Abstract
Objective
To evaluate the usefulness of transvaginal ultrasound measurements of cervical length before and after elective prophylactic cervical cerclage in predicting preterm delivery before 32 weeks of gestation.
Methods
Women who underwent an elective cerclage operation at 14 to 19 weeks of gestation and who delivered between January 2004 and December 2009 were enrolled in this study (n=52). Ultrasonography was performed to measure cervical length before and after cerclage. The primary outcome was defined as preterm delivery before 32 weeks of gestation. A receiver operating characteristic curve was used to determine the most discriminating cut-off values of ultrasonographic cervical parameters predictive of preterm delivery before 32 weeks of gestation.
Results
Among the 52 patients studied, ten delivered before 32 weeks of gestation. Among the ultrasonographic cervical parameters compared, only the cervical length after cerclage was significantly different (shorter) in patients who delivered before 32 weeks of gestation (P=0.037) compared to that of those who delivered after 32 weeks of gestation in univariate and multivariate analyses (odds ratio, 0.402; 95% confidence interval, 0.174 to 0.925; P=0.021). The receiver operating characteristic curve showed that a cervical length of 25 mm or less after cerclage was predictive of preterm delivery before 32 weeks of gestation (area under curve, 0.71; 95% confidence interval, 0.56 to 0.87; P=0.029) with a sensitivity of 91.0% and a specificity of 30.0%.
Elective prophylactic cervical cerclage is usually performed in women who have a history of spontaneous second-trimester miscarriages and preterm delivery or those who underwent cervical procedures such as conization that may cause cervical incompetence [1]. However, not all cerclage operations resulted in full term delivery; some patients delivered as preterm even after a cerclage operation. A recent study showed that women who underwent the procedure, regardless of whether it was elective or emergent, had a higher rate of preterm birth compared to that of the general population [2]. The results from studies of the effectiveness of elective cerclage have been mixed [3456], and few studies have attempted to determine parameters that can predict preterm delivery after elective cerclage [789101112].
Cervical length measurement is the most powerful method to predict preterm delivery in women with a history of prior preterm birth [13]. Studies of post-elective cerclage have shown that cervical length is correlated with eventual pregnancy outcome [714]. Some studies showed that prophylactic cerclage procedures resulted in measurable cervical lengthening [81015]. It is not known whether this relative restoration of cervical anatomy after prophylactic or urgent cerclage predicts pregnancy outcome [8].
Our aims in this study are therefore to determine 1) ultrasonographic cervical parameters predictive of preterm delivery before 32 weeks of gestation after elective cerclage and 2) cut-off values for these cervical parameters predictive of preterm delivery before 32 weeks of gestation [7].
In this retrospective study, the records of women who underwent elective cerclage and who subsequently delivered at a tertiary referral hospital in Seoul, Korea from January 2004 to December 2009 were examined. Patients were included based on their prior obstetric histories. Twin pregnancies (n=4), the transferred after cerclage (n=13) and, re-cerclage operation receivers (n=2) in one pregnancy were excluded from this study. This study was approved by the institutional review board for Clinical Research in our institute. Among a total of 72 elective cerclage cases performed during the study period, 52 patients fulfilling the inclusion criteria were investigated. The indications for elective cerclage were patients with (1) a prior obstetric history of advanced cervical dilation and/or membrane bulging to the external os in the second trimester (n=29), (2) a history of conization (n=22), (3) a history of cervical pregnancy, and (4) a history of preterm delivery at 28 weeks of gestation. One patient underwent cerclage for (1) and (2) concurrently.
The presence of funneling and the overall cervical length from the internal os to the external os, regardless of the cerclage knot, was evaluated before and after cerclage using a 4–9 MHz transvaginal ultrasound probe (Accuvix V10, Medison, Seoul, Korea). Cervical length was measured in the operating room at least three times and the shortest value was recorded. In all patients, the McDonald cerclage procedure was performed using 5 mm Mersilene tape at 14 to 19 weeks of gestation. None of the patients had uterine contractions, vaginal bleeding, or a watery vaginal discharge at the time of cerclage. After cerclage, we used tocolytics such as nifedipine, ritodrine, or atosiban when preterm labor was diagnosed. Antibiotics were prescribed when premature preterm rupture of membranes was confirmed. Steroids were used when delivery was pending before 34 weeks of gestation.
