Abstract
Objective
The goal of this study was to evaluate the etiologies and clinical outcomes of Korean recurrent pregnancy loss (RPL) patients. And also, we investigated the differences between primary and secondary RPL patients, between two and three or more pregnancy losses.
Methods
One hundred seventy eight women diagnosed as RPL were enrolled. We performed chromosomal analysis, thyroid stimulating hormone, prolactin, blood glucose, plasminogen activator inhibitor-1, natural killer cell proportion, anticardiolipin antibodies, antiphospholipid antibodies, lupus anticoagulant, anti-β2glycoprotein-1 antibodies, antinuclear antibody, protein C, protein S, antithrombin III, homocysteine, MTFHR gene, factor V Leiden mutation, and hysterosalphingography/hysteroscopic evaluation.
Results
The mean age was 34.03±4.30 years, and mean number of miscarriages was 2.69±1.11 (range, 2 to 11). Anatomical cause (13.5%), chromosomal abnormalities (5.6%), and endocrine disorders (34.3%) were observed in RPL women. Elevated natural killer cell and antiphospholipid antibodies were observed in 43.3% and 7.3% each. Among of 178 women, 77 women were pregnant. After management of those women, live birth rate was 84.4% and mean gestational weeks was 37.63±5.12. Women with three or more RPL compared with women with two RPL had more common anatomical cause such as intrauterine adhesions and lower rates of spontaneous pregnancy. Compare with secondary RPL women, immunological abnormalities were more common in primary RPL. However, miscarriage rates were not different.
Conclusion
Immunological factor including autoimmune and alloimmune disorders was most common etiology of RPL. Inherited thrombophilia showed different patterns with other ethnic countries. Miscarriage rates were not different between primary and secondary RPL, or between two and three or more miscarriages group.
Recurrent pregnancy loss (RPL) is a frustrating, bitter experience to hopeful parents, estimated to occur in 2% to 4% for reproductive age couples [1]. PRL has been defined as three or more spontaneous pregnancy losses. In cases of female partner age over 35 years, history of infertility, normal karyotype on products of conception and embryonic heart activity observed in previous miscarriage, the investigation of causes of RPL have also been recommended even in women with two miscarriages. Nowadays, American Society for Reproductive Medicine proposes two more miscarriages as the RPL definition considering delayed pregnancy trial and late marital age [2]. However, European Society of Human Reproduction and Embryology maintains the definition of RPL as three or more miscarriages were happened. As an important public health concern, RPL may evoke physical and psychological traumas to pregnant women. Moreover, the risk of miscarriage in a subsequent pregnancy increases with the number of previous miscarriages [3]. There are still many debates regarding the diagnostic and treatment options. Various etiologies have been proposed including chromosomal abnormalities, uterine abnormalities, endocrine disease, autoimmune disease, alloimmune abnormalities, thrombophilia and infection. Despite extensive evaluation, 30% to 40% of cases of RPL remained unexplained [45]. Immune responses in maternal-fetal interface are important for survival of semi-allogenic fetus. Regarding the alloimmune tolerance, human leukocyte antigens, natural killer cells, TH1/TH2 cell imbalance, TH17 cells, regulatory T cells, macrophages and chemotactic factors have been investigated. Antiphospholid antibodies have been associated with RPL and other obstetric complications as thrombophilic disease [6]. Recently, there are many studies about the inherited thrombophilia such as factor V Leiden mutation [5], prothrombin gene mutation [3], plasminogen activator inhibitor-1 (PAI-1) gene polymorphism [7], methylenetetrahydrofolate reductase (MTHFR) polymorphism [89], protein S deficiency, protein C deficiency [10]. However, the results were inconsistent and also ethnical differences were existed [11]. The guideline for evaluation and management for RPL women based on the evidence and our circumstances is urgently needed. The goal of this study was to evaluate the etiologies and clinical outcomes of Korean RPL patients. And also, we investigated the differences between primary and secondary RPL patients, between two and three or more pregnancy losses.
