Abstract
Objective
To demonstrate the safety of fetal delivery through placental incision in a placenta previa pregnancy.
Methods
We examined the medical records of 80 women with singleton pregnancy diagnosed with placenta previa who underwent cesarean section between May 2010 and May 2015 at the Department of Obstetrics and Gynecology, Chungbuk National University Hospital. Among the women with placenta previa, those who did not have the placenta in the uterine incision site gave birth via conventional uterine incision, while those with anterior placenta previa or had placenta attached to the uterine incision site gave birth via uterine incision plus placental incision. We compared the postoperative hemoglobin level and duration of hospital stay for the mother and newborn of the two groups.
Results
There was no difference between the placental incision group and non-incision group in terms of preoperative and postoperative hemoglobin change, the amount of blood transfusions required by the mother, newborns with 1-min or 5-min Apgar scores below 7 points or showing signs of acidosis on umbilical cord blood gas analysis result of pH below 7.20. Moreover, neonatal hemoglobin levels did not differ between the two groups.
Placenta previa occurs when the placenta totally or partially covers the opening of the cervix or when the placenta is attached in the vicinity of the cervix. Depending on the location of the attached placenta in relation to the uterine wall, placenta previa can be classified into anterior placenta previa and posterior placenta previa, and can be further categorized into complete, partial, marginal, and low lying placenta, according to the degree to which the placenta covers the opening of the cervix [1]. Placenta previa is a disease that most commonly causes vaginal bleeding in the second-half of pregnancy as well as neonatal anemia [2]. The frequency of occurrence of placenta previa varies with different studies, but is reported to be approximately 4.0 to 4.8 per 1,000 women [34]. Risk factors of placenta previa include advancing maternal age, multiparity, previous cesarean delivery, spontaneous or induced abortion, infertility treatments, and smoking and cocaine use during pregnancy [456]. Placenta previa is an important disease that increases the risk of placental abruption, postpartum bleeding, emergency cesarean delivery, and cesarean hysterectomy. Maternal mortality rates have been decreasing in recent years through early diagnosis of placental previa achieved by prenatal ultrasonography and appropriate preoperative and postoperative blood transfusion and intravenous fluid supply. However, when compared to mothers with uneventful pregnancies, newborn complications and maternal complications due to premature birth and postpartum bleeding are still markedly high [3]. Currently, lower segment transverse incision is commonly used as a uterine incision method for general cesarean sections. However, when the placenta is positioned at the uterine incision site in a placenta previa, such an incision can be used to incise the placenta to deliver the newborn. Placental incision increases the possibility of blood loss in the fetus; therefore, a uterine incision method that avoids the placenta, such as classic cesarean incision or inverted T cesarean incision, have been used to deliver the fetus. Nonetheless, although attempts to incise the uterus have been attempted by avoiding the placenta as much as possible, there have been cases where the placenta was positioned at the incision site. When the uterine corpus is incised, suturing the incised site becomes difficult and the amount of blood loss increases, which increases the risk of uterine rupture during subsequent pregnancy. During cesarean section of patients with placenta previa at our hospital, there have been cases in which the placenta was unexpectedly positioned at the uterine incision site. The placenta was incised to deliver the newborn, but both the newborn and the mother did not experience any major complications and were able to recover. In another cases, where the placenta was positioned near the usual uterine incision site, the placenta was incised to deliver the fetus, but neither the mother nor the newborn showed any unusual complications. We have previously reported the details of these cases [7]. Since then, at our hospital, we have attempted fetal delivery through uterine lower segment transverse incision and placental incision for all cases of anterior placenta previa, and posterior placenta previa, which is positioned at the uterine incision site. Furthermore, to compare maternal and newborn complications, we retrospectively analyzed the medical records of women whose placenta was incised and women whose placenta was
not incised.
