Abstract
Objective
We investigated the features of endometrial hyperplasia with concurrent endometrial cancer that had been diagnosed by endometrial sampling. Further, we attempted to identify an accurate differential diagnostic method.
Methods
We retrospectively studied 125 patients who underwent a diagnostic endometrial biopsy or were diagnosed after the surgical treatment of other gynecological lesions, such as leiomyoma or polyps. Patients were diagnosed between January 2005 and December 2013 at Busan Paik Hospital. Clinical and histopathological characteristics were compared in patients who had atypical endometrial hyperplasia with and without concurrent endometrial cancer.
Results
The patients were grouped based on the final pathology reports. One hundred seventeen patients were diagnosed with endometrial hyperplasia and eight patients were diagnosed with endometrioid adenocarcinoma arising from atypical hyperplasia. Of the 26 patients who had been diagnosed with atypical endometrial hyperplasia by office-based endometrial biopsy, eight (30.8%) were subsequently diagnosed with endometrial cancer after they had undergone hysterectomy. The patients with endometrial cancer arising from endometrial hyperplasia were younger (39.1 vs. 47.2 years, P=0.0104) and more obese (body mass index 26.1±9.6 vs. 23.8±2.8 kg/m2, P=0.3560) than the patients with endometrial hyperplasia. The correlation rate between the pathology of the endometrial samples and the final diagnosis of endometrial hyperplasia was 67.3%.
Conclusion
In patients with atypical endometrial hyperplasia, the detection of endometrial cancer before hysterectomy can decrease the risk of suboptimal treatment. The accuracy of endometrial sampling for the diagnosis of concurrent endometrial carcinoma was much lower than that for atypical endometrial hyperplasia. Therefore, concurrent endometrial carcinoma should be suspected and surgical intervention should be considered in young or obese patients who present with atypical endometrial hyperplasia.
Endometrial hyperplasia is defined as histologically abnormal overgrowth of the endometrial glands and can be a precursor to cancer. Sustained stimulation by estrogen that is not opposed by progesterone can lead to an increased number of endometrial glands. There are several conditions that can induce the abnormal proliferation of endometrial glands. One example is polycystic ovary syndrome, which can occur in women of reproductive age, or obese women. Endometrial hyperplasia, particularly with atypia, is a significant concern clinically because it can be a precursor and marker of concurrent endometrial cancer [1].
The incidence rate of endometrial hyperplasia is dependent on both age and symptoms. In asymptomatic premenopausal women, the incidence of endometrial hyperplasia without atypia is <5% and the incidence of endometrial hyperplasia with atypia is <1% [2]. In contrast, the incidence of endometrial hyperplasia has been reported to be as high as 10% among premenopausal women with abnormal uterine bleeding [3]. The risk factors for endometrial hyperplasia are similar to those for type 1 endometrial cancers, which are estrogen-dependent endometrioid adenocarcinomas and are associated with a favorable prognosis [4]. In fact, approximately 80% to 85% of endometrial cancers are endometrioid carcinomas with minimal myometrial invasion that arise from atypical complex hyperplasia [56]. Approximately 30% to 40% of patients diagnosed with atypical hyperplasia may have concurrent adenocarcinoma, and the remaining 60% to 70% have a very high risk of cancer development [7]. Because the management and prognosis of endometrial hyperplasia and endometrial cancer are very different, differential diagnosis is important. Specifically, the accurate diagnosis of precancerous lesions of the endometrium and the exclusion of coexisting endometrial carcinomas are absolutely required for the optimal management of patients.
In general, endometrial hyperplasia is diagnosed by endometrial sampling with biopsy or curettage. However, it is unclear whether these methods can be used to accurately diagnose precancerous lesions of the endometrium [8]. Additionally, patients with endometrial intraepithelial neoplasia (EIN) or atypical hyperplasia that has been diagnosed by endometrial biopsy may be subsequently diagnosed as endometrial carcinoma based on the final analysis of the hysterectomy specimens. Therefore, the risk of suboptimal treatment can be decreased by detecting endometrial carcinoma accurately before hysterectomy in patients with endometrial hyperplasia.