The study subjects were stratified into two groups to assess the predictive values of cervical parameters after cerclage for preterm delivery: those who delivered before 32 weeks of gestation (n=10, group 1) and those who delivered after 32 weeks of gestation (n=42, group 2). The cutoff of 32 weeks of gestation was chosen based on the findings of the French The etude epidémiologique sur les petits ages gestationnels cohort study [16], namely that delivery before 32 weeks of gestation was associated with a significant increase in neonatal mortality and morbidity [13].
Demographic characteristics including prior obstetric history and a history of conization, cervical length before and after cerclage, measured cervical length change before and after cerclage, and pregnancy outcomes were compared between the two groups. Prior obstetric history was defined as a history of a previous cerclage operation and/or a history of cervical incompetence defined as advanced cervical dilation and/or fetal membrane bulging to the external os in the second trimester.
Categorical data were analyzed with Fisher's exact tests, and continuous data were analyzed with Mann-Whitney U-tests. The significance of the change in the cervical length before and after cerclage was analyzed using Wilcoxon's signed rank test. Multivariable analysis was used to adjust for known confounders identified in previous studies and for variables associated with preterm delivery before 32 weeks in the univariate analysis with P<0.2, namely a history of cerclage, history of conization, gestational week at which the cerclage operation was performed, cervical length before and after cerclage, and change in cervical length before and after cerclage. Multivariable logistic was used to assess the effects of confounding variables. Receiver operating characteristic (ROC) curves were used to identify the best cut-off values of cervical parameters for predicting preterm birth before 32 weeks of gestation after elective cerclage [13]. Statistical analyses were performed using PASW ver. 18 (SPSS Inc., Chicago, IL, USA), and a P-value less than 0.05 was considered significant.
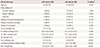
The mean maternal age was 32.6±3.7 years. A cerclage operation was performed at an average gestational age of 15.3±1.5 weeks. The mean cervical length before cerclage was 29.4±9.2 mm (range, 10.0 to 52.5 mm) compared to 35.6±9.4 mm (range, 13.0 to 55.0 mm) after cerclage. Gestational age at delivery was 36.5±5.8 weeks. The mean cerclage to delivery duration was 147.7±40.1 days. The relationships between ultrasonographic parameters and early preterm delivery before 32 weeks are shown in Table 1. Cervical lengths before cerclage were not significantly different between the two groups. In contrast, cervical lengths after cerclage were significantly different between the two groups (P=0.037); the mean cervical length after cerclage was longer in group 2. Nevertheless, there was no significant difference in the change in cervical length before and after cerclage between the two groups. There was a significant increase in overall cervical length after cerclage in both groups, as shown in Table 2.
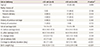
In additional analysis with the patients who have a prior obstetric history of advanced cervical dilation and/or membrane bulging to the external os in the second trimester (n=29), the history of definite cervical insufficiency, cervical lengths before and after cerclage were not significantly different between the two groups (Table 3). There was a significant increase in overall cervical length after cerclage in both groups, as shown in Table 4.
In multivariable logistic with multiple confounding variables accounting for preterm birth, only cervical length after cerclage showed a significant association with delivery before 32 weeks of gestation; in other words, preterm delivery before 32 weeks of gestation decreased as the cervical length after cerclage increased (odds ratio, 0.402; 95% confidence interval, 0.174 to 0.925; P=0.021).
ROC curve analysis (Fig. 1) revealed that cervical length measured after cerclage was a moderate predictor of early preterm delivery before 32 weeks of gestation (area under curve, 0.71; 95% confidence interval, 0.56 to 0.87; P=0.029). The best cut-off value of cervical length after cerclage for the prediction of preterm delivery before 32 weeks of gestation was 25 mm, with a sensitivity of 91.0% and a specificity of 30.0%.
In this study, we found an association between cervical length after cerclage and preterm delivery before 32 weeks of gestation. As the post-operative cervical length got longer, the probability of preterm delivery before 32 weeks of gestation was reduced. The ROC curve had an area under the curve of 0.71 with a 95 percent confidence interval of 0.56–0.87. Therefore, a cervical length of 25 mm measured immediately after cerclage could be used as a moderately confident baseline reference for early preterm delivery before 32 weeks of gestation. However, the sample size in this study was fairly small; additional studies are required to confirm our reference cut-off value of post-cerclage cervical length.
