Abstract
Objective
Appropriate gestational weight gain (GWG) is important in diabetic women. Current GWG guideline is for US general population, but not specific for diabetic women. We compared the effect of GWG on perinatal outcomes between diabetic and non-diabetic women.
Methods
Fifty two hundred and twelve women who delivered live singleton infants at Korea University Medical Center from January 2009 to December 2013 were included. One hundred twenty-nine overt diabetes women and 322 gestational diabetes women were categorized as diabetic women, and the others were categorized as none-diabetic women. 5,212 women were categorized by GWG (low 1,081; adequate 2,102; or high 2,029; according to the 2009 Institute of Medicine guidelines), and each of the 3 GWG groups was categorized into 2 groups; diabetic or non-diabetic women. And then, we compared perinatal outcomes between diabetic and non-diabetic groups.
Results
In each 3 GWG groups, primary cesarean section delivery, high birth weight, and large for gestational age rates were significantly higher in diabetic women than non-diabetic women. Only in adequate GWG group, preterm birth rate was significantly higher in diabetic women than non-diabetic women.
Conclusion
Our study shows that diabetic women had higher rates of adverse perinatal outcomes than non-diabetic women, although they achieved same GWG. It suggests that current GWG guideline may not be adequate for diabetic women, and that diabetic women may need more strict GWG control than normal population.
It is known that maternal pre-pregnancy body mass index (BMI), rate of weight gain, and total gestational weight gain (GWG) are closely associated with maternal and neonatal outcomes [123]. High GWG increases maternal risk of cesarean section (CS) delivery, pregnancy-related hypertension, and gestational diabetes (GDM) [2]. GWG also impacts the neonate, as high GWG increases risk of high birth weight (HBW), and, as low GWG increases risk of low birth weight (LBW), and preterm birth.
In 2009, the Institute of Medicine (IOM) revised their GWG guidelines, and these guidelines have been used as a current recommendation of GWG [3]. IOM 2009 guidelines are for the general obstetrical population in the United States, but application on subpopulations of pregnant women has not been evaluated extensively, especially diabetic women.
Diabetes during pregnancy, GDM or pregestational diabetes (overt diabetes), is associated with adverse obstetrical outcomes [45678910111213]. Diabetes increases the risk of preeclampsia, CS delivery, congenital malformation, spontaneous abortion, macrosomia, polyhrdramnios, and preterm birth. Adequate GWG is important for diabetic women to prevent adverse outcomes [1415], which is one of the goals of medical nutritional therapy and exercise.
Maternal diabetes and obesity are independently associated with adverse pregnancy outcomes, and their combination has a greater impact than either disorder alone [816]. IOM 2009 GWG guidelines, however, are for general obstetrical population, but applicability of these GWG targets to diabetic women is controversial [3].
To examine whether current GWG guidelines are sufficient for diabetic women, we compared the effect of GWG on perinatal outcomes between diabetic and non-diabetic women.
We conducted a retrospective cohort study of 5,840 women who delivered a live singleton infant at the Korea University Medical Center from January 2009 to December 2013. Patients who did not know their pre-pregnancy weight, who did not take glucose tolerance test, or who did not receive proper antenatal care were excluded. After exclusion, data of total 5,212 women were analyzed. Fifty two hundred and twelve women consisted of 322 GDM patients, 129 overt diabetes patients, and 4,761 non-diabetic patients. GDM and overt diabetes patients were categorized in "diabetic women" group, and the others were categorized in "non-diabetic women" group. All women were categorized into 3 GWG groups according to IOM 2009 guidelines; low GWG, adequate GWG, and high GWG.
Each of the 3 GWG groups was categorized into 2 subgroups; diabetic or non-diabetic women. And then, we compared perinatal outcomes between the 2 subgroups. In 1,081 low GWG women, 126 diabetic women were compared with 955 non-diabetic women. In 2,102 adequate GWG women, 137 diabetic women were compared with 1,965 non-diabetic women. In 2,029 high GWG women, 188 diabetic women were compared with 1,841 non-diabetic women.
GDM was defined as diabetes which is diagnosed in pregnancy by two step oral glucose tolerance test (OGTT) (50 g OGTT for screening test, and 100 g OGTT for diagnostic test). GDM was diagnosed if two or more plasma glucose levels met or exceeded the following thresholds: fasting glucose concentration of 95 mg/dL, 1-hour glucose concentration of 180 mg/dL, 2-hour glucose concentration of 155 mg/dL, or 3-hour glucose concentration of 140 mg/dL. Overt diabete was defined as a history of diabete. BMI was calculated by dividing weight in kilograms by the square of height in meters. Prepregnancy BMI was categorized as underweight (BMI <18.5 kg/m2), normal weight (18.5≤ BMI <25 kg/m2), overweight (25≤ BMI <30 kg/m2), or obese (BMI ≥30 kg/m2) by World Health Organization classification. Adequacy of GWG was defined according to the maternal pre-pregnancy BMI status and the IOM 2009 GWG recommendations; 12.5 to 18 kg total weight gain, or 0.44 to 0.58 kg/wk rate of weight gain in underweight women, 11.5 to 16 kg total weight gain, or 0.35 to 0.50 kg/wk rate of weight gain in normal weight wome n, 7 to 11.5 kg total weight gain, or 0.23 to 0.33 kg/wk rate of weight gain in overweight women, and 5 to 9 kg total weight gain, or 0.17 to 0.27 kg/wk rate of weight gain in obese women. We used the guidelines of weight gain rate (kg/wk) to correct the effect of gestational age (GA) to GWG.
