Abstract
Objective
Vesicovaginal fistula (VVF) causes detrimental psychosomatic effects on a woman. It is repaired using open abdominal as well as laparoscopic approach. Here we compare a series of open versus laparoscopic VVF repairs done at a single centre.
Methods
Retrospectively data of patients undergoing VVF repair in our department between January 2011 to December 2014 was analyzed. Patients who had a single, primary, simple VVF following a gynaecological surgery were included in the study. 26 patients met all the criteria. Out of these, thirteen patients had undergone a laparoscopic VVF repair (group 1) while thirteen had undergone an open transabdominal VVF repair (group 2).
Results
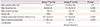
Mean fistula size was 2.14±0.23 cm in group 1 and 2.18±0.30 cm in group 2, which was comparable. Mean blood loss was 58.69±6.48 mL in group 1 and 147.30±19.24 mL in group 2, which is statistically significant (P<0.0001). Mean hospital stay was 4 days in group 1 and 13 days in group 2 which is statistically significant (P<0.0001). The analgesic requirement (diclofenac) was 261.53±29.95 mg in group 1 and 617.30±34.43 mg in group 2, which is statistically significant (P<0.0001). Fistula repair was successful in all the patients in both the groups.
Vesicovaginal fistula (VVF) is a devastating and debilitating condition for all women. Due to continuous urinary leakage and smell of urine, the women becomes a social outcast. It is the most common type of urogenital fistula. In developed countries it is most commonly caused by an abdominal hysterectomy, while in developing countries poor obstetric care is the leading cause of VVF [12].
Various approaches of VVF repair have been described and these can be performed either by an abdominal or vaginal route. The abdominal route is preferred in recurrent fistulas, radiation fistulas, small capacity bladder requiring augmentation, associated ureteric injury requiring reimplantation and high up supratrigonal fistulas [34]. Although the abdominal approach provides a durable result, it is more morbid as compared to vaginal repair [1]. With the use of laparoscopy for VVF repair, this disadvantage can be overcome. Here we present our comparative analysis of laparoscopic versus open VVF repair.
We retrospectively reviewed the data of patients who underwent VVF repair at our department from January 2011 to December 2014. VVF which were caused by gynaecological surgery were included in our study. Patients with recurrent fistula, VVF with a concomitant ureterovaginal fistula, VVF due to obstructed labour and multiple fistulas were excluded from analysis. All patients had undergone gynaecological surgery for benign diseases. Detailed history and physical examination including pelvic and per-speculum vaginal examination findings were noted from the hospital records. Patients generally had a history of urinary drainage per vagina after a gynaecological surgery. All the patients had urine routine examination and culture, renal function test, abdominal ultrasonography, intravenous urography (to rule out ureterovaginal fistula), and cystourethroscopy and vaginoscopy to assess the site, number, size of the fistula, proximity to ureteric orifices or bladder neck for the feasibility of a transvaginal repair. Patients who could not be operated through the vaginal route due to reasons like high up supratrigonal fistula, narrow vagina etc, underwent repair by an abdominal route and were included in this study. There were twenty patients who underwent laparoscopic VVF repair (group 1) and thirty-one who had open VVF repair (group 2) during this period. In laparoscopic group (group 1), seven patients were excluded as three had a concomitant ureterovaginal fistula repair, two had multiple fistulas, one was a recurrent fistula and one patient was lost to follow up. In open group (group 2) eighteen patients were excluded as fifteen had obstructed labour as a cause, two patients had recurrent VVF repair and one was lost to follow-up.
