Abstract
This study assesses the fertilization and blastocyst-forming rate in mice cumulus-oocyte complexes (COCs) after the exposure of human ovarian endometriotic fluid. Endometriotic fluid was obtained from a single patient by aspiration at the time of a laparoscopic cystectomy and serially diluted. COCs were obtained from 46-week-old female BDF1 mice. After exposure to ovarian endometriotic fluid for five minutes, the COCs were washed three times and the oocytes were then fertilized by mice sperm. The fertilization and blastocyst formation rate and the proportion of hatching/hatched blastocyst in the four treatment groups were not inferior to those in non-exposure group.
Accidental exposure of oocyte to endometriotic fluid is an uncommon but possible event during oocyte retrieval with an incidence of 2.8% to 6.1% [12]. Only three human studies were published regarding the effect of fertilization rate and subsequent embryonic development after the accidental exposure of oocyte to endometriotic contents but the results were conflicting [34]. In a recent mouse experiment, exposure of cumulus-oocyte complexes (COCs) to ovarian endometriotic fluid resulted in a similar fertilization and blastocyst-forming rate but a significantly lower percentage of hatching/hatched blastocysts when compared with non-contaminated COCs [5]. In the clinical setting, endometriotic fluid exposure time is very limited because aspirated follicular fluids are immediately separated from COCs. However, the amount of exposure to endometriotic fluid would be very variable. In this study, we explored various concentration of endometriotic fluid exposure on mouse COCs and evaluated for subsequent fertilization and blastocyst-forming rate.
Commercially available BDF1 mice (Orient Co., Seoul, Korea) were used after one week adaptation. They were fed ad libitum and were kept under 12-hour light/12-hour dark cycle at 23℃. The animals used in this study were in accordance with the institutional guidelines established by the Animal Care and Use Committee of Seoul National University Bundang Hospital.
Forty six-week-old female BDF1 mice were treated with intra-peritoneal injection of 5 IU pregnant mare serum gonadotropin (Daesung Microbiological Labs, Uiwang, Korea) followed by intra-peritoneal injection of 5 IU equine chorionic gonadotropin (Daesung Microbiological Labs) 48 hours later. Oviducts were collected 13 to 14 hours later after scarification of mice through cervical dislocation. The oviducts were dissected and placed in a Petri dish containing modified mouse tubal fluid medium supplemented with 0.8% bovine serum albumin. The COCs were released by tearing the ampulla of the oviducts.
Human endometriotic fluid was obtained from a single patient by aspiration at the time of a laparoscopic cystectomy. She was 29-year-old nulligravida with 1-year infertility. Preoperative serum CA 125 level was 168.8 U/mL. The fluids were kept refrigerated at -80℃ and warmed to 37℃ before the experiment. The warmed endometriotic fluid was serially diluted as 1/2, 1/4, 1/8, and 1/16. From 46-week-old female BDF1 mice, COCs were obtained and randomly divided into five groups. In four endometriotic fluid treated group, 0.1 mL of diluted endometriotic fluid was added to 0.9 mL of modified mouse tubal fluid medium containing COCs, thus final concentrations of endometriotic fluid within medium were 0.625%, 1.25%, 2.5%, and 5%, respectively. After exposure for five minutes, the COCs were washed three times.
The cumulus cells were then removed enzymatically using 85 IU/mL hyaluronidase and by mechanical dissociation using a glass pipette. Only morphologically normal mature oocytes, as judged by the presence of a first polar body, were used for insemination.
The epididymal sperm were retrieved from the cauda epididymis of fourteen 9- to 18-week-old male mice. Sperm suspensions were pre-incubated for 1.5 hours in capacitation medium (modified mouse tubal fluid supplemented with 0.8% bovine serum albumin). Oocytes were inseminated by the sperms at a final dilution of 1 million/mL and incubated at 37℃ in humidified 5% CO2 in air.
Inseminated oocytes were washed by pipetting 6 hours later and then placed in embryo maintenance medium (Global medium supplemented with 0.4% bovine serum albumin; Life Global, Guilford, CT, USA). Fertilization was assessed by the formation of 2-cell on day 1 after insemination. The cleaved embryos were transferred to new embryo maintenance medium, and development to blastocyst was recorded on day 5 after insemination.
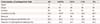
The fertilization rate in all endometriotic fluid treated groups, except 0.625% exposure group, was similar to those with a non-exposure group (Table 1). In all endometriotic fluid treated groups, no differences were observed in the blastocyst formation rate and the proportion of hatching/hatched blastocyst when compared with a non-exposure group.
