Abstract
Heterotopic pregnancy is a rare and life-threatening condition which is defined as coexistent intrauterine and ectopic gestation. The risk of ectopic and heterotopic pregnancy is increasing due to the increased risk of multiple pregnancies with the aid of assisted reproductive technologies. However, it hardly happens in the setting of single embryo transfer, since single embryo transfer significantly reduces the incidence of multiple pregnancies. Surprisingly, we experienced a case of heterotopic pregnancy after a single embryo transfer caused by coincidental natural pregnancy during assisted reproductive technologies. An infertile woman who underwent, during her natural cycle, transfer of a single embryo that had been cryopreserved for 3 years was found to be heterotopically pregnant. After an early and successful management with laparoscopic right salpingectomy, she finally reached at full-term vaginal delivery.
Heterotopic pregnancy (HP) is a rare and fatal condition. Its incidence is known to be one in 8,000 to 30,000 in spontaneous conceptions increasing to a rate of 0.2% to 1% in gestations after assisted reproductive technologies [123]. However, the detection of HP could be neglected in an infertile woman who underwent single embryo transfer (SET) because this procedure significantly reduces the incidence of twin pregnancies and where twin pregnancies do occur after SET most are monozygotic [4]. Since HPs should be dizygotic (if it is a twin pregnancy), HPs in theory are extremely rare in SET cycles; however, case reports show that twins following SET can also be dizygotic and may be the result of a natural conception occurring during the SET [5]. Herein, we introduce the first case report of a HP following frozen SET in a spontaneous cycle with laparoscopic management that resulted in a healthy singleton full-term delivery.
A 40-year-old woman was referred to the emergency room presenting with right lower quadrant colicky pain. Her medical history revealed primary infertility and a treated pelvic inflammatory disease before marriage. Three years earlier, a hysterosalpingogram had shown obstructions in both fallopian tubes. Shortly after, she underwent a successful in vitro fertilization (IVF) cycle at a local clinic. She underwent a full-term vaginal delivery following an emergent cerclage performed at 22 weeks of gestation at our hospital. This time, when she presented to the emergency room of our hospital, she was also pregnant. A single blastocyst stage cryopreserved embryo which had been preserved since her first IVF trial was transferred in a spontaneous cycle at the 24th menstrual cycle day at the same local clinic. The timing of SET was 5 days after spontaneous ovulation, which had been confirmed with ultrasonographic examination. Also, she had several times of intercourse during assisted reproductive technologies treatment but, she could not remember the timing and frequency of it. Serum β-hCG level, estimated at the local clinic, was 112 mIU/mL 10 days after the SET and 1,285 mIU/mL 17 days after the SET.
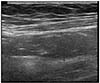
When she came to the emergency room, it was 21 days after SET. Transvaginal and transabdominal ultrasonographic examination revealed a single intrauterine gestational sac of a gestational age of 5.2 weeks (Fig. 1) and a dilated tubular structure of 1.9-cm-thickness in the right lower quadrant of her abdomen (Fig. 2). There was no fluid collection in the abdomen. Her vital signs were normal and she did not have anemia. The primary clinical suspicion was acute appendicitis that had occurred coincidently during an early intrauterine pregnancy. However, the appendix was normal and minimal hemoperitoneum was noted during laparoscopy. The left ovary showed normal appearance but, left salpinx was suspected for obstruction. The right salpinx was dilated and appeared to have hemorrhagic and trophoblastic tissues, suggestive of an ectopic pregnancy. Laparoscopic right salpingectomy was carried out, and prophylactic cerclage was performed for the ongoing intrauterine pregnancy. The pathology report confirmed an ectopic pregnancy. Her pregnancy was uneventful after the operation except for short cervical length during mid-trimester. A healthy girl weighing 3,030 g was born vaginally at 39 weeks of gestation.