The objectives of this study were to analyze the frequency of coexisting endometrial cancer in patients with atypical endometrial hyperplasia that had been diagnosed by endometrial sampling, and to identify an accurate differential diagnostic method by performing a literature review.
Between January 2005 and December 2013, 218 patients with endometrial hyperplasia were diagnosed by endometrial sampling with office-based biopsy, curettage, or an operation for the treatment of other gynecological lesions (such as leiomyoma or polyps) at the Department of Obstetrics and Gynecology, College of Medicine, Inje University, Busan Paik Hospital. Of these patients, 125 were managed as inpatients and 93 were treated as outpatients. The medical records of the 125 hospitalized patients were retrospectively reviewed. The clinicopathological data that were collected included the patient's age, symptoms, body mass index (BMI), parity, menopausal status, methods of diagnosis, and subsequent operation, such as total hysterectomy. BMI was calculated as weight in kilograms divided by height in meters squared. Menopause was defined as the absence of menstrual periods for 12 consecutive months. Endometrial hyperplasia was suspected when measurement revealed that the endometrial thickness was greater than 4 mm in a patient with postmenopausal bleeding or greater than 8 mm in a patient with premenopausal abnormal uterine bleeding. Transvaginal ultrasonography was used to determine the endometrial thickness, which was measured as the maximum anterior-posterior thickness of the endometrial echo on a long-axis transvaginal view of the uterus. None of the patients was receiving hormonal replacement therapy.
The histopathological reports for the endometrial samples and final excised specimens were reviewed. We compared the clinical and histopathological characteristics of patients with endometrial hyperplasia and those with endometrial cancer arising from atypical complex hyperplasia according to the final diagnosis. The histopathological diagnosis was based on the World Health Organization (WHO) classification criteria. The study was approved by the relevant institutional review board of Busan Paik Hospital.
Statistical analyses were performed using MedCalc ver. 14.8.1 (MedCalc Software, Mariakerke, Belgium). Categorical variables were compared using chi-square tests and Fisher's exact tests. The mean, median, and standard deviation were calculated for continuous variables, which were compared using t-tests and Pearson's correlation coefficients. The chi-square test was used to assess concordance. P<0.05 was considered statistically significant.
Between January 2005 and December 2013, 125 patients were hospitalized for the treatment of endometrial hyperplasia that had been diagnosed based on the pathological results of endometrial sampling, such as from office-based biopsy, curettage, or surgery for the treatment of other gynecologic lesions. Of these patients, 117 were diagnosed with endometrial hyperplasia and eight were diagnosed with endometrioid adenocarcinoma based on the final pathology. The patient characteristics and methods of diagnosis and treatment are shown in Table 1. The mean age of the patients was 46.8±10.0 years, the mean BMI was 23.7±4.1 kg/m2, and the most common symptom was intermenstrual bleeding (66.4%). Twenty-four percent of the patients were postmenopausal women. The patients were diagnosed by transvaginal sonography (TVS) and endometrial biopsy. However, 21 patients (16.8%) did not undergo endometrial sampling because endometrial hyperplasia had not been discovered until they underwent surgery. Of these 21 patients, 13 were diagnosed with endometrial hyperplasia after a hysterectomy had been performed for the treatment of myoma, adenomyosis, or endometrial polyps; 7 were diagnosed with simple endometrial hyperplasia after hysteroscopic polypectomy for the treatment of endometrial polyps; and 1 was diagnosed with simple endometrial hyperplasia after myomectomy of submucosal myoma. After endometrial hyperplasia had been diagnosed, 119 patients (95.2%) underwent surgical or medical treatment.
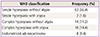
Using the WHO 1994 classification system, the endometrial lesions were divided into five groups after the histology of the case had been confirmed by the final pathology (Table 2).
