Abstract
Objective
To estimate the incidence of falsely elevated risk of ovarian malignancy algorithm (ROMA) in a group of women with pathologically confirmed endometrioma and to investigate the associated factors.
Methods
One hundred premenopausal women surgically diagnosed with ovarian endometrioma were selected. Preoperative clinical, laboratory, and surgical characteristics were compared between the elevated-risk group (ROMA-premenopausal value, ≥7.4%) and normal-risk group (ROMA-premenopausal value, <7.4%).
Results
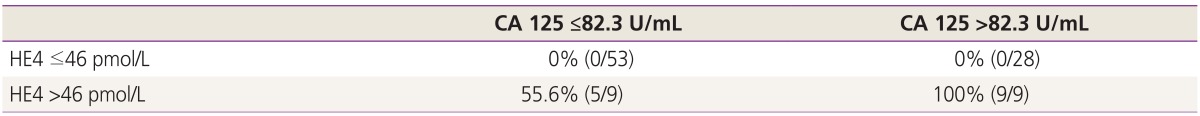
Elevated ROMA was observed in 15 women (false positive rate, 15%). Excluding one woman with known chronic renal failure, we compared the characteristics of 99 women between the elevated-risk group (n=14) and the normalrisk group (n=85). None of the clinical and surgical variables distinguished the two groups. Serum level of CA 125 >82.3 U/mL and serum level of human epididymis protein 4 (HE4) >46 pmol/L could predict an elevated ROMA test with a statistical significance. When serum level of HE4 ≤46 pmol/L, none of the women showed an elevated ROMA test, regardless of serum level of CA 125; however, 55.6% of the women showed an elevated ROMA test when serum level of HE4 >46 pmol/L and CA 125 ≤82.3 U/mL and all women showed an elevated ROMA test when serum level of HE4 >46 pmol/L and CA 125 >82.3 U/mL.
Go to : 
For women with ovarian tumors, a number of diagnostic indexes are combined with different variables. Several combinations of serum biomarkers were tested to distinguish benign from malignant ovarian lesions, and only a 2-marker combination, including CA 125 and human epididymis protein 4 (HE4), showed superior diagnostic performance [1]. From these observations, the risk of ovarian malignancy algorithm (ROMA) was conceptualized [2]. The ROMA is an index based on evaluation of serum CA 125 and HE4 levels in combination with the hormonal status of patients with adnexal tumors. The dual-marker algorithm achieved significantly higher sensitivity for identifying women with epithelial ovarian cancer (EOC) than the risk of malignancy index in the same cohort [3]. While women with endometriosis or inflammation could be falsely positive in the risk of malignancy index system, the ROMA system was found to be most accurate for differentiating endometriosis from EOC or borderline ovarian tumors [4]. Collectively, the ROMA showed excellent diagnostic performance in excluding malignancies in premenopausal women and was highly accurate in the diagnosis of EOC in postmenopausal women [5].
Although the initial reports were promising, several validation studies showed some limitations of the ROMA. For example, it did not perform better than HE4 alone in the diagnosis of early-stage EOC. Neither the ROMA nor HE4 alone did increase the detection of mucinous ovarian cancer, which is commonly metastatic from other sites [67]. The sensitivity of ROMA was reported to be relatively low (66%) in premenopausal women; thus, 1 of 3 premenopausal women with a malignant tumor would be misdiagnosed as having a benign disease (i.e., false negative) and therefore would not be referred to oncology specialists [8]. In a systematic review and meta-analysis, the ROMA had increased diagnostic sensitivity for ovarian cancer (87%), but its specificity (82%) was lower than that of HE4 alone (87%) [9]. An 82% specificity of the ROMA indicates that 18% the results are falsely positive and the risk of malignancy would be falsely reported to be elevated even in benign conditions.
Currently, renal failure is known to be the main source of increased false positive results of elevated HE4 level [6]. Elevated HE4 levels have been observed in patients with chronic renal disease, which may result from decreased elimination or increased production of HE4 from damaged renal tubules [10]. High creatinine concentrations are associated with higher HE4 concentrations [11]. The median HE4 concentration in patients with renal failure was 1,157 pmol/L, 30 times higher than that in healthy individuals (48.9 pmol/L). Thus, serum HE4 concentrations were extremely influenced by renal failure [11]. By contrast, the median serum CA 125 concentration in the patients with renal failure was 17.8 U/mL, which was still under the cutoff values, and the false positive rate was 19.0% (11/58 subjects), revealing that serum CA 125 level was less influenced by renal failure.
