Abstract
Objective
To evaluate the effect of second-line conservative surgery on in vitro fertilization (IVF) outcome in comparison with IVF without second-line surgery in infertile women with ovarian endometrioma recurrence after primary conservative surgery.
Methods
In this retrospective cohort study, 121 consecutive IVF/intracytoplasmic sperm injection cycles that were performed after second-line surgery (n=53) or without second-line surgery (control group, n=68) between January 2006 and December 2011 in 121 infertile women with ovarian endometrioma(s) recurrence after primary conservative surgery for moderate to severe endometriosis were included. The two groups were compared in terms of controlled ovarian stimulation and IVF outcomes.
Results
There were no differences in patients' characteristics between the two groups. Total dose and days of gonadotropins administered were significantly higher in the second-line surgery group than in the control group (P<0.001, P=0.008). The numbers of oocytes retrieved, mature oocytes and grade 1 or 2 embryos were significantly lower in the second-line surgery group (P=0.007, P=0.001, P<0.001, respectively). Clinical pregnancy rate per cycle and embryo implantation rate were also significantly lower in the second-line surgery group of 24.5% and 11.8% compared with 48.5% and 25.3% in the control group (P=0.008, P=0.005, respectively).
Endometriosis is a chronic inflammatory gynecologic disease associated with chronic pelvic pain and infertility. The current treatment of endometriosis includes both medical and surgical methods. For women with moderate to severe endometriosis who hope to preserve fertility and conceive, conservative surgery is commonly chosen as a primary treatment. However, conservative surgery cannot often eradicate the disease and recurrence of endometriosis is common. Recurrence rate of endometriosis after primary surgery has been reported as high as 30% to 50% within 5 years after surgery [12]. In women seeking pregnancy, management of recurrent ovarian endometrioma is particularly one of clinical dilemmas, because surgical intervention can cause further damage to the already devastated ovarian tissue, thereby decreasing the ovarian reserve and reproductive performance significantly. Actually the pregnancy rate after second-line surgery for endometriosis has been reported to be almost half that after primary surgery [34].
The European Society of Human Reproduction and Embryology (ESHRE) guidelines in 2014 reported that cystectomy of ovarian endometrioma larger than 3 cm prior to treatment with assisted reproductive technology in infertile women does not improve pregnancy rates [5]. Nevertheless, the effect of ovarian endometrioma and previous surgical treatment for that before in vitro fertilization (IVF) treatment is still controversial. Moreover, the effect of second-line surgery prior to IVF treatment in infertile women with ovarian endometrioma recurrence remains open for debate. The ESHRE guidelines also recommended that the decision to proceed with surgery should be considered carefully if the woman has had previous ovarian surgery [5]. However, there are no well-designed controlled studies if second-line surgery for recurrent ovarian endometrioma before IVF has a beneficial or deleterious effect on ovarian response to controlled ovarian stimulation (COS) and IVF outcome. Therefore, we performed this study to investigate the effect of second-line conservative surgery on IVF outcome as compared with IVF without second-line surgery in infertile women with ovarian endometrioma recurrence after primary surgery.
The present retrospective cohort study included 121 consecutive IVF/intracytoplasmic sperm injection (ICSI) cycles that were performed in 121 infertile women with ovarian endometrioma(s) recurrence after primary conservative surgery for moderate to severe endometriosis between January 2005 and December 2011. Of 121 subjects, 53 patients underwent second-line surgery before IVF (second-line surgery group) and 68 patients underwent IVF treatment without second-line surgery (control group).
This study was approved by the institutional review board of the University of Ulsan College of Medicine, Asan Medical Center (IRB no. 2013-1090). The clinical information was obtained by chart review. If patients underwent two or more IVF/ICSI cycles after endometrioma recurrence during the study period, only the charts corresponding to the 1st IVF/ICSI cycle after endometrioma recurrence were reviewed and analyzed.