We examined the medical records of all pregnant women diagnosed with placenta previa who underwent cesarean section between May 2010 and May 2015 at the Department of Obstetrics and Gynecology, Chungbuk National University Hospital. This study was approved by the Institutional Review Board for Clinical Research in our institute. We compared the subjects by dividing them into two groups. For 31 cases of anterior placenta previa, and 9 cases of posterior placenta previa, in which a part of the placenta invaded into the uterine incision site and placental incision was unavoidable, the placenta was incised to deliver the newborn; these cases were allocated to the placental incision group. Forty cases of posterior placenta previa in which placental incision was not necessary were allocated to the non-incision group. Excluding placental abruption, multifetal pregnancy, and premature rupture of membranes before 30 weeks gestation, a total of 80 subjects were enrolled in the present study. We did not select patients, but incidentally the number of subjects of both groups was equal.
Lower segment transverse incision was used as a uterine incision method for all cases, regardless of the position of the placenta. Three full-time experienced clinicians performed cesarean sections on patients with anterior placenta previa who necessitated placental incision, and placental incision and fetal delivery methods were identical for all three operating surgeons. Once the placenta was exposed after incising the myometrium, the surgeon inserted his fingers between the incised sections, and penetrated through the remaining placenta and amnion to deliver the newborn. Prior to the surgery, patients received a thorough explanation of the complications that may arise from placenta previa, the risks of fetal delivery through placental incision, and hospital expertise available to the patients and guardians. All patients provided consent.
We divided the patients into the placental incision group and the non-incision group. For mothers, preoperative and postoperative hemoglobin change, presence of blood transfusion, amounts of blood transfusion, and duration of hospital stay were compared. For newborns, Apgar score, umbilical cord blood gas analysis and hemoglobin, and duration of hospital stay were compared. To determine the presence of anemia in two-day old newborns, capillary blood sampling was conducted for comparative analysis. Shapiro-Wilk normality test, Student's t-test, Mann-Whitney U-test, chi-square test, and Fisher's extract test were used for statistical analysis of the results, and P<0.05 was regarded as statistically significant. All analyses were performed using IBM SPSS ver. 20 (IBM Corp., Armonk, NY, USA).
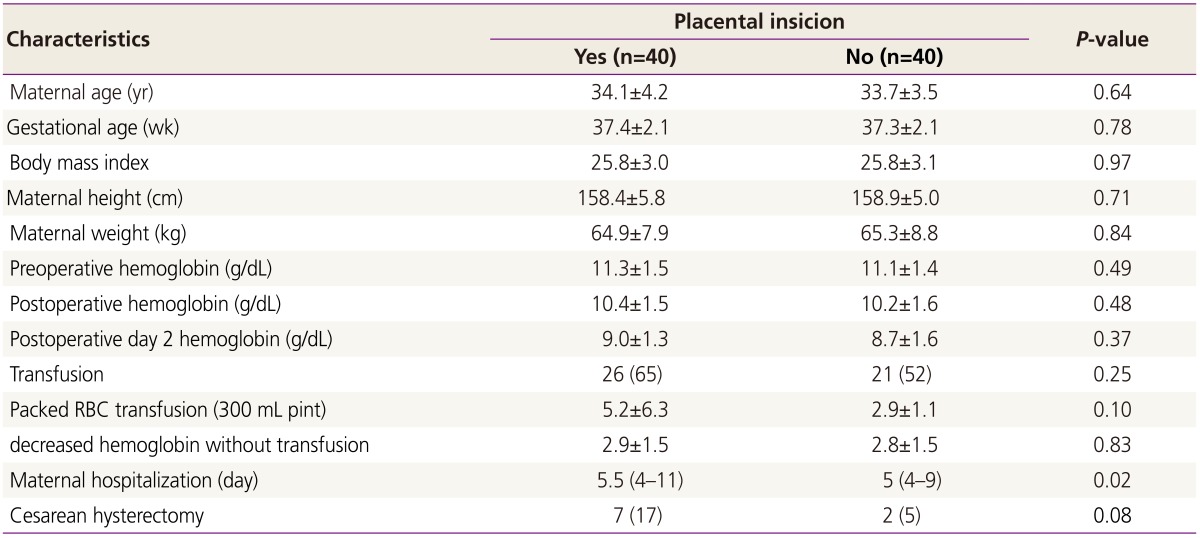
Of the total placenta previa pregnancies, the placental incision group included 40 patients and the non-incision group, 40 patients. Comparison of the placental incision group and the non-incision group revealed that age, gestational week, height, weight, body mass index, and preoperative hemoglobin level all followed normal distributions, and no statistically significant difference in clinical characteristics was observed between the two groups.
Depending on the placental incision, the frequency of mothers who received blood transfusion during or after surgery was 26 out of 40 patients in the placental incision group, and 14 out of 40 patients in the non-incision group. There was no statistical significant difference between the two groups. Of the mothers who did not receive blood transfusion in the two groups, we examined the change between hemoglobin level before surgery and 2 days after surgery. Mothers who received blood transfusion before or after surgery were excluded. The reduced hemoglobin level between the placental incision group and the non-incision group was not considered statistically significant.
The duration of hospital stay of mothers in both groups was a median of 5.5 days (range, 4 to 11 days) in the incision group and a median of 5 days (range, 4 to 9 days) in the non-incision group. Although this difference was statistically significant, it was not a clinical major difference. The frequency of cesarean hysterectomy was 7 patients in the placental incision group and 2 patients in the non-incision group. Pathology examination confirmed placenta accreta in 8 of these 9 patients (Table 1). Of the patients in the placental incision group who received hysterectomy for accreta, 1 person received intensive care unit care after surgery. There were no maternal deaths in the present study.
