Abstract
Lymphangioma is a rare proliferation of the lymphatic system which is classified as either lymphangioma circumscription or carvenous lymphangioma. The involvement of the vulva is very rare and only a small number of case reports have been made on carvenous lymphangioma of the vulva. We herein report a case of 20-year-old unmarried girl presented with gradually expanding and painless tumor of the left labium majus. The mass was removed surgically and pathology confirmed as carvenous lymphangioma, with no recurrences to date.
Carvenous lymphangioma (CL) is extremely rare benign tumor of the vulva. To our knowledge, only 8 case reports describing patients with CL arising from the vulva reported. We here report a young patient who presented with a history of gradually growing vulva tumor , which was removed surgically and histologically diagnosed as CL.
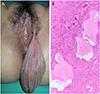
A 20-year-old unmarried girl attended the outpatient clinic of KangNam Sacred heart Hospital because of gradually expanding and painless tumor of the vulva. She noticed a small mass on left labium majus five years ago that had been increasing in size over the past year. She had attained menarche at 14 years with regular cycles and was not sexually active. She had no unremarkable medical and surgical history. Physical examination revealed soft, pedunculated skin-covered mass, about 10 cm in diameter, arising from the left labium majus (Fig. 1A). Transrectal and transabdominal ultrasonography revealed no abnormal findings of the uterus, bilateral ovaries or other pelvic organ. The result of blood test were within normal limit and the rest of gynecologic and general examinations were normal. Under general anesthesia, a circular incision was made around the base of the stalk and vulva mass was resected. In pathologic findings, macroscopically the mass was relatively well demarcated with covering skin, measuring 10×9×3 cm. On section, the cut surface showed small cystic spaces containing clear fluid. Microscopically, dilated lymphatic vessels, often cystic and ectatic, were lined by flattened endothelial cells with the paucicellular fibrous background in the mid and the deep dermis (Fig. 1B). The lymphatic endothelial cells were positive in D2-40 immunohistochemical stain and positive nuclear staining for estrogen and progesterone receptor (PR) was noted in the stromal fibroblasts. After one year the patient is in good condition without evidence of recurrence.
Lymphangiomas is benign tumor of the lymphatic system. which is classified into lymphangioma circumscription or CL also known as cystic hygroma, according to the location of lymphatics [1]. Lymphangioma circumscriptum is the most common cutaneous form of lymphangioma and the dilated lymphatics are located in the upper dermis and epidermis. It has typical skin findings such as multiple gelatinous-like papulo-vesicular vesicles or warty lesions that may appear pink, red, or black in color. In contrast to lymphangioma circumscriptum, CL present a small or large, ill-defined, poorly circumscribed subcutaneous swelling without epidermal changes because the dilated lymphatics are located within the deep reticular dermis and subcutaneous fat [2]. Cystic hygroma is reserved for those congenital lymphatic malformations that appears at birth or infancy and almost identical histopathologically to CL except that it has fewer but larger cystic cavities containing lymph [3].
Clinical features of CL was summarized in Table 1 together with the present case [1,3,4,5,6,7,8]. CL have been reported mainly in adolescent girl. The most common symptom is painless expanding mass. The most common site is unilateral labium majus (right labium majus, 4 cases; left labium majus, 4 cases) and only one case report involved bilateral labium minus.
The etiology of CL is not clear. It is postulated that developmental malformation in which obstruction or agenesis of lymphatic tissue results in lymphangiectasia, secondary to lack of normal communication of the lymphatic system, which are particularly frequent in Turner's and other malformative syndromes [7,9]. However including present case, all cases had a normal karyotype and general appearance.
Because of its propensity to occur in female patients after menarche a period of rapid increase in sex hormone levels. Watanabe et all assumed that the relationship between tumor development and sex hormone(estrogen and progesterone) levels and found positivity for estrogen receptor (ER) and PR in the tumor [8]. In this case, we also found positivity for ER and PR in the tumor. However, more ER and PR stain case reports are needed to clarify this suppostion.
Treatment option for CL is complete surgical resection. In non-pedunculated type, complete surgical resection may considered difficult, because these tumors are ill-defined and not encapsulated, thus determining the correct anatomical plane is difficult [1]. However, in pedunculated type including present case, excision was extremely easy and simple. Outcome of surgical resection of both type was excellenv and no reports described the reccurence.
Figures and Tables
Fig. 1
(A) Gross appearance of the vulva . Pedulculated cystic mass arising from the left vulva. (B) Microscopic findings. Dilated lymphatic vessels, often cystic and ectatic, were lined by flattened endothelial cells with the paucicellular fibrous background in the mid and the deep dermis (hematoxylin-eosin, ×100).
References
1. Brown JV, Stenchever MA. Cavernous lymphangioma of the vulva. Obstet Gynecol. 1989; 73(5 Pt 2):877–879.
2. Haley JC, Mirowski GW, Hood AF. Benign vulvar tumors. Semin Cutan Med Surg. 1998; 17:196–204.
3. Bagga R, Dhaliwal LK, Gupta I, Kalra N, Rajwanshi A. Pedunculated cavernous lymphangioma of the vulva. Acta Obstet Gynecol Scand. 2004; 83:1095–1096.
4. Forsnes EV. Cavernous lymphangioma of the vulva: a case report. J Reprod Med. 2002; 47:1041–1043.
5. Gupta SC, Misra V, Gupta AK. Cavernous lymphangioma in the vulva. Trop Doct. 1998; 28:52.
6. Krebs HB, Schneider V, Radford WL. Congenital dysplastic angiopathy (Klippel-Trenaunay-Weber syndrome) with vulvar involvement: a case report. J Reprod Med. 1984; 29:215–218.
7. Noël JC, Fernandez-Aguilar S, Anaf V. Cavernous lymphangioma of the vulva. Acta Obstet Gynecol Scand. 2007; 86:378–379.
8. Watanabe T, Matsubara S, Yamaguchi T, Yamanaka Y. Cavernous lymphangiomas involving bilateral labia minora. Obstet Gynecol. 2010; 116:Suppl 2. 510–512.
9. Fletcher CD, Unni KK, Mertens F. Pathology and genetics of tumours of soft tissue and bone. Lyon: IARC Press;2002.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download