One hundred seventy eight women were enrolled after two or more miscarriages, who visited the RPL clinic at Dongsan Medical Center for last three years. Among them, 79 women had three or more miscarriages and 99 women had two miscarriages. One hundred forty five women suffered miscarriages without any live births were classified as primary RPL group, and compared with secondary RPL women. This prospective cohort study was approved by the University Institutional Review Board. All of the study populations were tested for chromosomal analysis, thyroid stimulating hormone (TSH), prolactin, blood glucose, PAI-1, natural killer (NK) cell proportion, anticardiolipin antibodies IgM/G, antiphospholipid antibodies IgM/G, lupus anticoagulant, anti-β2 glycoprotein-1 antibodies IgM/G, antinuclear antibody (ANA), protein C activity, protein S activity, antithrombin III activity, homocysteine, MTFHR gene polymorphism (C677G), factor V Leiden mutation and hysterosalphingography/or hysteroscopic evaluation. All patients took these tests at least two spontaneous menses after miscarriage. When the antiphospholipid antibodies including anticardiolipin and antiβ2glycoprotein-1 were positive, they were tested again at least 12 weeks apart.
Pregnancy outcomes after enrollment were evaluated. RPL patients were conceived naturally without the assisted reproductive technology such as intrauterine insemination or in-vitro-fertilization. Some patients who complained irregular cycle or anovulation took clomiphen citrate or aromatase inhibitor (Femara, Novartis AG, Stei, Switzerland) and had timed intercourse. RPL women took levothyroxine, bromocriptine, progesterone, low dose aspirin, low molecular weight heparin, steroid, or immunoglobulin as their conditions. Patients with hyperprolactinemia were treated with bromocriptine (Parlodel, Novartis AG, Annunziata, Italy) before pregnancy. Patients with hypothyroidism were treated with (Synthyroid, Bukwang, Ansan, Korea) before pregnancy and during pregnancy with monitoring the serum TSH and free T4 levels. Patients with elevated NK cell proportion were treated with prednisolone (Solondo, Yuhan, Cheongju, Korea) after confirming the urinary human chorionic gonadotropin until 12 gestational weeks with monitoring the NK cell proportion. When it was not controlled, immunoglobulin (400 mg/kg) was administrated every 3 weeks. Patients with antiphospholipid antibodies and thrombotic abnormalities such as protein S deficiencies were treated with low molecular weight heparin (Clexan, Sanofi Winthrop Industrie, le Trait, France; 40 mg) and low dose aspirin during the pregnancy. Most of women had multiple abnormalities, in that cases, combination of medication were applied.
Pregnancy loss was defined as any natural miscarriage occurring before 20 weeks of gestation. Ectopic pregnancy, molar pregnancy and artificial abortion were excluded.
For the statistical analysis, Student's t-test and Mann-Whitney test was performed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA) to determine the differences between primary and secondary RPL, and also between two and three or more miscarriages. For categorical data, Pearson's chi-square test and Fisher's exact test were used. Statistical significance was assumed at P<0.05.
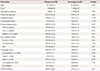
The mean age of RPL patients was 34.03±4.31 years, parity was 0.22±0.49 (range, 0 to 2) and mean number of miscarriages was 2.58±1.21 (range, 2 to 11). Twenty four of 178 women (13.5%) had anatomical cause such as uterine synnechia (14 cases), uterine anomaly (5 cases), endometrial polyp (4 cases), and submucosal myoma (1 case). Chromosomal abnormalities were 9 cases of balanced translocation and one Tuner syndrome, found in 8 women and 2 men among 178 couples (5.6%). Serum TSH was 2.43±1.78 mIU/mL (range, 0.01 to 10.54 mIU/mL), serum prolactin was 15.62±18.87 ng/mL (range, 3.48 to 174.81 ng/mL), fasting insulin levels was 6.96±5.86 µIU/mL (range, 1.44 to 34.13 µIU/mL). Serum PAI-1 was 26.99±21.58 ng/mL (range, 3.40 to 95.83 ng/mL). NK cells proportion was 14.56±7.38% (range, 2.40% to 41.60%). Serum homocysteine was 8.40±2.39 µmol/L (range, 3.85 to 22.99 µmol/L). Protein C activity was 109.13±21.83% (range, 10.705% to 171.00%), protein S activity was 71.52±24.14% (range, 15.00% to 170.00%), anti-thrombin III was 99.05±10.68% (range, 65.00% to 123.00%). Endocrine disorders (34.3%) such as hypothyrodism and hyperprolactinemia, and elevated NK cell proportion (43.3%) were observed. Antiphospholipid antibodies including anticardiolipin IgM/G, antiβ2glycoprotein-1 IgM/G, and lupus anticoagulant were observed in 7.3%. Deficiency of protein S activity was observed in 13.5%, however, deficiency of protein C and antithrombin III were observed only in 0.6% and 1.1% each. Factor V Leiden mutation was not found in any patients. MTFHR gene polymorphism was observed in 35.4% of RPL patients (Table 1).