All subjects were between 28 and 41 years of age at the time of IVF treatment included in this study, and they had regular ovulatory cycles of 24 to 35 days in length and body mass index between 18 and 25 kg/m2. In addition, they underwent primary conservative surgery for infertility with moderate to severe endometriosis within 5 years prior to IVF treatment included in this study and endometrioma was confirmed pathologically at the time of primary surgery. After primary surgery, all patients included in this study failed to be pregnant and had recurrent ovarian endometriomas with a mean diameter of >3 cm that were diagnosed by transvaginal ultrasonography. Twenty-six of 53 women in the second-line surgery group and 35 of 68 women in the control group had undergone IVF treatment before ovarian endometrioma recurrence. Infertile women who had received more than 2 cycles of IVF before ovarian endometrioma recurrence were excluded from this study. Patients who had current endocrine abnormalities such as polycystic ovary syndrome and diabetes mellitus, history of previous hospitalization due to severe ovarian hyperstimulation syndrome, or history of previous (within 12 months) or current abuse of alcohol or drugs were also excluded from the present study.
Patients who did not achieve spontaneous pregnancy within 12 months from second-line surgery and/or had recurrent ovarian endometrioma >3 cm after second-line surgery underwent IVF/ICSI and they were included in the second-line surgery group. During the study period, 80 infertile women who met the inclusion and exclusion criteria underwent second-line surgery for recurrent ovarian endometrioma(s) and only five (6.3%) of them were spontaneously pregnant within 12 months after second-line surgery. Of 75 patients who failed to achieve spontaneous pregnancy within 12 months after second-line surgery, 53 infertile women received IVF treatment in our hospital and they were followed up and therefore included in the second-line surgery group of the present study. Twenty-three patients (43.4%) of 53 included in the second-line surgery group had recurrent ovarian endometriomas >3 cm in a mean diameter after follow-up of 24 months following second-line surgery. Patients included in the control group underwent IVF without any surgical intervention for ovarian endometrioma recurred after primary surgery.
Gonadotropin releasing hormone (GnRH) agonist long protocol or GnRH antagonist protocol was used for COS in all subjects. In the GnRH agonist long protocol, daily injection of a GnRH agonist 1 mg (leuprorelin acetate; Lorelin, Dongkook, Seoul, Korea) was initiated from the midluteal phase of the preceding menstrual cycle and was continued at least for 14 days, followed by a dose reduction to 0.5 mg daily. GnRH agonist 0.5 mg was continued daily up to day of human chorionic gonadotropin (hCG) injection. Ovarian stimulation was started with 150 to 300 IU of recombinant human follicle-stimulating hormone (rhFSH; Gonal-F, Merck Serono SA, Geneva, Switzerland) after establishing ovarian and uterine quiescence using vaginal ultrasound. The rhFSH dose was adjusted every 3 to 4 days according to the ovarian response. A recombinant hCG (rhCG; Ovidrel, Merck Serono SA) of 250 µg was injected to induce follicular maturation when one or more follicles reached a mean diameter of ≥18 mm. Oocyte retrieval was performed 35 to 36 hours after hCG injection, and one to three embryos were transferred into the uterus on the third day after oocyte retrieval. Vaginal progesterone gel (Crinone 8% 90 mg, Merck Serono SA) once daily was administrated from the day of oocyte retrieval for luteal support.
In the GnRH antagonist protocol, ovarian stimulation was commenced with 150 to 300 IU of rhFSH, from the third day of menstruation after establishing ovarian and uterine quiescence by using transvaginal ultrasound. The rhFSH dose was adjusted every 3 to 4 days according to the ovarian response. When the lead follicle reached a mean diameter of 13 to 14 mm, GnRH antagonist cetrorelix (Cetrotide, Merck Serono SA) at a dose of 0.25 mg/day was started and continued daily up to the day of hCG administration. When one or more follicles reached 18 mm or more in a mean diameter, a single subcutaneous bolus of 250 µg rhCG (Ovidrel, Merck Serono SA) was administered simultaneously with GnRH agonist 0.1 mg (Decapeptyl, Ferring, Malmö, Sweden). Oocyte retrieval and luteal support were performed in same manner with GnRH agonist long protocol.