The 104 patients with endometrial hyperplasia that had been diagnosed by endometrial sampling were divided into two groups. The first group consisted of the 58 patients who were diagnosed by office-based endometrial biopsy and the second consisted of the remaining 46 patients, who had been diagnosed by dilatation and curettage (D&C). We assessed the concordance rate between the diagnoses based on endometrial sampling and those based on the final pathology. Seventy-eight patients were diagnosed with endometrial hyperplasia without atypia based on endometrial sampling and 26 patients were diagnosed with atypical endometrial hyperplasia based on endometrial sampling. Among the 104 patients who were diagnosed with endometrial hyperplasia based on the final pathology, the histological results of the endometrial sampling were largely in agreement with the final hysterectomy specimens or repeat D&C in 70 patients (67.3%). The diagnoses that had been based on endometrial samples from office-based endometrial biopsies and D&C showed concordance rate of 60.3% and 76.1% with the final diagnosis, respectively (P=0.1364).
Of the 26 patients with atypical endometrial hyperplasia that had been diagnosed by endometrial sampling, eight were subsequently diagnosed with endometrial cancer based on the final hysterectomy specimens. These patients had atypical endometrial hyperplasia with concurrent endometrial carcinoma. The rate of coexisting endometrial cancer in patients with a diagnosis of atypical endometrial hyperplasia was therefore 30.8% (8/26). Importantly, the histological results from the endometrial sampling were highly inconsistent with the final pathology for the eight patients with endometrial cancer. Five of the patients had undergone office-based endometrial biopsy and three had undergone D&C. The patients with concurrent endometrial carcinoma demonstrated favorable prognostic features with histologic grade 1 and type 1 (endometrioid) carcinomas. None of these eight patients showed serosal invasion or ovarian, tubal, or omental involvement.
As shown in Table 3, we compared the clinical characteristics of patients who had atypical endometrial hyperplasia alone and patients who had atypical endometrial hyperplasia with concurrent endometrial carcinoma in the resected uteri, who were diagnosed with atypical endometrial hyperplasia on endometrial sampling. The mean age of the patients diagnosed with endometrial carcinoma was much lower than that of patients diagnosed with atypical endometrial hyperplasia alone (39.1 vs. 47.2 years, P=0.0104). In addition, the mean BMI of the patients with endometrial cancer was higher than that of patients with atypical endometrial hyperplasia alone (26.1±9.6 vs. 23.8±2.8 kg/m2), although the difference was not statistically significant. As measured using TVS, the endometrial thickness in women with endometrial cancer was greater than that in women with atypical hyperplasia alone (10.0±4.9 vs. 13.0±8.9 mm), but this difference was also non-significant. The degree of concordance between the surgical biopsy results and the final pathology was much higher in the patients with atypical endometrial hyperplasia alone than in those who also had concurrent endometrial cancer (72.2% vs. 0%, P=0.00164).
The standard treatment for early-stage endometrial cancer is hysterectomy with bilateral salpingo-oophorectomy, as well as pelvic and para-aortic lymph node sampling. However, primary hormonal therapy with progesterone is an alternative to surgical treatment for younger patients who wish to preserve their fertility [9]. In our study, office-based biopsy and D&C showed 60.3% and 70.6% concordance with the final diagnosis, respectively. Accordingly, the diagnosis of atypical endometrial hyperplasia is difficult. Nonetheless, it remains important to diagnose this condition because it can progress to cancer.
The positive predictive value of atypical endometrial hyperplasia diagnosed by endometrial sampling has varied widely in previous reports, ranging 6% to 63% [101112]. In our study, the positive predictive value of endometrial sampling for diagnosing atypical endometrial hyperplasia was 72.2 % (95% confidence interval, 46.5 to 90.3). Therefore, additional diagnostic testing is needed to accurately diagnose atypical endometrial hyperplasia.
In a recent report on patients diagnosed with atypical endometrial hyperplasia [13], the rate of concurrent endometrial cancer was high, with an overall average of 37%. Moreover, this rate increased to 40% to 48% in recent cases that were diagnosed in routine practice. In our study, we observed a somewhat lower rate of coexisting endometrial cancer in patients who had been diagnosed with atypical endometrial hyperplasia (30.8%); nonetheless, this rate remains high enough to suggest that differential diagnostic techniques are required to identify concurrent endometrial cancer among those patients who have been diagnosed preoperatively with atypical endometrial hyperplasia.