Forty two women without any abnormal result after evaluation were classified as unexplained RPL (23.6%). Fifty women had single abnormality such as anatomical factor (9 cases), chromosomal factor (2 cases), endocrine factor (hypothyroidism 6 cases and hyperprolactinemia 5 cases), immunological factor (elevated NK cell 14 cases and autoantibodies 2 cases), and thrombotic factor (protein S deficiency 5 cases, hyperho-mocysteinemia 1 case, and MTFHR mutation 6 cases). Eighty six women (48.3%) had multiple abnormalities such as two factors (50 cases), three factors (28 cases) and even four factors (8 cases). The various combinations of etiologies were found.
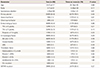
One hundred forty five women (81.5%) had not had a live birth before their miscarriages (primary RPL). The mean age of women with one or more prior live birth (35.45±4.91 years) was greater than that of women who had no prior live births (33.70±4.10 years, P=0.04). The mean parity of secondary RPL was 1.18±0.39. The number of miscarriages of each group were not different (2.66±1.14 for primary RPL and 2.79±0.99 for secondary RPL). Anatomical abnormalities and chromosomal abnormalities were found similarly in both groups. The mean value of TSH, prolactin, fasting insulin, blood glucose were not different between two groups. The incidence of endocrine disorders was similar in both groups. However, immunological abnormalities were more prevalent in primary RPL group compared to secondary RPL group (P=0.01). Elevated NK cell proportion was more common in primary RPL (49.7%) compared to that of secondary RPL (15.2%, P=0.01). Antiphospholipid antibodies and inherited thrombophilias were not different between two groups (Table 2).
Seventy nine women (44.4%) had three or more miscarriages (range, 3 to 11) and 99 women had two miscarriages. The mean age of women with three or more miscarriages was similar with that of women with two miscarriages. The mean parity was not different between two groups either. Women with three or more RPL had more common anatomical abnormalities such as intrauterine adhesions (21.5%) compared to women with two RPL (7.1%, P=0.01). However, mean value of TSH, prolactin, fasting insulin, blood glucose, homocysteine, PAI-1, NK cell proportion, protein C activity, protein S activity, and antithrombin III activity in both groups were similar. Incidence of chromosomal abnormalities, endocrine disorders and immunological abnormalities were not different between two groups (Table 3).
Among of 178 women, seventy seven women were pregnant. After management of those women, live birth rate was 84.4% and mean gestational weeks was 37.63±5.12 weeks. Twelve miscarriages were happened in the enrolled women. In primary RPL women, sixty three women out of 145 were pregnant, and live births were achieved in 51 women (81.0%). Fourteen women out of 33 secondary RPL women were pregnant, and all of them had live births. Secondary RPL women showed better live birth rate compared with primary RPL women, however, statistically insignificant. Delivery weeks of gestation were similar in both groups. Fifty one women with two previous miscarriages (51.5%) and 26 women with three or more miscarriages (32.9%) were pregnant. Compared with three or more RPL women, RPL women with two miscarriages showed higher pregnancy rate (P<0.05). However, Live birth rates of each group were not different. Delivery weeks of gestation were not different either (Table 4).