Falsely elevated ROMA can be attributed to a higher false positive rate of CA 125, especially in endometrioma [6]. Serum HE4 levels in healthy subjects increased with age and smoking habits, but were not affected by menstrual cycle, pregnancy, oral contraceptive use, or endometriosis [1112]. Increased age was found to be associated with a gradual increase in serum HE4 concentration and a gradual decrease in serum CA 125 level [11].
The aim of this study was to estimate the incidence of falsely elevated ROMA in a group of women with pathologically confirmed endometrioma and to investigate the risk factors associated with false positive results.
Go to : 
A single-institution retrospective study was conducted at the Seoul National University Bundang Hospital with the approval of the institutional review board. One hundred premenopausal women surgically diagnosed as having ovarian endometrioma between October 2014 and July 2015 were selected.
The patients' demographic and clinical characteristics were collected from electronic medical records, which included the women's age, body mass index, parity, menopausal status, smoking status, and past or current medical disease. Results of routine electrocardiography and chest radiography were collected within 1 month before surgery. We also checked for the presence of breast imaging, but only eight women underwent mammography and/or breast sonography, with normal results in seven women and fibroadenoma in one woman.
The presumptive diagnosis of ovarian mass in all the women was endometrioma. The severity of pelvic pain, laterality of ovarian endometrioma, and size and location of the ovarian endometrioma(s) were recorded. The severity of pelvic pain was assessed and classified as absent, mild (visual analog scale [VAS] score of 1 to 3), moderate (VAS score of 4 to 6), or severe (VAS score of 7 to 10). The largest diameter of the endometrioma on sonographic view was recorded as the size of the ovarian endometrioma. If endometrioma was present in both ovaries, the total size was estimated by adding the largest diameters of the two endometriomas. Recurrent cases of endometrioma and patients who have used dienogest were also identified.
From the surgical records, information on the method of pelvic entry, name of operation, coincident surgery, operation time, and transfusion of red blood cell was obtained. Information regarding endometriosis score, stage (evaluated according to the revised American Society for Reproductive Medicine [rASRM] guidelines), and the degree of obliteration of the posterior cul-de-sac was obtained (no, partial, or complete). From the pathological reports, the presence of endometriosis was confirmed in all the cases and additional pathologies from coincident surgeries were identified.
Laboratory data such as serum CA 125 level (normal cutoff value, ≤35 U/mL), HE4 level (normal cutoff value, ≤70 pmol/L), the ROMA (normal premenopausal cutoff value, <7.4%; normal postmenopausal cutoff value, <25.3%), preoperative and postoperative 1-day hemoglobin levels, decrease in hemoglobin level after surgery were also extracted. Serum HE4 concentrations were determined by using the HE4 assay (Abbott Diagnostics, Abbott Park, IL, USA), and serum CA 125 levels were measured by using the Architect CA 125 II assay (Abbott Diagnostics). Both blood test and sonographic examination was performed on the same day. The interval between the blood test date and the surgery date was also recorded. We also checked for the presence of menstruation on the blood test day.
All statistical analyses were performed by using PASW ver. 18 (SPSS Inc., Chicago, IL, USA). When numeric data were compared between the elevated-risk group (false positive) and normal-risk group (true negative), test for normal distribution was performed for the data in each group. If the data of both groups showed a normal distribution, the Student t-test was used, and the data were expressed as mean±standard deviation. If the data of at least one group did not show a normal distribution, the nonparametric Wilcoxon test was used, and the data were expressed as median and 95% confidence interval for the median. The proportions were compared by using the chi-square test. If more than 25% of the expected cell values were less than 5, the Fisher exact test was applied instead. The correlation between the groups was assessed by using the parametric Pearson test if both parameters showed a normal distribution. A receiver operating characteristics curve analysis was performed to determine serum cutoff of CA 125 and HE4. Results were considered significant when the P-value was <0.05.
