Abstract
Objective
Methods
Results
Figures and Tables
Fig. 1
The percentage of women who had a emergency cesarean section, stratified according to gestational weight gain ≥18 and <18 kg (emergency cesarean section vs. vaginal delivery): <18 kg (12.3 vs. 87.7), ≥18 kg (17.8 vs. 82.2). The women with weight gain ≥18 kg had a significantly increased risk of emergency cesarean section (P=0.005). BMI, body mass index.

Fig. 2
The percentage of women who had emergency cesarean section, stratified according to gestational weight gain (emergency cesarean section vs. vaginal delivery): total (13 vs. 87), inadequate (12.6 vs. 87.4), adequate (12.6 vs. 87.4), excessive (14.2 vs. 85.8). The risk of emergency cesarean section had no significant differences between each groups (P=0.36). IOM, Institute of Medicine.

Fig. 3
The percentage of women who had a emergency cesarean section, stratified according to gestational weight gain ≥18 and <18 kg (emergency cesarean section vs. vaginal delivery): <18 kg (12.3 vs. 87.7), ≥18 kg (17.8 vs. 82.2). The women with weight gain ≥18 kg had a significantly increased risk of emergency cesarean section (P=0.005).

Table 1
The maternal characteristics of the study groups
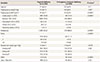
Values are presented as mean±standard deviation or number (%).
BMI, body mass index; GDM, gestational diabetes mellitus.
a)P-values are based on t-tests for continuous variables and on chi-square test for categorical variables; b)Gestational weight gain below Institute of Medicine (IOM) guidelines; c)Gestational weight gain within IOM guidelines; d)Gestational weight gain above IOM guidelines.
Table 3
ORs for emergency cesarean delivery versus vaginal delivery according to prepregnancy body mass index and gestational weight gain

OR, odds ratio; CI, confidence interval; BMI, body mass index; IOM, Institute of Medicine.
a)Adjusted for maternal age, gestational age at delivery, parity, gestational diabetes mellitus, labor induction, birth weight, neonate for large gestational age and gender; b)Adjusted for prepregnancy BMI and gestational weight gain, according to the 2009 IOM guidelines.
Table 4
Adjusted odds ratios and 95% confidence intervals for the risk of emergency cesarean delivery due to gestational weight gain, stratified according to prepregnancy body mass index

Adjusted for maternal age, gestational age at delivery, parity, gestational diabetes mellitus, labor induction, birth weight, gender, and weight gain.
a)Gestational weight gain below Institute of Medicine (IOM) guidelines; b)Gestational weight gain within IOM guidelines; c)Gestational weight gain above IOM guidelines.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download