Repeat pregnancy loss has been public health concern, developed 1 in 300 pregnancies and 2% to 4% of reproductive-aged couples. PRL has been defined as three or more spontaneous pregnancy losses. Nowadays, American Society for Reproductive Medicine proposes two more miscarriages as the RPL definition [2]. The comparison of etiologies or clinical outcomes between women with only two miscarriages and women with three or miscarriages is still scarce [112]. To our acknowledgment, this is the first study with Korean RPL women for comparison of the differences between primary and secondary RPL patients, between two and three or more pregnancy losses.
There is still a lack of consensus regarding the diagnostic and treatment options. However, patients have a strong will to perform diagnostic test and to start treatment despite a lack of solid evidence. Couples suffering RPL experienced emotional stress such as feeling of grief, lower self esteem, guilt, anger, depression and anxiety which persisted for 6 months after miscarriage [13]. Parental chromosome, uterine anatomy, endocrine disorder and antiphospholipid antibodies are undisputed etiology of RPL. However, 30% to 40% of RPL remained unexplained. Immunological imbalance, acquired and inherited thrombophilia have been issued as related with these unexplained RPL.
Only 5.6% of couples had chromosomal abnormalities, but chromosomal analysis must be considered a part of routine investigation. This result was consistent with other studies and fell within the reported range (2.5% to 8%) for women with RPL [11415]. Uterine anatomic defects were found in 13.5%, similar with other reports [115]. Intrauterine adhesion was most common cause, followed by septated uterus. The prevalence of endocrine disorder in our study was 34.3%, higher than other report [4], most likely because of subclinical hypothyroidism. The abnormal level of TSH was defined as more than 2.5 µIU/mL instead of 4 µIU/mL. It has been recommended that the normal range of TSH for pregnancy are modified, and also some advocate using pregnancy thresholds for the treatment of women attempting conception in order to minimize the potential risks associated with subclinical hypothyroidism in pregnancy [1617]. Thyroid hormone replacement with levothyroxine in pregnant women with subclinical hypothyroidism (TSH >2.5 µIU/mL) improved pregnancy outcome [1819]. The prevalence of hypothyroidism using levels of TSH more than 4 µIU/mL was similar with previous reports. Hyperprolactinemia is unique endocrinopathy that cause infertility and miscarriage through anovulation or luteal phase defect. Dopamine agonist like bromocriptine significantly improved subsequent pregnancy outcome in women with RPL and hyperprolactinemia [20]. Women with polycystic ovary syndrome, the most common endocrinopathy of reproductive-aged women, have an increased risk of pregnancy loss. The precise mechanism is unclear but possibly acts through the clotting factor PAI-1 [18]. In the meta-analysis about association between PAI-1 gene polymorphism and RPL, PAI-1-675G/A polymorphism was significantly associated with RPL (odds ratio [OR], 1.70; 95% confidence interval [CI], 1.21 to 2.38). Especially, this association was significant for Asians and Africans but not for American, Europeans, and Oceanians [7]. Management of polycystic ovary syndrome (PCOs) with normalization of weight or metformin seems to reduce the risk of pregnancy loss.