Go to : 
Elevated ROMA was identified in 15 of the 100 premenopausal women with pathologically proven endometrioma; thus, the false positive rate was 15%. We identified one woman with known chronic renal failure and ongoing hemodialysis. This 42-year-old nulliparous woman had no pelvic pain, but an endometrioma-like mass with a 4-cm-diameter was detected on her right ovary on sonographic examination. The preoperative serum levels of the tumor markers were as follows: CA 125, 90.4 U/mL; HE4, 3,098.1 pmol/L; and ROMA, 99.9%. Twenty-seven days later, she underwent laparoscopic right ovarian cystectomy, and the presence of an endometriotic cyst was confirmed on pathological examination. The posterior culde-sac was completely obliterated, and the rASRM score was 92 (rASRM stage IV). It was interesting that the postoperative serum level of CA 125 (12 days after surgery) was decreased (60.5 U/mL), but that of HE4 (3,078.3 pmol/L) and the ROMA value (99.9%) were almost same.
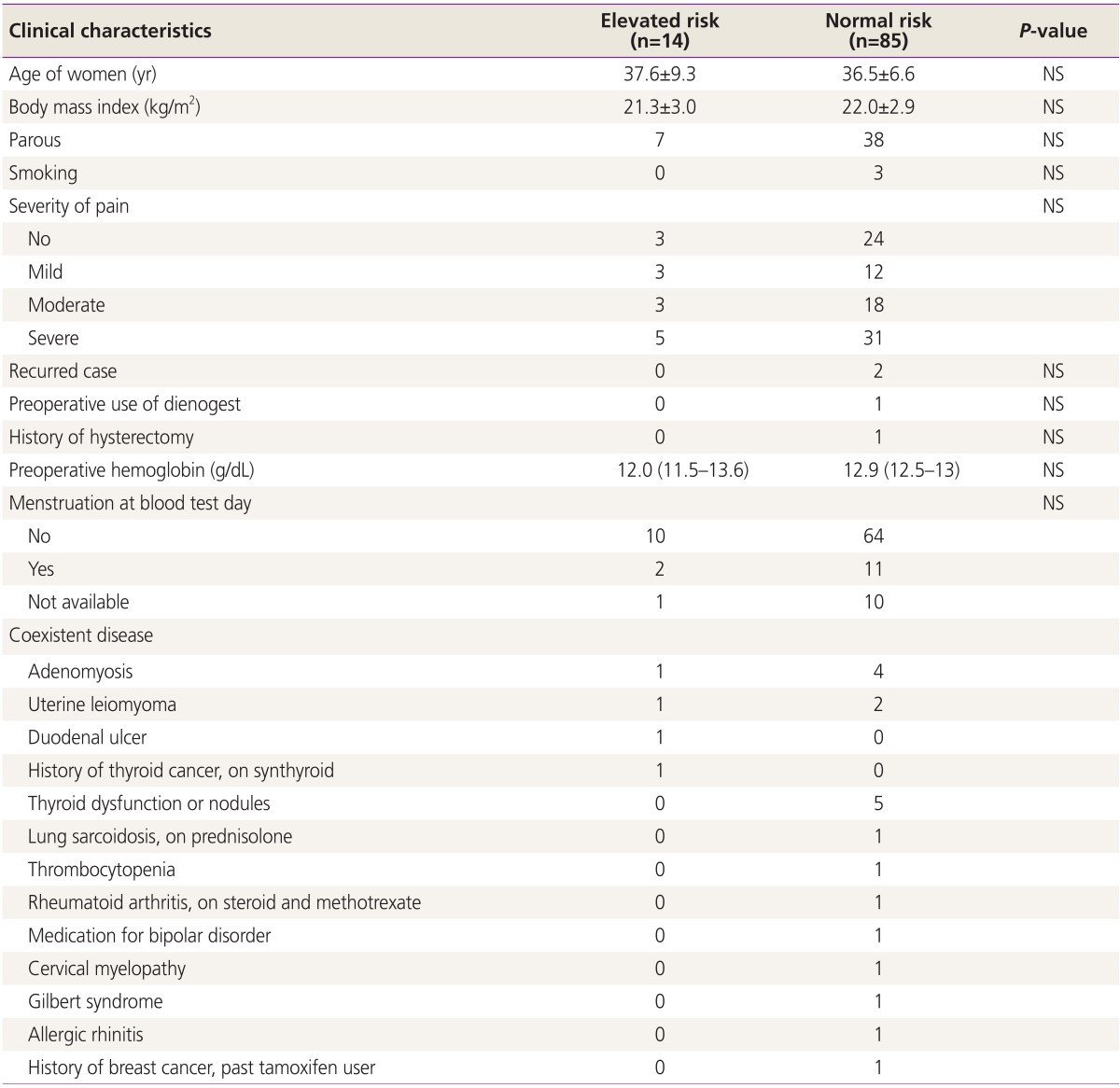
Excluding the patient with known chronic renal failure, we compared the clinical, surgical, and laboratory characteristics of the 99 women between the elevated-risk group (false positive, n=14) and normal-risk group (true negative, n=85). No significant differences in preoperative clinical features were found between the two groups (Table 1). None of the women showed evidence of myocardial infarction on routine electrocardiography and lung cancer on routine chest radiography.