After IVF or ICSI, one to three embryos were transferred into the uterus on the third day after oocyte retrieval. All patients received 90 mg of vaginal progesterone gel (Crinone gel 8%, Merck Serono SA) once daily from the day of oocyte retrieval for luteal phase support. The β-hCG serum levels were measured 11 days after embryo transfer. The β-hCG serum levels were measured by radioimmunoassay using a hCG MAIA clone kit (Serono Diagnostics, Woking, UK) with interassay and intraassay variances of <10% and 5%, respectively. Clinical pregnancy was defined as the presence of a gestational sac by ultrasonography, while miscarriage rate per clinical pregnancy was defined as the proportion of patients who failed to continue development before 20 weeks of gestation in all clinical pregnancies.
Mean values were expressed as mean±standard deviation. Student's t-test was used to compare mean values. Chi-square test and Fisher's exact test were used to compare fraction. Statistical significance was defined as P<0.05. All analyses were performed by using SPSS ver. 11.0 (SPSS Inc., Chicago, IL, USA).
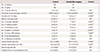
The second-line surgery and control groups were comparable with respect to patients' characteristics such as the age of patients, infertility duration, body mass index and the proportions of nullipara and patients who have undergone IVF before endometrioma recurrence was found after primary surgery (Table 1). However, total antral follicle count and serum anti-Müllerian hormone levels were significantly lower in the second-line surgery group than in the control group (P=0.002, P<0.001, respectively). The period from primary surgery to IVF treatment analyzed for this study was significantly longer in the second-line surgery group of 34.1±9.6 months compared with 24.2±8.5 months of the control group (P<0.001). The size of endometrioma on the day of oocyte retrieval was significantly smaller in the second-line surgery group (P<0.001) (Table 1).
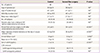
Total dose and days of gonadotropins administered were significantly higher in the second-line surgery group than in the control group (P<0.001, P=0.008, respectively). The numbers of oocytes retrieved, mature oocytes, fertilized oocytes, grade 1 or 2 embryos and frozen 2 pronucleus embryos were significantly lower in the second-line surgery group (P=0.007, P=0.001, P=0.001, P<0.001, P=0.003, respectively). Clinical pregnancy rate per cycle and embryo implantation rate were also significantly lower in the second-line surgery group of 24.5% and 12.3% compared with 48.5% and 25.8% in the control group (P=0.008, P=0.007, respectively) (Table 2).
Endometriosis is a troublesome disease that seriously compromises the female fertility and has high likelihood of recurrence after surgical treatment. The cumulative recurrence rate of endometriosis after conservative surgery has been recognized to be high and increase as the follow-up period gets longer [123]. The recurrence rates of pain and endometrioma after second-line surgery have been reported to be also comparable with those after primary surgery [6]. Ovarian endometrioma resection may be deleterious to residual oocyte and hormone function [78] and the overall pregnancy rate observed after a conservative surgery has been reported to be decreased [9]. Moreover, second-line surgery for endometrioma recurrence can worsen the reproductive performance [1011]. It has been reported that cumulative pregnancy rate after second-line surgery for recurrent endometriosis is significantly lower than those obtained after primary surgery [34]. Also the present study showed that 12-month cumulative spontaneous pregnancy rate after second-line surgery for recurrent endometrioma is only 6.3%. These results suggest that infertile women who undergo second-line surgery for recurrent ovarian endometrioma are very likely to receive IVF treatment for pregnancy. Therefore the effect of second-line surgery on IVF outcome is one of our great concerns. However, it is hard to find the well-controlled studies that investigated the impact of second-line surgery for recurrent ovarian endometrioma on IVF outcome.
In our study, ovarian response to COS after second-line surgery was significantly worse than that after primary surgery alone, although the size of endometrioma on the day of oocyte retrieval was significantly smaller in the second-line surgery group. Clinical pregnancy rate per cycle and embryo implantation rate were also significantly lower in the second-line surgery group. It is thought that primary cause of these results is a serious reduction of ovarian reserve by further detriment to already damaged ovarian tissue. Significantly lower antral follicle count and serum anti-Müllerian hormone levels in the second-line surgery group that were shown in this study support our hypothesis. In addition, recurrent endometriosis after primary surgery may exhibit particularly aggressive charactericstics and therefore, repeated surgery is more likely to damage the surrounding tissue of ovarian endometrioma, thereby leading to more severe and extensive adhesion around ovaries. These changes can result in the decrease of blood perfusion to the ovary, thereby worsening the ovarian response to COS. Another reason for deterioration of ovarian response to COS in the second-line surgery group can be further decrease of ovarian reserve by delayed trial of IVF. Actually, the period from primary surgery to 1st IVF cycle after endometrioma recurrence in this study was significantly longer in the second-line surgery group. For these reasons, many women who underwent second-line surgery for recurrent endometrioma appears to be finally need IVF treatment for getting pregnant.