Peripheral blood and peri-implantation endometrial CD56+ NK cells in early pregnancy are intensively studied. Uterine natural killer cells in the endometrium are thought to support remodeling of the uterine spiral arteries and to facilitate successful placentation through the regulation of trophoblast invasion. An abnormal increase of the peripheral blood natural killer cell fraction and NK cytolytic activity is associated with RPL [2122]. Downregulation of NK cells was associated with a favorable pregnancy outcome [23]. However, Immunotherapy for recurrent miscarriages and infertility is still controversial [24]. In our study, elevated peripheral NK cell was found in 77 women (43.3%), most common cause of enrolled RPL women. And also, antiphospholipid antibodies including anticardiolipin antibodies IgM/G, lupus anticoagulant, anti-β2 glycoprotein-1 antibodies IgM/G were found in 13 women (7.3%). Antiphospholipid syndrome (APS) is an autoimmune condition characterized by the production of antiphospholid antibodies combined with clinical features like vascular thrombosis or pregnancy morbidity [25]. The incidence of APS was reported as 15% to 20% in women with RPL [2627], and fetal loss rate of these women was 50% to 90% if no specific treatment was given [6]. In this study, APS was less common than other studies. It is needed further large scale investigation for Korean RPL women. Treatment with heparin and aspirin is emerging as the therapy of choice, with approximately 75% of treated women having a successful live birth [26]. Screening for inherited thrombophilias such as factor V Leiden, prothrombin gene mutations, MTHFR gene polymorphism, protein C deficiencies, protein S deficiencies, and antithrombin deficiencies may have focused on recurrent miscarriages [52829]. Factor V Leiden and prothrombin G20210A mutations are by far the most common of the inherited thrombophilias, present in 8 and 3%, respectively, of the general Caucasian population [130]. Protein S deficiency, protein c deficiency and antithrombin III deficiency were found 3.5%, 1.1%, and 1.5% each [1]. However, in Indian women with RPL, factor V Leiden mutation was found only 3.5% and proteins S deficiency was most common (16%) of the inherited thrombophilia [11]. In our study, factor V Leiden mutation was not found in any women and proteins S deficiency was found 13.5%. The risk of miscarriages related with inherited thrombophilia seems to be controversial. Recently, in meta-analysis, factor V Leiden mutation was associated with RPL (OR, 1.68; 95% CI, 1.16 to 2.44) [5]. A significant association was found between prothrombin mutation and RPL with OR 1.81 (95% CI, 1.26 to 2.60). In subgroup analysis, the pooled OR remained significant in European studies (OR, 1.80; 95% CI, 1.35 to 2.41), whereas it was not significant in the Middle-Eastern studies (OR, 2.39; 95% CI, 0.96 to 5.92) [3]. Inherited thrombophilia has shown the ethnical difference, which signify the need for consideration in screening and interpretation.
Compared to secondary RPL, women without any live birth had almost similar results in the evaluation tests. However, alloimmune abnormalities such as elevated NK cell proportions were more common in primary RPL. Shapira et al. [31] reported the only significant difference in the etiological evaluation was abnormal prolactin levels in the primary RPL. In our study, serum prolactin level and incidence of hyperprolactinemia were not different between two groups. Pregnancy rate and live birth rate were also similar. Miscarriages of index pregnancy tend to be happened in primary RPL group (12 out of 63) compared with none out of 33 in secondary RPL group, statistically insignificant. We believe further study with large scale is needed.
Women with three or more RPL compared to women with two RPL had also similar in the etiological evaluations except anatomical cause such as intrauterine adhesions. It might be related with previous uterine curettage. Bashiri et al. [12] reported women with two miscarriages and three or more miscarriages had very similar in evaluation test results and obstetric characteristics. In our study, pregnancy rate was significantly higher in women with two miscarriages (59.0%) than in women with three or more (33.3%, P=0.01). Live birth rate of each group was not different. Lund et al. [32]. reported the chance of a live birth by increasing number of miscarriages before first consultation was decreased, 70% for women with three miscarriages and 60% for five miscarriages until five years after consultation. Five years after the first consultation, overall cumulative live birth rates was achieved in 66.7% of women with RPL after management with imunoglobulin, steroid, progesterone, heparin, or aspirin [32]. Recently, Lee et al. [33]. reported overall live birth rate in Korean RPL women was 86.8%, regardless of treatment modalities such as low dose aspirin, low molecular weight heparin, or intravenous immunoglobulin. In our study, live birth in the index pregnancy was 84.4%, comparable with other studies. RPL patients have various etiologies, and most of them have multiple abnormalities. In our study, many RPL women were treated with combination of medication as their own conditions. We drew the overall live birth rate after combination of treatment which might be higher than live birth rate after singe treatment in other studies. Comparing primary RPL with secondary RPL, and two miscarriages with three or more, live birth rate of each groups were not different. However, women with secondary RPL might have better live birth rate even though the limited number of cases were not reached to statistical significance. Further longitudinal studies with larger scale are required.