The patient was placed in a low lithotomy position with access to the vagina in the sterile operative field. The abdomen was opened by a lower midline incision. All the patients were approached through transperitoneal route. Adhesions, if present between the bladder, bowel, or vaginal cuff were lysed. The bladder was opened vertically, and the cystotomy was extended down to the fistula. Bilateral ureteric orifices were identified and confirmed by inserting 6fr infant feeding tube through both the ureteric orifices. The plane between the bladder and the vagina was developed, and the fistulous tract was excised. The anterior vaginal wall was repaired with 2-0 polyethylglycol interrupted stitches. Omental flap was interposed between the bladder and vagina from above. The bladder was repaired in two layers in a continuous manner with 3-0 polyglactin suture over 20 Fr supra-pubic and 16 Fr Foley’s urethral catheters. An abdominal drain was placed in the pelvis and the abdomen was closed in layers. Postoperatively patients were put on analgesics, antibiotics and anticholinergics. The drain was removed when the output was less than 50 mL in 24 hours. The abdominal sutures were removed after 8-10 days postoperatively. Due to concerns regarding wound infection and their management, patients were discharged only after abdominal suture removal i.e., after 10 days, if their surgical scar was healthy. The suprapubic catheter was removed at 3 weeks postoperatively. It was removed after 3 weeks as there was bivalving of urinary bladder leading to a large surgical incision on urinary bladder, which takes time to heal. Seven days after the removal of suprapubic catheter, per urethral catheter was removed and a micturating cystourethrogram was performed in all the patients to look for contrast extravasation. In patients with contrast extravasation, per urethral foleys catheter was reinserted and removed after 2 to 3 weeks.
Under general anesthesia, the patient was first placed in lithotomy position. Cystoscopy was performed and ureteric catheters were placed bilaterally. A different coloured ureteric catheter was placed through the fistulous tract from the bladder and brought out off the vagina for easy identification of fistula. A 20 Fr Foley catheter was placed and both ureteric catheters were secured to it. The vagina was packed with vaseline soaked gauze to prevent leakage during bladder filling and escape of CO2 during laparoscopy. Then the patient was placed in supine position with 15 to 30 degrees Trendelenburg tilt. Initial 10 mm trocar was placed at the infra-umbilical site by open method. Two working ports, 10 mm at right iliac fossa and 5 mm at left iliac fossa over the spino-umbilical line were placed under vision following the creation of pneumoperitoneum. Another 5 mm trocar was placed in lower abdomen according to the requirement. After adhesiolysis bladder was filled with about 200 to 250 mL saline to see the outline. Near midline, a limited cystotomy of about 2 cm was performed just above the vaginal vault. Then the fistula was identified by the different colored ureteric catheter/guidewire. The cystotomy was then extended up to the fistula. A plane was created between bladder and vagina for about 1 to 1.5 cm all around the fistulous opening. Vaginal opening was repaired with 2-0 polyglactin in a single layer continuous manner placing the suture line horizontally. The repair was augmented with either omentum or epiploic appendix of sigmoid colon according to availability. Cystotomy was closed with 2-0 polyglactin suture in a single layer continuous manner in a vertical orientation to get a non-overlapping suture line with respect to the vaginal suture line. Then the bladder was filled with about 150 mL of saline mixed with methylene blue to assess watertight repair. Interrupted sutures with 2-0 polyglactin were taken according to the necessity where the leak was identified. An 18 Fr Ryle’s tube was kept in the pelvis as a drain. No suprapubic catheter was placed. The 10mm trocars sites were closed with 2-0 polyglactin. Oral liquids were allowed in the evening of the surgery according to the patient’s tolerance. Oral anticholinergics were given till the removal of Foleys catheter. Patients were ambulated from postoperative day 1. Ureteral catheters were removed 48hrs after surgery. The drain was removed once the output was below 50 mL/day. Patients were discharged after removal of the drain i.e., generally 3rd or 4th postoperative day. Per urethral catheter was removed on the 10th postoperative day, following a cystogram, if there was no suspicion of leakage. Per urethral catheter was removed earlier here as there was a limited cystostomy made laproscopically and a small surgical incision, which takes less time to heal.
All patients were followed up postoperatively every 3 months in the first year and every 6 months thereafter. In follow-up, patients had a detailed history and physical examination with emphasis on detecting urinary leakage. If patients had no history, symptoms or signs of urinary leakage they were considered as successful repair.
Demographic and non-parametric outcome variables between groups were assessed using chi-square and Fisher’s exact tests. Unpaired Student’s t-test was used for comparison of parametric data between the two groups. A P<0.05 was considered statistically significant. We used IBM SPSS ver. 20.0 (IBM Corp., Armonk, NY, USA).