In conclusion, our study demonstrated that ovarian response to COS and IVF outcome after second-line surgery is substantially worse than those in IVF cycles without secondline surgery in infertile women with ovarian endometrioma recurrence after primary surgery for moderate or severe endometriosis. Second-line surgery for recurrent ovarian endometriomas may give an adverse effect rather than any beneficial effect on IVF outcome. Therefore, second-line surgery should be determined carefully in infertile women with recurrent endometrioma after primary surgery and IVF treatment should be considered as an alternative to second-line surgery.
However, our study has a limitation to evaluate the effect of second-line surgery for recurrent endometrioma due to a small number of subjects available and their heterogenous characteristics due to its retrospective nature. Therefore, welldesigned controlled trials are required to confirm the results of our present study.
Figures and Tables
Table 2
Comparison of COS results and IVF/ICSI outcome
Values are mean±standard devition unless otherwise indicated.
COS, controlled ovarian stimulation; IVF, in vitro fertilization; ICSI, intracytoplasmic sperm injection; NS, not significant; EMT, endometrial thickness; hCG, human chorionic gonadotropin; PN, pronucleus; PR, pregnancy rate.
a)Chi-square test or Fisher's exact test; b)Student's t-test.
References
1. Guo SW. Recurrence of endometriosis and its control. Hum Reprod Update. 2009; 15:441–461.
2. Kikuchi I, Takeuchi H, Kitade M, Shimanuki H, Kumakiri J, Kinoshita K. Recurrence rate of endometriomas following a laparoscopic cystectomy. Acta Obstet Gynecol Scand. 2006; 85:1120–1124.
3. Vercellini P, Somigliana E, Vigano P, De Matteis S, Barbara G, Fedele L. The effect of second-line surgery on reproductive performance of women with recurrent endometriosis: a systematic review. Acta Obstet Gynecol Scand. 2009; 88:1074–1082.
4. Vercellini P, Somigliana E, Daguati R, Barbara G, Abbiati A, Fedele L. The second time around: reproductive performance after repetitive versus primary surgery for endometriosis. Fertil Steril. 2009; 92:1253–1255.
5. Dunselman GA, Vermeulen N, Becker C, Calhaz-Jorge C, D'Hooghe T, De Bie B, et al. ESHRE guideline: management of women with endometriosis. Hum Reprod. 2014; 29:400–412.
6. Fedele L, Bianchi S, Zanconato G, Berlanda N, Raffaelli R, Fontana E. Laparoscopic excision of recurrent endometriomas: long-term outcome and comparison with primary surgery. Fertil Steril. 2006; 85:694–699.
7. Benaglia L, Somigliana E, Vighi V, Ragni G, Vercellini P, Fedele L. Rate of severe ovarian damage following surgery for endometriomas. Hum Reprod. 2010; 25:678–682.
8. Loh FH, Tan AT, Kumar J, Ng SC. Ovarian response after laparoscopic ovarian cystectomy for endometriotic cysts in 132 monitored cycles. Fertil Steril. 1999; 72:316–321.
9. Koga K, Takemura Y, Osuga Y, Yoshino O, Hirota Y, Hirata T, et al. Recurrence of ovarian endometrioma after laparoscopic excision. Hum Reprod. 2006; 21:2171–2174.
10. Catenacci M, Sastry S, Falcone T. Laparoscopic surgery for endometriosis. Clin Obstet Gynecol. 2009; 52:351–361.
11. Diwadkar GB, Falcone T. Surgical management of pain and infertility secondary to endometriosis. Semin Reprod Med. 2011; 29:124–129.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download