The reduced hemoglobin level between 31 patients with anterior placenta and 9 with posterior placenta in placental incision group was not considered statistically significant. The frequency of cesarean hysterectomy was 6 patients in the anterior placenta and 1 in the posterior placenta in placental incision group, and not considered statistically significant.
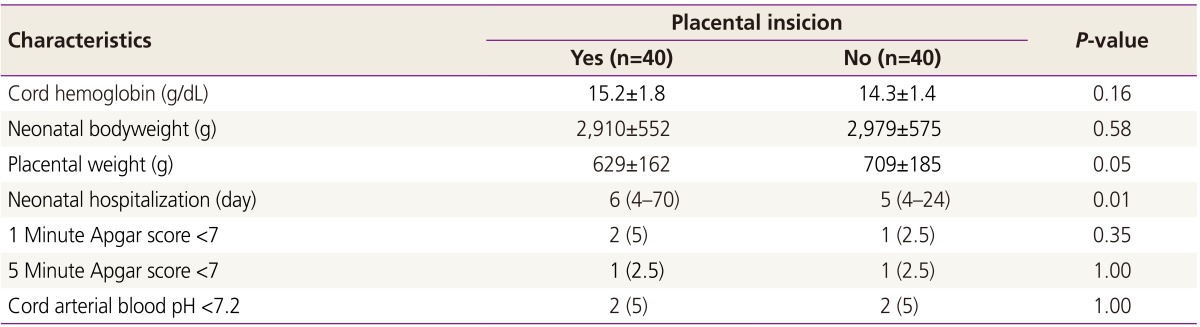
Comparing the neonatal Apgar score between the two groups, there was no difference in signs that suggested mild fetal distress. Umbilical cord blood gas analysis results showed no difference between the two groups in the occurrence of blood acidosis below pH 7.20. The total duration of hospital stay for the newborns was a median of 6 days (range, 4 to 70 days) in the placental incision group and a median of 5 days (range, 4 to 24 days) in the non-incision group, showing an increased duration in the placental incision group (Table 2). There were no newborn deaths during hospitalization after delivery.
There was no significant difference in neonatal prognosis described above between 31 patients with anterior placenta and 9 with posterior placenta in placental incision group.
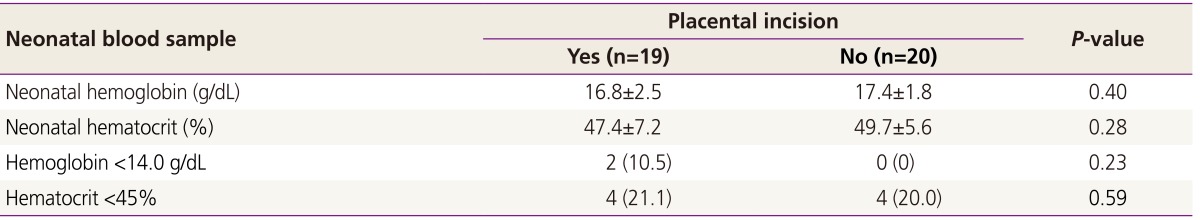
For all the study subjects, we analyzed those cases in which capillary blood sampling was obtained in two-day old newborns to determine the presence of neonatal anemia due to blood loss during placental incision. Although not all newborns received blood tests, there was no statistical difference in the percentage of newborns tested between the two groups categorized according to the previous placental incision used.
In the newborn group that underwent blood testing, hemoglobin level and presence of anemia 2 days after delivery was compared between the placental incision group and non-incision group, and no statistically significant difference was observed between the two groups (Table 3).
Placenta previa is the primary cause of neonatal anemia, and delivery of placenta previa pregnancy occurs generally through cesarean section. Although there are differences in uterine incision methods utilized, lower segment transverse incision has been reported in 71% to 96% of cases [8910]. The maternal blood transports oxygen and nutriments to the villus of the chorion, and the fetal blood circulates within the placenta, absorb the oxygen and nutrients from the maternal blood, and excrete wastes through the maternal blood. Therefore, when the placenta is incised, there is an increased risk of not only maternal blood loss but also of neonatal blood loss. Hence, various diagnostic methods and surgical techniques have been used to avoid placental incision for placenta previa pregnancy.
Before ultrasound was commonly utilized, placenta previa was diagnosed using radioactive isotopes such as 99mTc and ll3mln, but this is currently no longer practiced due to the risk of radiation exposure for mothers and fetuses and the difficulty of scanning [11]. Using magnetic resonance imaging (MRI), Kay and Spritzer [12] revealed the causes of vaginal bleeding in 15 patients in whom ultrasound failed to identify the causes of third-trimester bleeding. They stressed the effectiveness of MRI as a diagnostic method to examine the position of the placenta and placental abnormalities during vaginal bleeding of unknown cause, but pointed out the difficulties involved in repeatedly using this method due to the high scanning fees and long scanning times. Currently, diagnosis through transvaginal sonography is widely utilized as the most precise, convenient, and safe method; however, false-positive test results might arise depending on the degree of distention of the bladder and uterine contraction. Repeated tests to determine the best uterine incision site to avoid the placenta are needed, and the reliability of the test might differ significantly with the practitioner [13].
As a surgical technique that avoids the placental incision, classical cesarean incision, inverted T cesarean incision, and medial-transverse incision have been used. In 2003, Ward [14] reported a surgical technique for fetal delivery. After performing lower segment transverse incision once the position of the placenta is confirmed, the placenta does not need to be incised, and the practitioner can insert his fingers between the placenta and the uterus to separate and partially abrupt the placenta. Afterwards, the separated placenta can be first expulsed to the uterine incision site, and then the newborn can be delivered. He argued that this surgical technique could be effectively utilized not only for placenta previa but also for cesarean section in which the placenta is unexpectedly positioned at the uterine incision site. However, because placenta previa is frequently accompanied by accreta, this surgical technique is limited when the placenta and uterus cannot be separated. Ogawa et al. [15] incised the fundus of the uterus in an anterior placenta previa pregnancy accompanied by accreta, and delivered the newborn. After suturing the uterine incision site with placenta in situ, they performed a total hysterectomy. When cesarean hysterectomy is planned from the beginning, this technique is advantageous in that the fetus can be delivered without damaging the placenta. Kotsuji et al. [16] performed a cesarean delivery through transverse uterine fundal incision for 34 mothers with placenta previa with history of cesarean section who underwent MRI and had a high risk of accreta.