The strength of present study is the prevalence of each etiologies and overall live birth rate in RPL women with primary or secondary, and two or three more miscarriages. We believe this study could be useful to counsel the RPL coupes. However, the limitation of this study was lack of the efficacy of each treatment. To establish the efficacy of each treatment precisely, women with single etiology without any other abnormalities are evaluated by randomized controlled trials. Considering the prevalence of RPL was 1% of general population, multicenter studies or national registration studies are needed.
In conclusion, immunological factor including autoimmune disorders and alloimmune disorders was most common etiology of RPL in our clinic. Inherited thrombophilia showed different patterns compared with other ethnic groups. Nowadays, the guideline for evaluation and management of RPL women based on the evidence and our Korean circumstances is urgently needed. Considering this situation, our data must be useful for counseling the RPL women and establishing the Korean RPL guidelines. Further well designed, large scaled studies are also needed.
Figures and Tables
Table 1
Demographic data and etiologic characteristics in all enrolled women with recurrent pregnancy losses (178 Enrolled women)

Table 2
Comparison of demographic data and etiologic characteristics between primary and secondary recurrent pregnancy loss patients
References
1. Jaslow CR, Carney JL, Kutteh WH. Diagnostic factors identified in 1020 women with two versus three or more recurrent pregnancy losses. Fertil Steril. 2010; 93:1234–1243.
2. Practice Committee of American Society for Reproductive Medicine. Definitions of infertility and recurrent pregnancy loss: a committee opinion. Fertil Steril. 2013; 99:63.
3. Gao H, Tao FB. Prothrombin G20210A mutation is associated with recurrent pregnancy loss: a systematic review and meta-analysis update. Thromb Res. 2015; 135:339–346.
4. Ford HB, Schust DJ. Recurrent pregnancy loss: etiology, diagnosis, and therapy. Rev Obstet Gynecol. 2009; 2:76–83.
5. Sergi C, Al Jishi T, Walker M. Factor V Leiden mutation in women with early recurrent pregnancy loss: a metaanalysis and systematic review of the causal association. Arch Gynecol Obstet. 2015; 291:671–679.
6. Kwak-Kim J, Agcaoili MS, Aleta L, Liao A, Ota K, Dambaeva S, et al. Management of women with recurrent pregnancy losses and antiphospholipid antibody syndrome. Am J Reprod Immunol. 2013; 69:596–607.
7. Chen H, Nie S, Lu M. Association between plasminogen activator inhibitor-1 gene polymorphisms and recurrent pregnancy loss: a systematic review and meta-analysis. Am J Reprod Immunol. 2015; 73:292–300.
8. Yousefian E, Kardi MT, Allahveisi A. Methylenetetrahydrofolate reductase C677T and A1298C polymorphism in Iranian women with idiopathic recurrent pregnancy losses. Iran Red Crescent Med J. 2014; 16:e16763.
9. Kim NK, Choi YK, Kang MS, Choi DH, Cha SH, An MO, et al. Influence of combined methylenetetrahydrofolate reductase (MTHFR) and thymidylate synthase enhancer region (TSER) polymorphisms to plasma homocysteine levels in Korean patients with recurrent spontaneous abortion. Thromb Res. 2006; 117:653–658.
10. Davenport WB, Kutteh WH. Inherited thrombophilias and adverse pregnancy outcomes: a review of screening patterns and recommendations. Obstet Gynecol Clin North Am. 2014; 41:133–144.
11. Patil R, Ghosh K, Vora S, Shetty S. Inherited and acquired thrombophilia in Indian women experiencing unexplained recurrent pregnancy loss. Blood Cells Mol Dis. 2015; 55:200–205.
12. Bashiri A, Ratzon R, Amar S, Serjienko R, Mazor M, Shoham-Vardi I. Two vs. three or more primary recurrent pregnancy losses: are there any differences in epidemiologic characteristics and index pregnancy outcome? J Perinat Med. 2012; 40:365–371.
13. Van den Berg MM, Vissenberg R, Goddijn M. Recurrent miscarriage clinics. Obstet Gynecol Clin North Am. 2014; 41:145–155.
14. Christiansen OB, Nybo Andersen AM, Bosch E, Daya S, Delves PJ, Hviid TV, et al. Evidence-based investigations and treatments of recurrent pregnancy loss. Fertil Steril. 2005; 83:821–839.
