Abstract
We present a case of complete vaginal stenosis in a woman diagnosed with Sheehan’s syndrome. The patient delivered at full-term 5 months prior, and experienced massive postpartum bleeding at that time. During evaluation of persistent amenorrhea, we found that her vaginal orifice was completely adhesive and obstructed. Prior to corrective surgery, we managed the patient with an oral contraceptive to induce uterine bleeding into the vaginal outflow tract. After three cycles of an oral contraceptive, we could confirm that there was no stenotic lesion in the vaginal cavity as a hematocolpos was created. Adhesiolysis with scar revision for the vaginal stenosis was successfully performed; it was found that the lesion was limited to only the distal part of the vaginal outlet. Complete vaginal stenosis in reproductive age women with hypopituitarism has not been reported. The artificial induction of hematometrocolpos before surgery was useful in determining the extent of the stenotic lesion, and assured safety.
Sheehan’s syndrome is a rare complication caused by a massive hemorrhagic event, and obstetric postpartum bleeding is a well-known cause of this condition. This syndrome is characterized by a hypopituitary state secondarily caused by ischemic pituitary infarction, and clinically presents with varied symptoms related to multiple hormonal deficiencies [1].
The prevalence is estimated at 100 to 200 per 1,000,000 women by Sheehan who first described the entity [2]. Sheehan’s syndrome represents a lack of multiple pituitary hormones, including growth hormone, thyroid stimulating hormone, and gonadotropins, due to pituitary dysfunction. Clinical symptoms of Sheehan’s syndrome include generalized fatigue, hypoglycemia, hypothyroidism, and other laboratory abnormalities. In addition to general symptoms, gynecologic symptoms commonly include a failure of lactation, persistent amenorrhea, or oligomenorrhea [3].
We present a case of complete stenosis of the vaginal introitus that developed in a patient with Sheehan’s syndrome. The patient underwent surgical vaginoplasty after the induction of artificial hematometrocolpos.
A 37-year-old para 1 patient was admitted to the endocrinology department in our hospital for symptoms of general fatigue and arthralgias. The patient was referred because of persistent amenorrhea and difficulty in sexual activity. The patient vaginally delivered a female infant at 38 weeks of gestation at a private clinic five months prior. She had no other past medical history at that time.
At the initial examination, her serum hormone levels were comparable with hypopituitarism; sex steroid hormones were decreased, with estradiol less than 10.0 pg/mL and testosterone <0.1 ng/mL. Luteinizing hormone and follicle-stimulating hormone were 2.69 and 9.24 mIU/mL, respectively. Free T4 was decreased at 0.02 (normal reference range, 0.7 to 1.86 ng/mL), and thyroid stimulating hormone was 2.06 (normal reference range, 0.17 to 4.05 uIU/mL). In a timed pituitary function test, levels of three hormones did not significantly increase over minutes: corticotropin 1.5, 5.5, 8.5, 5.4, 5.5 pg/mL; cortisol 13, 13.3, 14.3, 13.7, 13.6 ug/mL; growth hormone 0.04, 0.21, 0.26, 0.17, 0.23 ng/mL. A minor factor, hyponatremia (Na 118 mmol/L; normal reference range, 135 to 145 mmol/L) was also observed. With the impression of hypopituitarism caused by postpartum bleeding, magnetic resonance imaging was performed and showed a marked decrease of pituitary gland size for age suspicious for atrophy (Fig. 1).
At gynecologic examination, the vaginal introitus was completely stenotic with fibrotic changes. Therefore, the inner vaginal cavity and uterine cervix could not be examined. Transabdominal ultrasound showed that the uterus was 73×39 mm in size, and bilateral ovaries were identified.
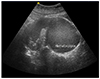
Since the patient was sexually active and complained of amenorrhea, we planned adhesiolysis and scar revision to relieve the stenotic area of the vagina. However, since we could not determine whether there were adhesions or stenosis inside the vaginal cavity, we managed the patient with an oral contraceptive (OC) to induce cyclic uterine bleeding into the vaginal cavity prior to surgery. While on the OC, the patient reported cyclic lower abdominal discomfort. After three cycles of the OC, a transabdominal and transperineal ultrasound showed a dilated uterine cavity with blood clots, along with a hematocolpos measuring 84×66 mm (Fig. 2). The distance from the distal margin of the hematocolpos to the vaginal introitus on ultrasound was thin as it measured at 5 mm; this finding implied the stenotic lesion was limited to the level of the vaginal orifice.