There were thirteen patients in both the groups. The demographic profile of our patients is shown in Table 1. VVF patients presented themselves to us after a varying period of 1 month to as long as 10 years after primary surgery. Patients were undertaken for surgery at least 3 months after their primary gynaecological surgery to allow the inflammation to subside. Mean blood loss was 58.69 mL in group 1 while it was 147.30 mL in group 2 which was statistically significant. Mean hospital stay was 4 days in group 1 and 13 days in group 2. The analgesic (diclofenac sodium; Voveran, Novartis, Mumbai, India) requirement was 261.53 mg in group 1 while it was 617.30 mg in group 2 which was statistically significant. Postoperatively, 3 patients in group 1 and 5 in group 2 developed urinary tract infections, which resolved after receiving antibiotics according to urine culture and sensitivity report. Three patients in group 2 developed minor wound infection which resolved with regular dressing. In both groups, there was 100% successful repair. Mean follow-up time ranges from 6 to 30 months (mean 18.7 months). During follow-up no patient had a recurrence.
The basic principles of a successful VVF repair are mobilization of the bladder from the vagina, good exposure of fistulous tract, complete excision of the fistulous tract, closure of vagina and bladder in tension free watertight fashion, the interposition of a healthy well-vascularised flap between bladder and vagina, continuous postoperative bladder drainage [56].
VVF repaired by transvaginal route has minimal morbidity with good results as demonstrated in many series [78]. The abdominal approach is absolutely necessary for patients where additional abdominal procedures are being undertaken like concomitant ureteric injury repair, augmentation cystoplasty due to small capacity bladder often due to radiation. Abdominal approach is preferred in high supratrigonal fistula, previous failed vaginal repair, those with diminished vaginal access due to radiation or narrow vagina although some use vaginal approach also in such situations. The surgeons’ preference and experience also plays a very important role as one generally chooses the approach in which one is well trained [91011].
Transabdominal repair of VVF can be performed either by transvesical transperitoneal or extraperitoneal approaches [1213]. We utilized a transabdominal transvesical approach with limited cystostomy in laparoscopic procedures. This approach was first described as a mini O’ Connor technique by Rizvi et al. [14]. Utilizing this technique one avoids extensive peritoneal mobilization of the bladder and reduces the operative time too.
Interposition grafts have been used in VVF repair as they promote healing by reinforcing suture lines and decrease fistula recurrence. Various types of grafts e.g., greater omentum, tinea epiploicae of the sigmoid colon, the lateral pelvic peritoneum, posterior superior bladder wall flap etc. have been described in the literature. In all our patients repaired by the open method, we interposed omentum between the vagina and urinary bladder. In laparoscopic repair in 4 patients, we used omentum while in 7 patients we used colonic epiploic appendix. Initially, we used colonic epiploicae in 2 cases as the omentum was short in length. But with the successful outcome, we adopted it in rest of the cases. Its advantages are that it lies near the operative field and it reduces the overall operative time where omentum is short and needs mobilization to bring down into the pelvic cavity [1516].
Laparoscopic surgery is beneficial over open surgery as the patient has less postoperative pain and, therefore, lesser analgesic requirements, faster recovery and shorter hospital stay [1718]. All of these advantages of laparoscopic surgery are clearly shown in our study also (Table 2). Laparoscopy is especially useful in pelvic surgeries as it is a difficult area to access via open surgery. Laparoscopy also provides a magnified view of the pelvic area where all structures are close by, which is very helpful in a reconstructive surgery like VVF repair. But one needs fine a dissection skill to manage the fistulous tract. The disadvantage of laparoscopy is that it has a steep learning curve and the surgeon doing laparoscopic VVF repair should be well versed in the technique of intracorporeal suturing.
With the use of Da Vinci Surgical System (Intuitive Surgical, Sunnyvale, CA, USA) a 3-dimensional magnified view and improved range of mobility can be obtained, which is further beneficial for such precise repair [19]. Gupta et al. [20] compared robotic and open VVF repair for recurrent VVF fistula. Both approaches had 100% successful repair of VVF. They reported significantly less blood loss (88 vs. 170 mL) and reduced hospitalization stay (3.1 vs. 5.6 days) of robotic surgery as compared to open surgery [20].