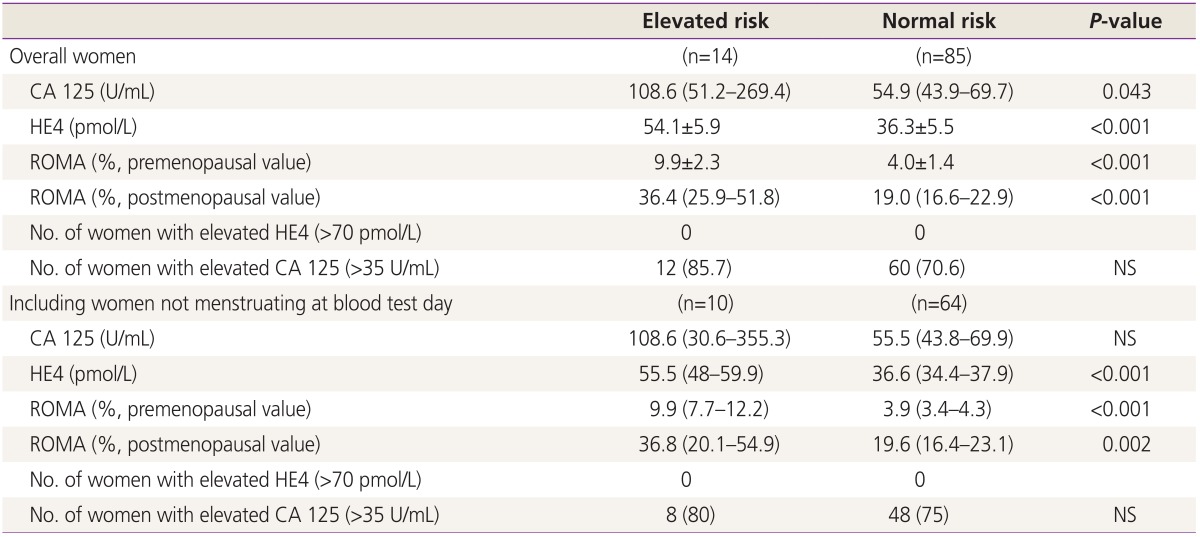
As expected, the preoperative serum levels of CA 125 and HE4, and the ROMA-premenopausal value were all higher in the elevated-risk group than in the normal-risk group (Table 2). None of the women showed an elevated serum HE4 level (>70 pmol/L), but 85.7% of the elevated-risk group and 70.6% of normal-risk group showed elevated serum CA 125 levels (>35 U/mL). As the serum CA 125 level may sometimes appear twice as high when measured during menstruation, the serum levels of the tumor markers were compared with those in 74 women who were not menstruating on the blood test day. Although the median serum CA 125 level was higher in the elevated-risk group, no significant difference was found between the two groups. HE4 level and the ROMA-premenopausal value were still higher in the elevated-risk group.