The relative risk of preterm delivery has been shown to increase as cervical length after cerclage becomes shorter. It is reasonable to hypothesize that prophylactic cerclage may reduce the risk of preterm delivery by restoring the cervical anatomy, which can act as a barrier to ascending infections [8]. Several studies have reported an increased cervical length after cerclage. Dijkstra et al. reported that both prophylactic and urgent cerclage resulted in a statistically significant increase in cervical length, although the degree of cervical lengthening after cerclage did not contribute to the success of the procedure based on the primary outcome of delivery after 37 weeks of gestation [8]. One study evaluated whether a successful cerclage depended on suture placement as close as possible to the internal cervical os, which can be represented by cerclage height [17]. Another study reported a trend toward an increased incidence of preterm delivery as cerclage height decreased, although this trend was not statistically significant [18]. A greater cerclage height results in a greater cervical length after cerclage because the overall cervical length is the sum of the cervical height (cervical length below the knot) and the cervical length above the knot. We therefore measured the overall cervical length in this study rather than cervical height.
During a cerclage operation, surgeons attempt to make the cervix as long as possible. Nevertheless, a surgeon may not be able to achieve the cervical length s/he intended, especially in cases with a very short cervical length prior to cerclage. Because these patients are at high risk for preterm delivery according to the results of this study, serial cervical length measurements after a cerclage operation are important to predict preterm birth, which can be expected if progressive cervical shortening is noted in the late second or early third trimester [19]. Serial measurements of cervical length after cerclage can help the physician to predict and prepare for preterm delivery by, for example, administering steroids to the mother to foster fetal lung maturation.
As the study being retrospective, we carefully selected and limited the patients enrolled to include only elective cerclage patients.
Limitations of our study include confounding factors such as the use of tocolytics or antibiotics. These factors might have affected the primary outcome of preterm delivery before 32 weeks. However, we argue that these factors are unlikely to have had a significant impact on the primary outcome of this study because we adopted standard management strategies for preterm labor and premature preterm rupture of membranes. Also, most of the pre and post operational cervical lengths used in the study were measured immediately before and after the surgery, although some immediate measurements were missing in patient records and were replaced by those measured in the nearest follow ups.
Practice Bulletin No. 142 "Cerclage for the management of cervical insufficiency" from the American College of Obstetrics and Gynecologists does not recommend prophylactic cerclage after conization [20]. Along with past reports in which cerclage after conization had no benefit on pregnancy outcomes [212223] a previous study in our center also showed that cervical cerclage after electrosurgical conization did not convincingly reduce the rate of spontaneous preterm delivery [24]. Present study includes the cerclage cases after conization reflecting the past practice. Cerclage cases with the definite history of cervical insufficiency need to be further evaluated with a larger population.
In summary, we found that cervical length measurements after elective cerclage operations are important for predicting preterm delivery. Patients with a post-cerclage cervical length shorter than 25 mm need to be followed-up with serial measurements. A prospective randomized study with a larger number of subjects is required to confirm our findings.
Figures and Tables
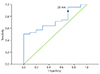 | Fig. 1Cervical length measured after cerclage was closely associated with early preterm delivery before 32 weeks of gestation (area under curve, 0.71; 95% confidence interval, 0.56 to 0.87; P=0.029). The best cut-off value of cervical length after cerclage for the prediction of preterm delivery before 32 weeks of gestation was 25 mm (sensitivity, 91.0%; specificity, 30%). |
References
1. Higgins SP, Kornman LH, Bell RJ, Brennecke SP. Cervical surveillance as an alternative to elective cervical cerclage for pregnancy management of suspected cervical incompetence. Aust N Z J Obstet Gynaecol. 2004; 44:228–232.
2. Nelson L, Dola T, Tran T, Carter M, Luu H, Dola C. Pregnancy outcomes following placement of elective, urgent and emergent cerclage. J Matern Fetal Neonatal Med. 2009; 22:269–273.
3. Lazar P, Gueguen S, Dreyfus J, Renaud R, Pontonnier G, Papiernik E. Multicentred controlled trial of cervical cerclage in women at moderate risk of preterm delivery. Br J Obstet Gynaecol. 1984; 91:731–735.
4. Rush RW, Isaacs S, McPherson K, Jones L, Chalmers I, Grant A. A randomized controlled trial of cervical cerclage in women at high risk of spontaneous preterm delivery. Br J Obstet Gynaecol. 1984; 91:724–730.
5. Althuisius SM, Dekker GA, van Geijn HP, Bekedam DJ, Hummel P. Cervical incompetence prevention randomized cerclage trial (CIPRACT): study design and preliminary results. Am J Obstet Gynecol. 2000; 183:823–829.
