). Differences of variables between groups were evaluated with t-test for continuous variables and χ2 test for categorical variables. Factor influencing success and failure of ECV was analyzed using multiple logistic regression analysis implemented in the software. Significance level of 0.05 was used to reject null hypothesis.
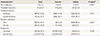
In a total of 145 trials of ECV, 103 (71.0%) changed to cephalic presentation and 42 (28.9%) remained in their initial state. Table 1 describes maternal baseline characteristics of the total, successful and failed ECV groups. Mean maternal age was 31.1 years in total, 31.3 years in successful and 30.6 years in failed group. The mean gestational age was 36.9 weeks, 36+6 weeks and 37+0 weeks in total, success and failed group, respectively. The most of women was 36 weeks (n=59, 40.6%) and 37 weeks of gestational age (n=60, 41.3%). The proportion of multiparous women was higher in successful group than in failed group. The women in successful group were tall and lean than those in failed group. Ultrasonographic findings are delineated in Table 2. As compared with women in failed group, those in succeeded group had higher amniotic fluid index (AFI) value, lower ratio of anterior position of fetal spine and higher ratio of anterior placentation and engagement. ECV was tried 1.8 times on an average per women, and the mean time required was 14.06 minutes; more trials and time was necessary for the procedure in failed group (Table 3). The difference in each value between succeeded and failed group was statistically significant in parity, fetal spine position, number of attempts and the necessary time for ECV and tocolytics usage (<0.05).
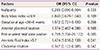
We evaluated the variables including maternal parity (nullior multi-paras) and body mass index, AFI, placental location (anterior or other), fetal spine position (anterior and other), gestational age and rotational direction in ECV, which determined the success or failure of ECV. As a result of multiple logistic regression analysis, four factors (parity, AFI, fetal spine position and rotational direction) were found to affect the success or failure of ECV (<0.05). Success rate was lower in women with nullipara, low AFI, anterior position of fetal spine and clockwise rotation group (Table 4).
The delivery information about 83 women, who experienced successful ECV, was obtained. There was no revision to breech presentation till labor. Sixty eight women (81.9%) had vaginal deliveries, whereas 15 (18.1%) had intrapartum cesarean section. Most common causes of intrapartum cesarean delivery were progress failure and fetal distress. All 39 failed ECV women, whose delivery information was accessible, had elective cesarean delivery. Temporary bradycardia was found in 25 fetuses (17.2%) during the procedure and was recovered with minutes (Table 3). A woman suffered vaginal bleeding after failed ECV. She was hospitalized overnight for observation, and discharged uneventfully the following day without any treatment. She delivered a healthy baby by elective cesarean section. Two women underwent emergent cesarean delivery due to nonreassuring cardiotocogram and labor progression after failed ECV; the newborns were healthy. The first woman had successful ECV at 35+5 weeks of gestation. After the procedure, prolonged deceleration was observed. She underwent emergent cesarean delivery and her baby was admitted to neonatal intensive care unit (Apgar score 4, 7). The other woman with 36+6 weeks of gestational age had failed ECV. After the confirmation of nonreassuring cardiotocogram, the baby was delivered by emergent cesarean section. The baby was healthy (Apgar score 9, 9). There were no other fatal feto-maternal complications after ECV.
According to the American College of Obstetricians and Gynecologists guideline, candidates for ECV are women at or after 36 weeks of gestation. ECV was usually tried before term until mid-1970s because of higher chance of success [5]. After severe perinatal mortality was reported in 1975, the frequency of preterm ECV has been reduced and term ECV became common [6]. ECV could be successfully accomplished even at term with the aid of tocolytic medication that makes the uterus soft. Term ECV has several advantages including low probability of spontaneous rotation to cephalic presentation or reversion after successful ECV; the fetus could be delivered in matured state even in the case of complications during or after the procedure. Hofmeyr and Kulier [7], compared late (≥39 weeks) with early (36 to 38 weeks) ECV and concluded that there was no difference in success rate and mode of delivery between the two groups. Following the references, we tried ECV after 36 completed weeks of gestation.