According to research studies that reported the shortcomings of surgical techniques other than lower segment transverse uterine incision, Patterson et al. [17] compared a group of patients who received classical cesarean incision or inverted T cesarean incision to a group who received lower segment transverse incision. The authors reported that the frequency of infection and blood transfusion was high, demonstrating that there was a significant difference in the prevalence of mothers with extended hospital stay. Greene et al. [18] reported that the occurrence of infection was high, bleeding was common, and uterus was damaged in patients who underwent classical cesarean incision.
Based on data from mothers with placenta previa who delivered newborns through placental incision, Kim et al. [7] reported that the risk of mothers and newborns in the placental incision group was not significantly different from that of mothers and newborns in the non-incision group. However, because of the small sample size of both the placental incision group and the sample size of blood tested newborns at the time of study, further studies using more cases are needed. In the present study, the average neonatal hemoglobin level between newborns delivered without placental incision and newborns through placental incision was compared and no significant differences were found. Neonatal anemia is generally defined as a hemoglobin level below 14 g/dL and a hematocrit below 45%; no difference was observed between the two groups. Therefore, we were able to confirm that the blood loss due to placental incision did not cause neonatal anemia. Although there was a statistically significant difference between the two groups in the duration of hospital stay for mothers and newborns, we presume that this was because there were more cases of anterior placental previa in the placental incision group. When we only compared patients with posterior placenta previa, we did not observe any significant differences between the two groups in the duration of hospital stay for mothers and newborns (duration of hospital days for mothers, P=0.71; duration of hospital days for newborns, P=0.53).
We compared the changes in the preoperative hemoglobin level and the hemoglobin level 2 days after surgery from mothers who did not receive blood transfusion. For cases receiving blood transfusion, it was difficult to perform a correct statistical comparison using hemoglobin above a certain level. There was no difference between the two groups in the amount or frequency of blood transfusion received. Therefore, by comparing the hemoglobin change in mothers who did not receive blood transfusion, we presumed that we would be able to confirm that placental incision caused these differences in the amount of bleeding. The results revealed no differences between the two groups, and thus, placental incision does not affect the amount of bleeding after placenta expulsion. Moreover, 9 out of the 80 patients underwent cesarean hysterectomy, and approximately 11.6% to 16.7% of the study subjects in other related studies also underwent cesarean hysterectomy [910]. Kotsuji et al. [16] demonstrated that 16 of 34 patients diagnosed with accreta all received hysterectomy, thus not showing a large deviation from other studies.
In conclusion, fetal delivery using lower segment transverse incision to incise the placenta for anterior placenta previa pregnancy is a safe surgical technique for mothers and newborns. This surgical technique is cost-effective because it reduces the number of imaging studies needed to find out incising site for avoiding the placental incision. Furthermore, using lower segment transverse uterine incisions, the uterine suturing is simple, duration of hospital stay is shorter, bleeding is reduced, and the risk of damaging the uterus after surgery is low. However, to successfully perform a surgical technique for fetal delivery through placental incision, the time of myometrial incision to fetal delivery must be minimized, and prompt decision-making and expertise of the obstetrician are needed.
References
1. Oyelese Y, Smulian JC. Placenta previa, placenta accreta, and vasa previa. Obstet Gynecol. 2006; 107:927–941. PMID: 16582134.