Our results demonstrated no detrimental effect on subsequent fertilization, blastocyst formation rate and hatched blastocysts of mouse COCs after exposure of various concentration of endometriotic fluid. This result is consistent with the human study previously mentioned above [24] but partially in agreement with previous mice study done by Piromlertamorn et al. [5]. Piromlertamorn et al. [5] was the prototype of our study, using mouse oocyte and exposed then in a single concentration of endometriotic fluid. In that study, fertilization, cleavage and blastocyst formation rates were similar between exposed and non-exposed group but there was significant decrease in hatching/hatched blastocysts in exposed group (10.0% vs. 20.0%, P=0.015) However, the authors have mentioned that this result may not be due to endometriotic content itself, because decreased hatching/hatched blastocyst was also noted in serum-treated group as well.
We used different endometriotic fluid concentration in order to represent more natural setting during oocyte retrieval. Even though the exposure time is short (less than 5 minutes), different concentration of endometriotic fluid exposure would theoretically have a dose-response relationship and might affect oocyte quality and thus, embryo development. This study proved that there is no effect on different endometriotic fluid concentration.
Treating endometriomas before assisted reproduction is still in debate, and particular attention has focused on conservative management in recent years [678]. Although Somigliana et al. [6] and Garcia-Velasco and Somigliana [7] showed a mean 25% decrease in ovarian response to gonadotropin in endometrioma-affected ovary compared to contralateral unaffected ovary in patients with unilateral endometrioma without prior ovarian surgery, the paradox of diminished ovarian reserve after surgical therapy must also be considered. Due to recent evidence of no effect on in vitro fertilization outcome during the presence of endometrioma and no improvement of in vitro fertilization outcome after surgical excision, coupled with experimental results in mouse oocytes, a more conservative approach for endometrioma during assisted reproduction would be a better choice [9].
Our study has some limitations. First, we used endometriotic fluid obtained from a single patient. Not all endometriomas have same chemical composition, and different types of endometriotic fluid might have different cytokine profiles and oxidative stress on oocytes. Secondly, we did not analyze pregnancy rate and implantation rate for the endometrial fluid exposed group, which is also an important factor for evaluating infertility.
Therefore, in order to truly understand the pathophysiology of detrimental effect of endometriotic fluid and infertility, further study regarding contents of endometriotic fluid and its cytotoxic effect in surrounding follicles, as well as its impact in pregnancy rate and implantation rate would be informative.
Figures and Tables
Acknowledgments
This work was supported by grant no. A120043 from the Korea Health Care Technology R&D Project, Ministry of Health and Welfare, Korea.
References
1. Benaglia L, Bermejo A, Somigliana E, Scarduelli C, Ragni G, Fedele L, et al. Pregnancy outcome in women with endometriomas achieving pregnancy through IVF. Hum Reprod. 2012; 27:1663–1667.
2. Benaglia L, Cardellicchio L, Guarneri C, Paffoni A, Restelli L, Somigliana E, et al. IVF outcome in women with accidental contamination of follicular fluid with endometrioma content. Eur J Obstet Gynecol Reprod Biol. 2014; 181:130–134.
3. Suwajanakorn S, Pruksananonda K, Sereepapong W, Ahnonkitpanit V, Chompurat D, Boonkasemsanti W, et al. Effects of contaminated endometriotic contents on quality of oocytes. J Med Assoc Thai. 2001; 84:Suppl 1. S371–S376.
4. Khamsi F, Yavas Y, Lacanna IC, Roberge S, Endman M, Wong JC. Exposure of human oocytes to endometrioma fluid does not alter fertilization or early embryo development. J Assist Reprod Genet. 2001; 18:106–109.
5. Piromlertamorn W, Saeng-anan U, Vutyavanich T. Effects of ovarian endometriotic fluid exposure on fertilization rate of mouse oocytes and subsequent embryo development. Reprod Biol Endocrinol. 2013; 11:4.
6. Somigliana E, Infantino M, Benedetti F, Arnoldi M, Calanna G, Ragni G. The presence of ovarian endometriomas is associated with a reduced responsiveness to gonadotropins. Fertil Steril. 2006; 86:192–196.
7. Garcia-Velasco JA, Somigliana E. Management of endometriomas in women requiring IVF: to touch or not to touch. Hum Reprod. 2009; 24:496–501.
8. Ruiz-Flores FJ, Garcia-Velasco JA. Is there a benefit for surgery in endometrioma-associated infertility? Curr Opin Obstet Gynecol. 2012; 24:136–140.
9. Keyhan S, Hughes C, Price T, Muasher S. An update on surgical versus expectant management of ovarian endometriomas in infertile women. Biomed Res Int. 2015; 2015:204792.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download