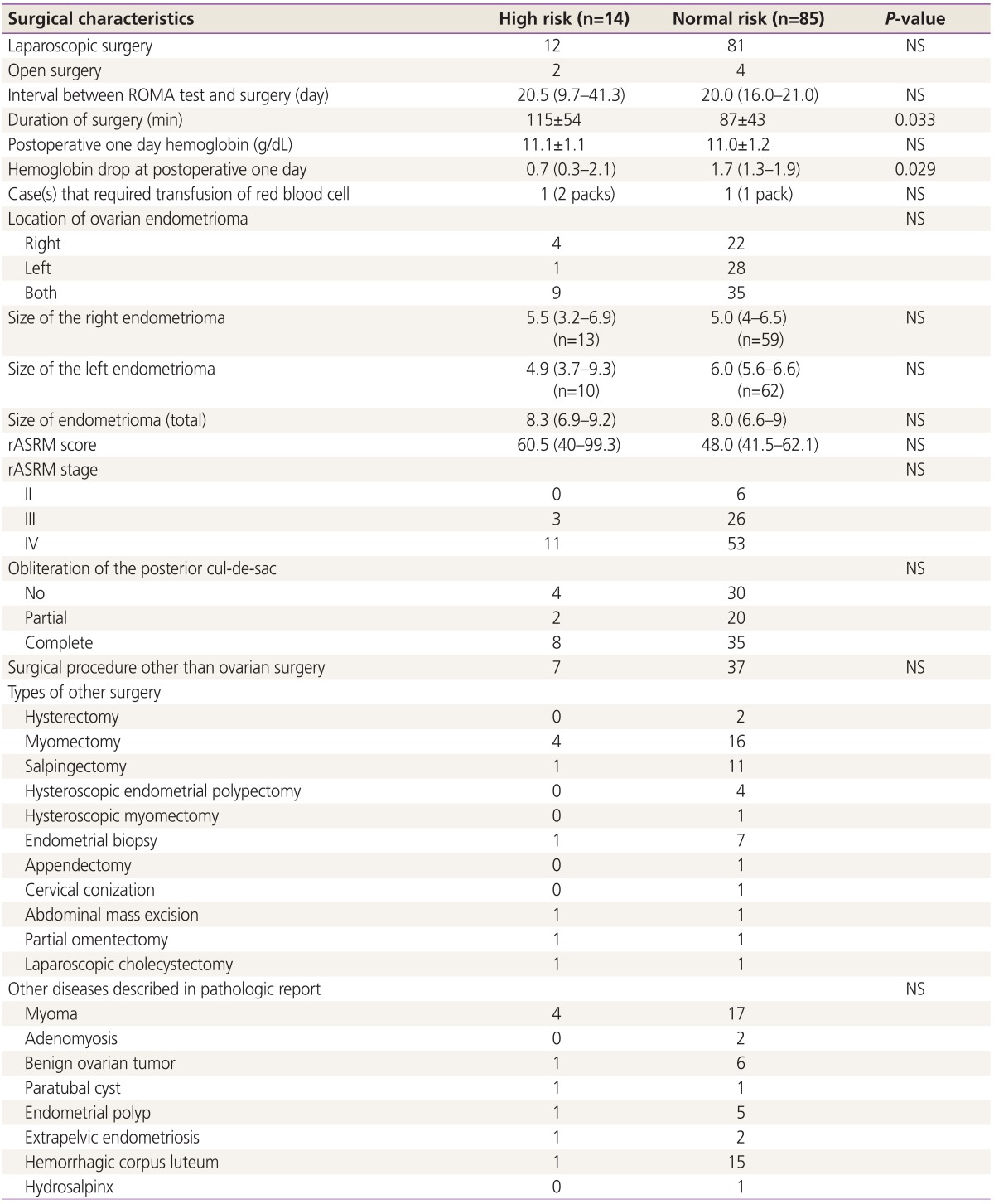
No significant differences in operative characteristics were found between the two groups (Table 3). The location and laterality of the ovarian endometrioma(s), rASRM score and stage, and presence or absence of posterior cul-de-sac obliteration were similar in the two groups. However, the mean surgical duration was significantly longer in the elevated-risk group, although no significant difference in the other surgical procedures performed along with ovarian surgery was found between the two groups. The decrease in hemoglobin level was significantly smaller in the elevated-risk group.