Regarding potential risk factors for coexisting endometrial cancer, our study's results suggest that obesity and age warrant further investigation. In our study cohort, the mean BMI was 23.7 kg/m2, which was not particularly high. We compared the mean BMIs of patients with concurrent endometrial cancer and atypical endometrial hyperplasia and found that they were 26.1 and 23.8 kg/m2, respectively. This result showed that patients with concurrent endometrial cancer were more obese than patients with atypical endometrial hyperplasia. However, the difference was not statistically significant, perhaps as a consequence of the small number of patients that were included in this study. In another recent study [11], a higher BMI was associated with an elevated risk of concomitant endometrial carcinoma. The mean age of patients with endometrial hyperplasia was 46.8 years overall, while the patients with concurrent endometrial cancer were generally younger than those with atypical endometrial hyperplasia (39.1 vs. 47.2 years, P=0.0104).
In our study, the concordance rate between diagnoses based on endometrial biopsy specimens and final pathology was much lower for atypical endometrial hyperplasia with concurrent endometrial cancer than for atypical endometrial hyperplasia alone (0% vs. 72.2%, P=0.00164). In our study, the concordance rate between the endometrial sample diagnosis and the final diagnosis was lower for endometrial sampling that had been performed via office-based endometrial biopsy. Therefore, although atypical endometrial hyperplasia was discovered in office-based endometrial biopsies, more aggressive therapies than treatment with medication alone should be considered. Goldstein [14] described the stepwise evaluation of the endometrium in patients with abnormal uterine bleeding. They concluded that TVS and sonohysterography could be used to triage patients effectively based on the following criteria: the absence of an anatomic lesion; the presence of a global lesion, such as a diffuse and proliferative endometrium; or the absence of focal lesions or focal abnormalities, such as polyps or carcinoma. In such cases, an invasive procedure would be required following TVS, such as a blind biopsy for global lesions or a hysteroscopy for focal endometrial processes.
Because focal lesions are often missed on office-based endometrial sampling, it has been recommended that patients at high risk undergo D&C before a hysterectomy [1516]. However, even with D&C, endometrial cancer will be missed in as many as 18% of patients with atypical endometrial hyperplasia [15]. It is clear that D&C does not completely exclude the possibility of concurrent endometrial carcinoma [17]. Therefore, a patient with atypical endometrial hyperplasia may have to undergo hysterectomy, depending on her age and the priority that she places on the preservation of reproductive function.
To accurately diagnose a patient with concurrent endometrial cancer, both a diagnostic method and a pathological classification are important. The greatest problem with the WHO 1994 classification system is that it relies upon relatively subjective histological criteria, resulting in relatively low interobserver agreement and reproducibility among pathologists [18]. In a large prospective multi-institutional cohort study of atypical complex endometrial hyperplasia diagnosed by community pathologists [18], a pathology review panel of 3 gynecologic pathologists agreed with the initial diagnosis in only 38% of cases. Baak et al. [19] and Salman et al. [1] have proposed that the EIN classification is more accurate than the WHO classification for identifying precancerous lesions. The EIN system is also better at identifying women with benign changes that were initially thought to be high risk according to the WHO classification [1].
There are several limitations in this study including its retrospective design, a small sample size, and the fact that it was conducted at a single institution. The small sample size may affect the power and significance of the findings.
In conclusion, the risk of concurrent malignancy was 30.8% in patients who had been diagnosed with atypical endometrial hyperplasia based on surgical biopsy specimens. As compared with office-based endometrial sampling, D&C provided more accurate diagnoses of atypical endometrial hyperplasia. However, neither approach constituted an appropriate method for diagnosing concurrent endometrial cancer. Our results tend to suggest that concurrent endometrial carcinoma should be suspected in patients with atypical endometrial hyperplasia who are younger and more obese than is typical for this condition; surgical intervention should be considered for these patients. Finally, we recommend using the EIN classification for endometrial lesions because it is more likely to successfully identify cancerous lesions than the WHO classification.