Success rates of ECV have been reported from 35% to 86% [4] and the result in the present study (71%) is compatible with the reported values. Multipara, higher AFI, non-anterior position of fetal spine and counterclockwise rotational direction had positive correlation with successful ECV. Researchers have worked on figuring out predictors of successful ECV. Multipara is a known favorable factor. In addition, higher AFI seems to have positive correlation with successful ECV [8], despite the presence of contradictory result [9].
Anterior position of fetal spine has been reported to have positive or neutral effect on successful ECV [3], but it was a negative predictor in our case. We thought, in prone position, the fetus resist against the force of version standing with his limbs on the posterior part of uterus. We could not find any reference to correlation between rotational direction and success rate of ECV. Rotational direction was determined mainly according to the direction of fetal face; a right-faced fetus was attempted to rotate in a counterclockwise direction and a left-faced fetus was attempted to rotate in another way. During the procedure, physician's one hand pushes the fetal buttock toward maternal head and the other hand pulls the fetal head following rotational direction. The hand pushing the fetal buttock is important in the procedure that is right hand in counterclockwise rotation. The physician doing the procedure in our institute is right-hander, who handles his right hand skillfully than the other; we presume it as the reason why counterclockwise rotation group had higher success rate of ECV. Estimated fetal weight and birth weight are factors affect the outcome of ECV [101112]. In our study, estimated fetal weight and birth weight were not gained and it is our weakness.
Intrapartum cesarean delivery rate of the women having successful ECV seems to be higher than the women with spontaneous cephalic presentation [51314151617]. In a recent meta-analysis, the overall cesarean delivery rate was 20.7% versus 10.9% in pregnancies after successful ECV and with spontaneous cephalic presentation, respectively; pooled relative risk and 95% confidence interval was 2.2 (1.7 to 2.8) [17]. In the present case, intrapartum cesarean delivery rate after successful ECV was 18.1%, and was comparable with the reported values; but our study lacked a control group for comparative analysis. We found two reports about intrapartum cesarean delivery rate in nulliparas in Korea [1819]. The subjects were term pregnant women having singleton vertex fetus without any pregnancy complications or history of uterine surgery, which were very similar to the inclusion criteria in this study. Observed intrapartum cesarean delivery rates were 12.6% and 9.4%, respectively. In our study, intrapartum cesarean delivery rate in nulliparas was 29.9%. Although direct comparison was not possible, we guardedly agreed previous opinion that cesarean delivery risk after successful EVC exceeds that of spontaneous cephalic presentation.
Substantial discordances between previously accounted intrapartum cesarean delivery rates after successful ECV have been reported to range from 8% to 31% [17]. The influencing factors included different policies on deciding cesarean delivery during labor at each hospital. Additionally, we presume that another contributor is an uneven admixture of nulliparas and multiparas in study populations. In our study, intrapartum cesarean delivery rates after successful ECV were 28.9% in nulliparas and 5.3% in multiparas. To the best of our knowledge, only two previous studies have considered intrapartum cesarean delivery rate after successful ECV by parity [1320]. The study reported intrapartum cesarean delivery rates after successful ECV as 32.0% and 29.8% in nulliparas and 7.4% and 15.9% in multiparas, respectively. Generally, intrapartum cesarean delivery rates after successful ECV are different between nulliparas and multiparas; cesarean delivery rate of a population is dependent on the ratio of the nulliparas and multiparas. Therefore, we propose separate description of intrapartum cesarean delivery rate by parity.
In conclusion, ECV is a useful procedure that could reduce cesarean delivery rate and is safe for pregnant women and her fetus. Therefore, ECV is worth a try to single pregnant women with breech presentation at or near term period.
Figures and Tables
Fig. 1
Counterclockwise external cephalic version. In case of engaged fetus, each hand takes one fetal pole and fetal buttocks pushed out of the maternal pelvis. Fetal head gently pushed toward direction of fetal face, counterclockwise in this figure.
References
1. Centers for Disease Control and Prevention. Births: method of delivery [Internet]. Atlanta (GA): Centers for Disease Control and Prevention;c2015. cited 2015 July 17. Available from: http://www.cdc.gov/nchs/fastats/delivery.htm.