2. Bizzarro MJ, Colson E, Ehrenkranz RA. Differential diagnosis and management of anemia in the newborn. Pediatr Clin North Am. 2004; 51:1087–1107. PMID: 15275990.

3. Iyasu S, Saftlas AK, Rowley DL, Koonin LM, Lawson HW, Atrash HK. The epidemiology of placenta previa in the United States, 1979 through 1987. Am J Obstet Gynecol. 1993; 168:1424–1429. PMID: 8498422.

4. Faiz AS, Ananth CV. Etiology and risk factors for placenta previa: an overview and meta-analysis of observational studies. J Matern Fetal Neonatal Med. 2003; 13:175–190. PMID: 12820840.

5. Ananth CV, Smulian JC, Vintzileos AM. The association of placenta previa with history of cesarean delivery and abortion: a metaanalysis. Am J Obstet Gynecol. 1997; 177:1071–1078. PMID: 9396896.

6. Rosenberg T, Pariente G, Sergienko R, Wiznitzer A, Sheiner E. Critical analysis of risk factors and outcome of placenta previa. Arch Gynecol Obstet. 2011; 284:47–51. PMID: 20652281.

7. Kim YG, Kim RM, Lim JH, Choi JY, Jeong EH, Kim HS. The safety of cesarean delivery through transplacental incision in anterior placenta previa. Korean J Obstet Gynecol. 2010; 53:694–699.

8. Ha JW, Chung IB, Cho HC, Lee HJ, Lee HJ, Han KH, et al. The comparison of the pregnancy outcomes according to the types of placenta previa. Korean J Obstet Gynecol. 2005; 48:51–57.
9. Won HS, Lee PR, Lee IS, Kim A, Nam JH, Kim KJ, et al. Maternal and perinatal outcomes in pregnancies complicated with placenta previa totalis. Korean J Perinatol. 1998; 9:375–380.
10. Kim SP, Lee CH, Kim SJ, Hur SY, Lee GS, Lee JH, et al. A clinical study of placenta previa. Korean J Obstet Gynecol. 1999; 42:481–486.
11. Wright FW. Placental localization by isotope scanning with 113mIn: results in 200 patients. Br Med J. 1970; 2:636–639. PMID: 5429098.

12. Kay HH, Spritzer CE. Preliminary experience with magnetic resonance imaging in patients with third-trimester bleeding. Obstet Gynecol. 1991; 78(3 Pt 1):424–429. PMID: 1876378.
13. Oppenheimer L. Society of Obstetricians and Gynaecologists of Canada. Diagnosis and management of placenta previa. J Obstet Gynaecol Can. 2007; 29:261–273. PMID: 17346497.
14. Ward CR. Avoiding an incision through the anterior previa at cesarean delivery. Obstet Gynecol. 2003; 102:552–554. PMID: 12962941.

15. Ogawa M, Sato A, Yasuda K, Shimizu D, Hosoya N, Tanaka T. Cesarean section by transfundal approach for placenta previa percreta attached to anterior uterine wall in a woman with a previous repeat cesarean section: case report. Acta Obstet Gynecol Scand. 2004; 83:115–116. PMID: 14678097.

16. Kotsuji F, Nishijima K, Kurokawa T, Yoshida Y, Sekiya T, Banzai M, et al. Transverse uterine fundal incision for placenta praevia with accreta, involving the entire anterior uterine wall: a case series. BJOG. 2013; 120:1144–1149. PMID: 23639121.

17. Patterson LS, O'Connell CM, Baskett TF. Maternal and perinatal morbidity associated with classic and inverted T cesarean incisions. Obstet Gynecol. 2002; 100:633–637. PMID: 12383525.

18. Greene RA, Fitzpatrick C, Turner MJ. What are the maternal implications of a classical caesarean section? J Obstet Gynaecol. 1998; 18:345–347. PMID: 15512105.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download