Figures and Tables
References
1. Salman MC, Usubutun A, Boynukalin K, Yuce K. Comparison of WHO and endometrial intraepithelial neoplasia classifications in predicting the presence of Coexistent malignancy in endometrial hyperplasia. J Gynecol Oncol. 2010; 21:97–101.
2. Gol K, Saracoglu F, Ekici A, Sahin I. Endometrial patterns and endocrinologic characteristics of asymptomatic menopausal women. Gynecol Endocrinol. 2001; 15:63–67.
3. Ash SJ, Farrell SA, Flowerdew G. Endometrial biopsy in DUB. J Reprod Med. 1996; 41:892–896.
4. Jick SS, Walker AM, Jick H. Estrogens, progesterone, and endometrial cancer. Epidemiology. 1993; 4:20–24.
5. Sherman ME. Theories of endometrial carcinogenesis: a multidisciplinary approach. Mod Pathol. 2000; 13:295–308.
6. Saso S, Chatterjee J, Georgiou E, Ditri AM, Smith JR, Ghaem-Maghami S. Endometrial cancer. BMJ. 2011; 343:d3954.
7. Mills AM, Longacre TA. Endometrial hyperplasia. Semin Diagn Pathol. 2010; 27:199–214.
8. Stock RJ, Kanbour A. Prehysterectomy curettage. Obstet Gynecol. 1975; 45:537–541.
9. Niwa K, Tagami K, Lian Z, Onogi K, Mori H, Tamaya T. Outcome of fertility-preserving treatment in young women with endometrial carcinomas. BJOG. 2005; 112:317–320.
10. Agostini A, Cravello L, Shojai R, Schaeffer V, Bretelle F, Roger V, et al. Risk of finding an endometrial cancer when atypical hyperplasia was incidentally diagnosed on hysteroscopic resection products. Eur J Obstet Gynecol Reprod Biol. 2002; 103:58–59.
11. Chen YL, Cheng WF, Lin MC, Huang CY, Hsieh CY, Chen CA. Concurrent endometrial carcinoma in patients with a curettage diagnosis of endometrial hyperplasia. J Formos Med Assoc. 2009; 108:502–507.
12. Hahn HS, Chun YK, Kwon YI, Kim TJ, Lee KH, Shim JU, et al. Concurrent endometrial carcinoma following hysterectomy for atypical endometrial hyperplasia. Eur J Obstet Gynecol Reprod Biol. 2010; 150:80–83.
13. Rakha E, Wong SC, Soomro I, Chaudry Z, Sharma A, Deen S, et al. Clinical outcome of atypical endometrial hyperplasia diagnosed on an endometrial biopsy: institutional experience and review of literature. Am J Surg Pathol. 2012; 36:1683–1690.
14. Goldstein SR. Modern evaluation of the endometrium. Obstet Gynecol. 2010; 116:168–176.
15. Suh-Burgmann E, Hung YY, Armstrong MA. Complex atypical endometrial hyperplasia: the risk of unrecognized adenocarcinoma and value of preoperative dilation and curettage. Obstet Gynecol. 2009; 114:523–529.
16. McKenney JK, Longacre TA. Low-grade endometrial adenocarcinoma: a diagnostic algorithm for distinguishing atypical endometrial hyperplasia and other benign (and malignant) mimics. Adv Anat Pathol. 2009; 16:1–22.
17. Armstrong AJ, Hurd WW, Elguero S, Barker NM, Zanotti KM. Diagnosis and management of endometrial hyperplasia. J Minim Invasive Gynecol. 2012; 19:562–571.
18. Zaino RJ, Kauderer J, Trimble CL, Silverberg SG, Curtin JP, Lim PC, et al. Reproducibility of the diagnosis of atypical endometrial hyperplasia: a Gynecologic Oncology Group study. Cancer. 2006; 106:804–811.
19. Baak JP, Mutter GL, Robboy S, van Diest PJ, Uyterlinde AM, Orbo A, et al. The molecular genetics and morphometry-based endometrial intraepithelial neoplasia classification system predicts disease progression in endometrial hyperplasia more accurately than the 1994 World Health Organization classification system. Cancer. 2005; 103:2304–2312.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download