To the best of our knowledge, this study is the first report of a HP following SET. Recently, there was a retrospective cohort study which indicated that at least 1 in 10 twin births following SET were dizygotic and likely the result of a concurrent natural conception [6]. The incidence of dizygotic twins in a frozen SET cycle is higher than in a fresh SET cycle, approaching about 1% of all pregnancies after frozen SET [6]. This is because the frozen SET cycle has a greater chance of spontaneous ovulation than a fresh SET. Frozen SET in natural cycles is a favored method for women with normal ovulatory menstrual cycles because the natural cycle protocol does not require exogenous hormones [7]. This case was a frozen SET that was performed on the 5th day after ovulation in a natural cycle and where the patient engaged in intercourse during their assisted reproductive technology treatment. Interestingly, there have been no dizygotic twins reported from frozen SET cycles with hormone replacement treatment.
The ideal outcome of IVF is a singleton pregnancy after SET, because multiple gestations have a higher risk of maternal and fetal morbidities. There is evidence to suggest that sexual intercourse assists the implantation provoking release of prostaglandins and growth factors [8]. However, this benefit must be weighed against the risk of dizygotic twins and even HPs, and couples should be counselled as to the advantages and disadvantages.
Because in this case the right salpingeal pregnancy was impending rupture and there was no fluid collection around it, the ultrasound finding which showed a dilated and tubular structure similar to that of appendicitis. Afterwards we found that the serum β-hCG concentration determined at the local clinic 10 days after SET was significantly higher than that of a singleton pregnancy [9]. When we performed an ultrasound examination in the emergency room, it revealed both a single gestational sac and single yolk sac of a gestational age 5.2 weeks. We should have thought of the possibility of a HP considering the high β-hCG concentration.
Referring to a recent study, dizygotic twin pregnancy after SET occurs more often than is expected and it is more often in frozen SET using natural cycle [6]. Therefore, we should always keep in mind the possibility of occurrence of a HP even when a single embryo was transferred, especially when an inappropriately high serum β-hCG level is associated with an ultrasound finding for singleton intrauterine pregnancy.
Figures and Tables
References
1. Reece EA, Petrie RH, Sirmans MF, Finster M, Todd WD. Combined intrauterine and extrauterine gestations: a review. Am J Obstet Gynecol. 1983; 146:323–330.
2. Donadio NF, Donadio N, Martins PT, Cambiaghi Cde G. Heterotopic gestation: diagnostic possibility after in vitro fertilization: a case report. Rev Bras Ginecol Obstet. 2008; 30:466–469.
3. Maruotti GM, Sarno L, Morlando M, Sirico A, Martinelli P, Russo T. Heterotopic pregnancy: it is really a rare event? The importance to exclude it not only after in vitro fertilization but also in case of spontaneous conception. Fertil Steril. 2010; 94:e49.
4. Prevention of twin pregnancies after IVF/ICSI by single embryo transfer. ESHRE Campus Course Report. Hum Reprod. 2001; 16:790–800.
5. Takehara I, Takahashi T, Hara S, Matsuo K, Igarashi H, Kurachi H. Dizygotic twin pregnancy after single embryo transfer: a case report and review of the literature. J Assist Reprod Genet. 2014; 31:443–446.
6. Osianlis T, Rombauts L, Gabbe M, Motteram C, Vollenhoven V. Incidence and zygosity of twin births following transfers using a single fresh or frozen embryo. Hum Reprod. 2014; 29:1438–1443.
7. Dal Prato L, Borini A, Cattoli M, Bonu MA, Sciajno R, Flamigni C. Endometrial preparation for frozen-thawed embryo transfer with or without pretreatment with gonadotropin-releasing hormone agonist. Fertil Steril. 2002; 77:956–960.
8. Tremellen KP, Valbuena D, Landeras J, Ballesteros A, Martinez J, Mendoza S, et al. The effect of intercourse on pregnancy rates during assisted human reproduction. Hum Reprod. 2000; 15:2653–2658.
9. Zhang X, Barnes R, Confino E, Milad M, Puscheck E, Kazer RR. Delay of embryo transfer to day 5 results in decreased initial serum beta-human chorionic gonadotropin levels. Fertil Steril. 2003; 80:1359–1363.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download