15. Stephenson M, Kutteh W. Evaluation and management of recurrent early pregnancy loss. Clin Obstet Gynecol. 2007; 50:132–145.
16. Practice Committee of the American Society for Reproductive
Medicine. Subclinical hypothyroidism in the infertile female population: a guideline. Fertil Steril. 2015; 104:545–553.
17. Yi KH, Kim KW, Yim CH, Jung ED, Chung JH, Chung HK, et al. Guidelines for the diagnosis and management of thyroid disease during pregnancy and postpartum. J Korean Thyroid Assoc. 2014; 7:7–39.
18. Ke RW. Endocrine basis for recurrent pregnancy loss. Obstet Gynecol Clin North Am. 2014; 41:103–112.
19. Reid SM, Middleton P, Cossich MC, Crowther CA, Bain E. Interventions for clinical and subclinical hypothyroidism pre-pregnancy and during pregnancy. Cochrane Database Syst Rev. 2013; (5):CD007752.
20. Hirahara F, Andoh N, Sawai K, Hirabuki T, Uemura T, Minaguchi H. Hyperprolactinemic recurrent miscarriage and results of randomized bromocriptine treatment trials. Fertil Steril. 1998; 7:246–252.
21. Kim YH, Kim YJ, Jeong SO, Cha SH, Choi MH, Yang KM. Changes of natural killer cell number and cytolytic activity during first trimester of pregnancy in recurrent spontaneous abortion patients and fertile control. Korean J Obstet Gynecol. 2012; 55:713–720.
22. Yi HJ, Kim JH, Koo HS, Bae JY, Cha SW, Yang KM. Elevated natural killer cell levels and autoimmunity synergistically decrease uterine blood flow during early pregnancy. Obstet Gynecol Sci. 2014; 57:208–215.
23. Kwak JY, Kwak FM, Ainbinder SW, Ruiz AM, Beer AE. Elevated peripheral blood natural killer cells are effectively downregulated by immunoglobulin G infusion in women with recurrent spontaneous abortions. Am J Reprod Immunol. 1996; 35:363–369.
24. Wong LF, Porter TF, Scott JR. Immunotherapy for recurrent miscarriage. Cochrane Database Syst Rev. 2014; (10):CD000112.
25. Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, Cervera R, et al. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost. 2006; 4:295–306.
26. Kutteh WH, Hinote CD. Antiphospholipid antibody syndrome. Obstet Gynecol Clin North Am. 2014; 41:113–132.
27. Yetman DL, Kutteh WH. Antiphospholipid antibody panels and recurrent pregnancy loss: prevalence of anticardiolipin antibodies compared with other antiphospholipid antibodies. Fertil Steril. 1996; 66:540–546.
28. de Jong PG, Goddijn M, Middeldorp S. Antithrombotic therapy for pregnancy loss. Hum Reprod Update. 2013; 19:656–673.
29. Bennett SA, Bagot CN, Arya R. Pregnancy loss and thrombophilia: the elusive link. Br J Haematol. 2012; 157:529–542.
30. Porter TF, Scott JR. Evidence-based care of recurrent miscarriage. Best Pract Res Clin Obstet Gynaecol. 2005; 19:85–101.
31. Shapira E, Ratzon R, Shoham-Vardi I, Serjienko R, Mazor M, Bashiri A. Primary vs. secondary recurrent pregnancy loss: epidemiological characteristics, etiology, and next pregnancy outcome. J Perinat Med. 2012; 40:389–396.
32. Lund M, Kamper-Jorgensen M, Nielsen HS, Lidegaard O, Andersen AM, Christiansen OB. Prognosis for live birth in women with recurrent miscarriage: what is the best measure of success? Obstet Gynecol. 2012; 119:37–43.
33. Lee SK, Kim JY, Han AR, Hur SE, Kim CJ, Kim TH, et al. Intravenous immunoglobulin G improves pregnancy outcome in women with recurrent pregnancy losses with cellular immune abnormalities. Am J Reprod Immunol. 2016; 75:59–68.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download