2. Chung SH, Seol HJ, Choi YS, Oh SY, Kim A, Bae CW. Changes in the cesarean section rate in Korea (1982-2012) and a review of the associated factors. J Korean Med Sci. 2014; 29:1341–1352.
3. Kok M, Cnossen J, Gravendeel L, Van Der Post JA, Mol BW. Ultrasound factors to predict the outcome of external cephalic version: a meta-analysis. Ultrasound Obstet Gynecol. 2009; 33:76–84.
4. Committee on. Gynecology, American College of Obstetrics and Gynecologists. External cephalic version. Int J Gynaecol Obstet. 2001; 72:198–204.
5. Chan LY, Tang JL, Tsoi KF, Fok WY, Chan LW, Lau TK. Intrapartum cesarean delivery after successful external cephalic version: a meta-analysis. Obstet Gynecol. 2004; 104:155–160.
6. Bradley-Watson PJ. The decreasing value of external cephalic version in modern obstetric practice. Am J Obstet Gynecol. 1975; 123:237–240.
7. Hofmeyr GJ, Kulier R. External cephalic version for breech presentation at term. Cochrane Database Syst Rev. 2012; 10:CD000083.
8. Boucher M, Bujold E, Marquette GP, Vezina Y. The relationship between amniotic fluid index and successful external cephalic version: a 14-year experience. Am J Obstet Gynecol. 2003; 189:751–754.
9. Newman RB, Peacock BS, VanDorsten JP, Hunt HH. Predicting success of external cephalic version. Am J Obstet Gynecol. 1993; 169(2 Pt 1):245–249.
10. Kok M, van der Steeg JW, van der Post JA, Mol BW. Prediction of success of external cephalic version after 36 weeks. Am J Perinatol. 2011; 28:103–110.
11. Burgos J, Melchor JC, Cobos P, Centeno M, Pijoan JI, Fernandez-Llebrez L, et al. Does fetal weight estimated by ultrasound really affect the success rate of external cephalic version? Acta Obstet Gynecol Scand. 2009; 88:1101–1106.
12. Kirkinen P, Ylostalo P. Ultrasonic examination before external version of breech presentation. Gynecol Obstet Invest. 1982; 13:90–97.
13. Vezina Y, Bujold E, Varin J, Marquette GP, Boucher M. Cesarean delivery after successful external cephalic version of breech presentation at term: a comparative study. Am J Obstet Gynecol. 2004; 190:763–768.
14. Chan LY, Leung TY, Fok WY, Chan LW, Lau TK. High incidence of obstetric interventions after successful external cephalic version. BJOG. 2002; 109:627–631.
15. Kuppens SM, Hutton EK, Hasaart TH, Aichi N, Wijnen HA, Pop VJ. Mode of delivery following successful external cephalic version: comparison with spontaneous cephalic presentations at delivery. J Obstet Gynaecol Can. 2013; 35:883–888.
16. Lau TK, Lo KW, Rogers M. Pregnancy outcome after successful external cephalic version for breech presentation at term. Am J Obstet Gynecol. 1997; 176(1 Pt 1):218–223.
17. de Hundt M, Velzel J, de Groot CJ, Mol BW, Kok M. Mode of delivery after successful external cephalic version: a systematic review and meta-analysis. Obstet Gynecol. 2014; 123:1327–1334.
18. Jeong EH, Park KH, Ryu A, Oh KJ, Lee SY, Kim A. Clinical and sonographic parameters at mid-trimester and the risk of cesarean delivery in low-risk nulliparas. J Clin Ultrasound. 2014; 07. 12. DOI: 10.1002/jcu.22212.
19. Kim SN, Park KH, Jung HJ, Hong JS, Shin DM, Kang WS. Clinical and sonographic parameters at 37 weeks' gestation for predicting the risk of primary cesarean delivery in nulliparous women. Ultrasound Obstet Gynecol. 2010; 36:486–492.
20. Clock C, Kurtzman J, White J, Chung JH. Cesarean risk after successful external cephalic version: a matched, retrospective analysis. J Perinatol. 2009; 29:96–100.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download