The limitation of our study is that it is a retrospective study. The surgeries were performed by separate surgeons. There are very few studies comparing open and laparoscopic VVF repair. Further randomised studies are needed to compare open and laparoscopic VVF repair.
References
1. Miller EA, Webster GD. Current management of vesicovaginal fistulae. Curr Opin Urol. 2001; 11:417–421.
2. Kumar A, Goyal NK, Das SK, Trivedi S, Dwivedi US, Singh PB. Our experience with genitourinary fistulae. Urol Int. 2009; 82:404–410.
3. Carr LK, Webster GD. Abdominal repair of vesicovaginal fistula. Urology. 1996; 48:10–11.
4. O'Conor VJ Jr, Sokol JK, Bulkley GJ, Nanninga JB. Suprapubic closure of vesicovaginal fistula. J Urol. 1973; 109:51–54.
5. Nezhat CH, Nezhat F, Nezhat C, Rottenberg H. Laparoscopic repair of a vesicovaginal fistula: a case report. Obstet Gynecol. 1994; 83(5 Pt 2):899–901.
6. Ou CS, Huang UC, Tsuang M, Rowbotham R. Laparoscopic repair of vesicovaginal fistula. J Laparoendosc Adv Surg Tech A. 2004; 14:17–21.
7. Singh V, Sinha RJ, Sankhwar SN, Sinha SM, Vatsal P, Jain V. Transvaginal repair of complex and complicated vesicovaginal fistulae. Int J Gynaecol Obstet. 2011; 114:51–55.
8. Wang Y, Hadley HR. Nondelayed transvaginal repair of high lying vesicovaginal fistula. J Urol. 1990; 144:34–36.
9. Angioli R, Penalver M, Muzii L, Mendez L, Mirhashemi R, Bellati F, et al. Guidelines of how to manage vesicovaginal fistula. Crit Rev Oncol Hematol. 2003; 48:295–304.
10. Leng WW, Amundsen CL, McGuire EJ. Management of female genitourinary fistulas: transvesical or transvaginal approach? J Urol. 1998; 160(6 Pt 1):1995–1999.
11. Blaivas JG, Heritz DM, Romanzi LJ. Early versus late repair of vesicovaginal fistulas: vaginal and abdominal approaches. J Urol. 1995; 153:1110–1112.
12. Hanif MS, Saeed K, Sheikh MA. Surgical management of genitourinary fistula. J Pak Med Assoc. 2005; 55:280–284.
13. Romics I, Kelemen Z, Fazakas Z. The diagnosis and management of vesicovaginal fistulae. BJU Int. 2002; 89:764–766.
14. Rizvi SJ, Gupta R, Patel S, Trivedi A, Trivedi P, Modi P. Modified laparoscopic abdominal vesico-vaginal fistula repair: “Mini-O’Conor” vesicotomy. J Laparoendosc Adv Surg Tech A. 2010; 20:13–15.
15. Arrowsmith S, Hamlin EC, Wall LL. Obstructed labor injury complex: obstetric fistula formation and the multifaceted morbidity of maternal birth trauma in the developing world. Obstet Gynecol Surv. 1996; 51:568–574.
16. Raz S, Bregg KJ, Nitti VW, Sussman E. Transvaginal repair of vesicovaginal fistula using a peritoneal flap. J Urol. 1993; 150:56–59.
17. Tiong HY, Shim T, Lee YM, Tan JK. Laparoscopic repair of vesicovaginal fistula. Int Urol Nephrol. 2007; 39:1085–1090.
18. Wong C, Lam PN, Lucente VR. Laparoscopic transabdominal transvesical vesicovaginal fistula repair. J Endourol. 2006; 20:240–243.
19. Hemal AK, Abol-Enein H, Tewari A, Shrivastava A, Shoma AM, Ghoneim MA, et al. Robotic radical cystectomy and urinary diversion in the management of bladder cancer. Urol Clin North Am. 2004; 31:719–729.
20. Gupta NP, Mishra S, Hemal AK, Mishra A, Seth A, Dogra PN. Comparative analysis of outcome between open and robotic surgical repair of recurrent supra-trigonal vesico-vaginal fistula. J Endourol. 2010; 24:1779–1782.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download