Under general anesthesia, adhesiolysis and scar revision of the vagina were performed. A vertical incision was made at the blind orifice of the vagina with a scalpel, and blood clots it measuring about 200 mL flowed out through the opening. After removing all blood clots and washing the vaginal cavity, we found that the vaginal wall and mucosa were intact and not involved. We removed tense fibrotic tissues around the vaginal orifice, and then the vaginal wall and perineal skin were approximated. The patient has been managed with a topical estrogen cream and use of a vaginal mold to prevent re-stenosis or narrowing of the vagina.
Hypopituitarism occurs as a result of ischemic necrosis of the pituitary and is mainly related to massive postpartum uterine bleeding. The clinical manifestations of this condition are varied and may be non-specific, while persistent amenorrhea and decreased lactation due to gonadotropin deficiency are known to be common gynecologic symptoms [123]. Our patient complained of amenorrhea and difficulty in sexual activity, and a finding of complete stenosis of the vaginal introitus and total obstruction of the vaginal outlet were noted on initial examination.
It was difficult to explain the causative factors for vaginal stricture and stenosis seen in our patient. A search of Medline did not find a case of vaginal stenosis complicated by Sheehan’s syndrome, but there was an unusual case of vaginal synechiae in a menopausal woman who had severe atrophic vaginitis [4]. Estrogen is believed to largely affect the female genital organs, as it maintains elasticity and rich collagen production in the vaginal tissues and has a moisturizing effect in the vagina. Hence, the decrease of estrogen production in menopause induces the breakdown of collagen in the supporting vaginal epithelium and increases vaginal pH by reduction of lactic acid production; these frequently provoke many bothersome genitourinary symptoms during menopause.
In line with genital aging related to estrogen loss, we might surmise that hypoestrogenism accompanied by Sheehan’s syndrome caused an acute atrophic change of the vagina and subsequently contributed to the stenosis of the vaginal orifice in our case. In addition, since our patient presented a few months after the postpartum period, a process of wound healing and scar formation of the episiotomy repair may have been major factor promoting adhesions around the vaginal orifice in addition to atrophic change in the vagina.
We planned corrective surgery to relieve the vaginal outlet obstruction and permit sexual activity. At the initial examination, we could not determine the internal condition of the vaginal cavity beyond the orifice. Artificial induction of hematocolpos by use of an OC in our patient was clinically useful and enabled confirmation of the level and extent of the obstruction of the vagina. In fact, this was similar to the clinical management of some gynecologic conditions. In cases suspicious for congenital vaginal obstruction, surgery frequently needs to be delayed until menarche. Thereafter, creation of hematocolpos can aid in making a definitive diagnosis and facilitate choice of the correct procedure [5]. Since our patient had no natural menstruation due to hypopituitarism, we decided to use a cyclic OC to artificially induce uterine bleeding and hematocolpos.
Although there has been no report on Sheehan’s syndrome producing vaginal stenosis, our case suggests that hypopituitarism secondary to postpartum bleeding could cause a vaginal stricture or adhesions. The method we used to induce a hematocolpos was beneficial for localization of the stenotic lesion and enabled safe surgery without operative complications.
Figures and Tables
References
1. Schrager S, Sabo L. Sheehan syndrome: a rare complication of postpartum hemorrhage. J Am Board Fam Pract. 2001; 14:389–391.
2. Sheehan HL. The frequency of post-partum hypopituitarism. J Obstet Gynaecol Br Commonw. 1965; 72:103–111.
3. Tessnow AH, Wilson JD. The changing face of Sheehan’s syndrome. Am J Med Sci. 2010; 340:402–406.
4. Segal S, Harvie HS, Siegelman E, Arya LA. Severe atrophic vaginitis causing vaginal synechiae and hematocolpos at menopause. Menopause. 2011; 18:333–335.
5. Shaked O, Tepper R, Klein Z, Beyth Y. Hydrometrocolpos: diagnostic and therapeutic dilemmas. J Pediatr Adolesc Gynecol. 2008; 21:317–321.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download