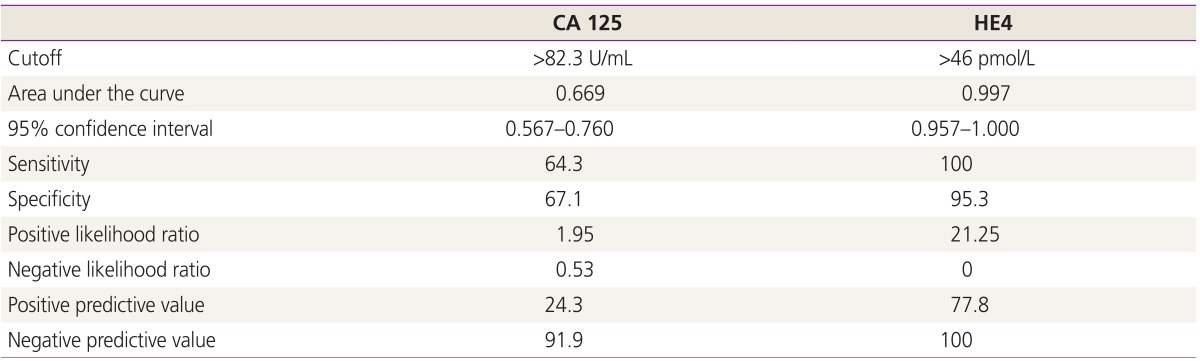
Since the ROMA test consists of the combination of serum level of CA 125 and HE4, we performed a receiver operating characteristics curve analysis to elucidate the cutoff of serum level of CA 125 and HE4 to predict an elevated ROMA test (Table 4). Serum level of CA 125 >82.3 U/mL and serum level of HE4 >46 pmol/L could predict an elevated ROMA test with a statistical significance. When serum level of HE4 ≤46 pmol/L, none of the women showed an elevated ROMA test, regardless of CA 125 level; however, 55.6% of the women showed an elevated ROMA test when serum level of HE4 >46 pmol/L and CA 125 ≤82.3 U/mL, and all women showed an elevated ROMA test when serum level of HE4 >46 pmol/L and CA 125 >82.3 U/mL (Table 5). The correlation coefficient (R-value) for CA 125 level and ROMA-premenopausal value was 0.04 (no correlation), on the contrary, the R-value for HE4 level and ROMA-premenopausal value was 0.98, indicating a strong correlation.
Go to : 
In our study, we were unable to find any clinical or surgical parameter that distinguishes the elevated-risk group from the normal-risk group for the ROMA test. It is still not clear why the ROMA test were elevated in some of the women with benign endometrioma. However, our results indicated a relatively high false positive rate (15%) in the ROMA test for discriminating ovarian endometrioma. In fact, none of the women had an HE4 value higher than 70 pmol/L, which is an abnormal level (maximum 69.2 pmol/L in our population). Hence, if HE4 test alone was considered, no false positive result of the ROMA would have been obtained. Since the ROMA-premenopausal value was strongly correlated with serum HE4 level (r=0.98), falsely elevated ROMA results might be attributed to an elevated serum HE4 level. We demonstrated that a higher chance (14/18 subjects, 77.8%) of falsely elevated ROMA results could occur when serum level of HE4 >46 pmol/L. When serum level of HE4 was >46 pmol/L and CA 125 was >82.3 U/mL, the chance of falsely elevated ROMA results was 100%. Therefore, the clinicians should keep in mind this observational finding when they interpret the ROMA results in women with suspicious ovarian endometriosis.
The surgical procedure took longer to perform in the elevated-risk group than in the normal-risk group, which was an unexpected finding. We identified several associated factors with surgical duration, including size, stage, and bilaterality of the endometrioma; open surgery; and additional surgery (data not shown). Despite the baseline clinical and surgical characteristics that affected surgical duration did not significantly differ between the groups, surgical duration was longer in the elevated-risk group. This implies that the surgical procedures were generally more difficult in the elevated-risk group. However, as surgical duration may depend on many factors such as surgeon experience and skill and the degree of adhesion of the ovarian endometrioma, which is not simply expressed by the rASRM score, the exact association could not be determined. Furthermore, various additional surgical procedures were performed alongside the surgery for endometriosis, thus, identifying the reason for the significantly longer surgical duration in the elevated-risk group than in the normal-risk group based on our data is difficult.
In one study, one patient with breast cancer was reported to have a falsely elevated ROMA value [6]. In our study, one patient had a history of breast cancer, but she was in the normalrisk group. Our patients might have had hidden breast malignancies, but as a retrospective study, breast imaging could not be performed for all the patients. Instead, we identified eight patients who underwent breast imaging, and none of them had breast cancer.
The one of main limitations in this study was a retrospective one, and therefore not all information were available that may have affected the serum CA 125 and HE4 levels. Inclusion of a relatively small number of subjects was another limitation. Only 15 subjects in the falsely elevated group might not be sufficient to report the false positive rate of ROMA in patients with ovarian endometrioma. Therefore, a larger study population would be necessary in order to appropriately estimate the false positive rate.
Discriminating benign from malignant disease is important not only to ensure appropriate management by a gynecologic oncology surgeon in the setting of malignancy but also to avoid unnecessary diagnostic procedures, including surgery, and anxiety in women with asymptomatic, nonmalignant conditions. The ROMA has been approved by the Food and Drug Administration in USA as a useful indicator for differentiating malignant from benign pelvic masses. However, a higher serum level of HE4 and/or CA 125 could result in a falsely elevated result, the interpretation should be cautious in women typical sonographic features of ovarian endometrioma.