6. Final report. Royal College of Obstetricians and Gynaecologists multicentre randomised trial of cervical cerclage MRC/RCOG Working Party on Cervical Cerclage. Br J Obstet Gynaecol. 1993; 100:516–523.
7. Andersen HF, Karimi A, Sakala EP, Kalugdan R. Prediction of cervical cerclage outcome by endovaginal ultrasonography. Am J Obstet Gynecol. 1994; 171:1102–1106.
8. Dijkstra K, Funai EF, O'Neill L, Rebarber A, Paidas MJ, Young BK. Change in cervical length after cerclage as a predictor of preterm delivery. Obstet Gynecol. 2000; 96:346–350.
9. Groom KM, Shennan AH, Bennett PR. Ultrasound-indicated cervical cerclage: outcome depends on preoperative cervical length and presence of visible membranes at time of cerclage. Am J Obstet Gynecol. 2002; 187:445–449.
10. Guzman ER, Houlihan C, Vintzileos A, Ivan J, Benito C, Kappy K. The significance of transvaginal ultrasonographic evaluation of the cervix in women treated with emergency cerclage. Am J Obstet Gynecol. 1996; 175:471–476.
11. O'Brien JM, Hill AL, Barton JR. Funneling to the stitch: an informative ultrasonographic finding after cervical cerclage. Ultrasound Obstet Gynecol. 2002; 20:252–255.
12. O'Connell MP, Lindow SW. Reversal of asymptomatic cervical length shortening with cervical cerclage: a preliminary study. Hum Reprod. 2001; 16:172–173.
13. Fuchs F, Bouyer J, Fernandez H, Gervaise A, Frydman R, Senat MV. Ultrasound cervical length measurement for prediction of delivery before 32 weeks in women with emergency cerclage for cervical insufficiency. Int J Gynaecol Obstet. 2010; 110:245–248.
14. Rana J, Davis SE, Harrigan JT. Improving the outcome of cervical cerclage by sonographic follow-up. J Ultrasound Med. 1990; 9:275–278.
15. Althuisius SM, Dekker GA, van Geijn HP, Hummel P. The effect of therapeutic McDonald cerclage on cervical length as assessed by transvaginal ultrasonography. Am J Obstet Gynecol. 1999; 180(2 Pt 1):366–369.
16. Marret S, Ancel PY, Marpeau L, Marchand L, Pierrat V, Larroque B, et al. Neonatal and 5-year outcomes after birth at 30-34 weeks of gestation. Obstet Gynecol. 2007; 110:72–80.
17. Scheib S, Visintine JF, Miroshnichenko G, Harvey C, Rychlak K, Berghella V. Is cerclage height associated with the incidence of preterm birth in women with an ultrasound-indicated cerclage? Am J Obstet Gynecol. 2009; 200:e12–e15.
18. Miroshnichenko G, Visintine JF, Suhag A, Gerson A, Berghella V. Is cerclage height associated with the incidence of preterm birth in women with a history-indicated cerclage. Am J Perinatol. 2011; 28:83–86.
19. Hedriana HL, Lanouette JM, Haesslein HC, McLean LK. Is there value for serial ultrasonographic assessment of cervical lengths after a cerclage? Am J Obstet Gynecol. 2008; 198:705.e1–705.e6.
20. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No.142. Cerclage for the management of cervical insufficiency. Obstet Gynecol. 2014; 123(2 Pt 1):372–379.
21. Zeisler H, Joura EA, Bancher-Todesca D, Hanzal E, Gitsch G. Prophylactic cerclage in pregnancy: effect in women with a history of conization. J Reprod Med. 1997; 42:390–392.
22. Simcox R, Seed PT, Bennett P, Teoh TG, Poston L, Shennan AH. A randomized controlled trial of cervical scanning vs history to determine cerclage in women at high risk of preterm birth (CIRCLE trial). Am J Obstet Gynecol. 2009; 200:623.e1–623.e6.
23. Drakeley AJ, Roberts D, Alfirevic Z. Cervical stitch (cerclage) for preventing pregnancy loss in women. Cochrane Database Syst Rev. 2003; CD003253.
24. Shin MY, Seo ES, Choi SJ, Oh SY, Kim BG, Bae DS, et al. The role of prophylactic cerclage in preventing preterm delivery after electrosurgical conization. J Gynecol Oncol. 2010; 21:230–236.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download