In conclusion, the incidence of falsely elevated ROMA was 15% in a group of women with pathologically confirmed endometrioma. Except in one case with known chronic renal failure, we could not find any variable that distinguishes elevated risk from normal risk for the ROMA test. Since the ROMA value was strongly correlated with serum HE4 level, falsely elevated ROMA results might be attributed to an elevated serum HE4 level. The potential limitations of the ROMA test in clinical management will be further investigated.
Go to : 
References
1. Moore RG, Brown AK, Miller MC, Skates S, Allard WJ, Verch T, et al. The use of multiple novel tumor biomarkers for the detection of ovarian carcinoma in patients with a pelvic mass. Gynecol Oncol. 2008; 108:402–408. PMID: 18061248.

2. Moore RG, McMeekin DS, Brown AK, DiSilvestro P, Miller MC, Allard WJ, et al. A novel multiple marker bioassay utilizing HE4 and CA125 for the prediction of ovarian cancer in patients with a pelvic mass. Gynecol Oncol. 2009; 112:40–46. PMID: 18851871.

3. Moore RG, Jabre-Raughley M, Brown AK, Robison KM, Miller MC, Allard WJ, et al. Comparison of a novel multiple marker assay vs the Risk of Malignancy Index for the prediction of epithelial ovarian cancer in patients with a pelvic mass. Am J Obstet Gynecol. 2010; 203:228.e1–228.e6. PMID: 20471625.

4. Jacob F, Meier M, Caduff R, Goldstein D, Pochechueva T, Hacker N, et al. No benefit from combining HE4 and CA125 as ovarian tumor markers in a clinical setting. Gynecol Oncol. 2011; 121:487–491. PMID: 21420727.

5. Stukan M, Dudziak M, Ratajczak K, Grabowski JP. Usefulness of diagnostic indices comprising clinical, sonographic, and biomarker data for discriminating benign from malignant ovarian masses. J Ultrasound Med. 2015; 34:207–217. PMID: 25614393.

6. Partheen K, Kristjansdottir B, Sundfeldt K. Evaluation of ovarian cancer biomarkers HE4 and CA 125 in women presenting with a suspicious cystic ovarian mass. J Gynecol Oncol. 2011; 22:244–252. PMID: 22247801.
7. Van Gorp T, Cadron I, Despierre E, Daemen A, Leunen K, Amant F, et al. HE4 and CA125 as a diagnostic test in ovarian cancer: prospective validation of the risk of ovarian malignancy algorithm. Br J Cancer. 2011; 104:863–870. PMID: 21304524.

8. Karlsen MA, Sandhu N, Hogdall C, Christensen IJ, Nedergaard L, Lundvall L, et al. Evaluation of HE4, CA125, risk of ovarian malignancy algorithm (ROMA) and risk of malignancy index (RMI) as diagnostic tools of epithelial ovarian cancer in patients with a pelvic mass. Gynecol Oncol. 2012; 127:379–383. PMID: 22835718.

9. Lin J, Qin J, Sangvatanakul V. Human epididymis protein 4 for differential diagnosis between benign gynecologic disease and ovarian cancer: a systematic review and metaanalysis. Eur J Obstet Gynecol Reprod Biol. 2013; 167:81–85. PMID: 23228410.

10. Romeo V, Framarino Dei Malatesta M, Nudo F, Simonelli L, Derme M, Berloco PB. Is HE4 serum level a valid screening test in women candidates for kidney transplant? A case report and a review of literature. Clin Ter. 2014; 165:e162–e165. PMID: 24770827.
11. Li PL, Zhang X, Li TF, Wang LL, Du LT, Yang YM, et al. Combined detection of sialic acid and hydroxyproline in diagnosis of ovarian cancer and its comparison with human epididymis protein 4 and carbohydrate antigen 125. Clin Chim Acta. 2015; 439:148–153. PMID: 25445414.

12. Granato T, Porpora MG, Longo F, Angeloni A, Manganaro L, Anastasi E. HE4 in the differential diagnosis of ovarian masses. Clin Chim Acta. 2015; 446:147–155. PMID: 25892674.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download