Perinatal outcomes assessed were primary CS delivery, preterm labor, preterm premature rupture of membranes (PPROM), and preterm birth as the maternal outcomes, and LBW, HBW, small for gestational age (SGA), large for gestational age (LGA), low Apgar score, and admission to neonatal intensive care unit (NICU) as the neonatal outcomes. Preterm labor was defined as presence of uterine contractions of sufficient frequency and intensity to enable progressive cervical effacement and dilation prior to term gestation. PPROM was defined as membrane rupture prior to term gestation. LBW was defined as birth weight less than 2,500 g, and HBW was defined as birth weight more than 4,000 g. SGA was defined as birth weight below the 10th percentile for GA, and LGA was defined as birth weight greater than the 90th percentile for GA. GA was estimated by ultrasound measurement of crown-rump length in first trimester. When we diagnosed SGA or LGA, GA was rounded off to the nearest weeks to use birth weight percentile table made by Doubilet et al. [17]. Low Apgar score was defined as below 7 in 1-minute or 5-minutes Apgar score.
Data are expressed as the mean±standard deviation for continuous variables, and data for the categorical variables are expressed as the number and the percentage of patients. The chi-square test was used for the categorical variables of the two groups, and the Mantel-Haenszel chi-square test was used to adjust potential confounding factors. The independent samples t-test was used to compare continuous variables between the two groups. A P-value <0.05 was considered statistically significant.
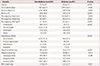
In the study population (n=5,212), diabetic women were 451, and non-diabetic women were 4,761 (Table 1). Mean age was older in the diabetic group than the non-diabetic group (33.6±4.3 vs. 32.0±4.5, P<0.001). The diabetic group have higher rate of multiparous pregnancy (50.8 vs. 45.9, P=0.049), and previous history of CS (31.7 vs. 18.3, P<0.001). Pre-pregnancy height was not significantly different between the two groups, but pre-pregnancy weight and BMI were higher in the diabetic group. GWG was higher in the non-diabetic group, but weight at delivery was higher in the diabetic group. Using IOM targets as reference, rate of adequate GWG was similar between the two groups, but fetal birth weight was higher in the diabetic group than the non-diabetic group (3.01±0.77 vs. 2.90±0.72, P=0.001). Mean GA was shorter in the diabetic group (259.7±20.2 vs. 262.9±22.2, P=0.002).
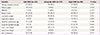
We categorized the study population into three GWG groups; low, adequate, and high GWG by IOM 2009. First, we compared perinatal outcomes among GWG groups in diabetic women (Table 2). The results showed tendency that higher GWG group had higher rates of primary CS delivery and LGA, and that lower GWG group had higher rates of LBW and SGA. However, the other outcomes were not significantly different among GWG groups.
Then perinatal outcomes were compared between diabetic and non-diabetic women in each GWG groups, respectively (Table 3). We found that primary CS delivery rate was higher in diabetic women, even though both diabetic and non-diabetic women belonged to same GWG group; 40.2% vs. 29.4% in low GWG group, 48.4% vs. 33.9% in adequate GWG group, 58.5% vs. 43.7% in high GWG group, respectively. The results were similar after adjustment of maternal age and parity. The other perinatal outcomes were also compared. In each 3 GWG groups, rates of HBW and LGA were significantly higher in diabetic women than non-diabetic women. In the low GWG group, NICU admission rate was higher in non-diabetic women. In the adequate GWG group, however, NICU admission rate was higher in diabetic women. In the high GWG group, there was no significant difference between non-diabetic and diabetic women. In the adequate GWG group, PPROM, preterm birth, and low 1 minute Apgar score rates were higher in diabetic women. In the high GWG group, PPROM rate was higher in diabetic women, but LBW and SGA rates were higher in non-diabetic women. The other outcomes were not significantly different between non-diabetic and diabetic women. The results were similar after adjustment of maternal age and parity.
To adjust for pre-pregnancy BMI as potential confounding factor, we also compared perinatal outcomes between non-diabetic and diabetic women in normal BMI group (Table 4). In the low GWG group, preterm birth and NICU admission rates were higher in non-diabetic women. In the adequate GWG group, primary CS delivery, preterm birth, HBW, and LGA rates were higher in diabetic women. In the high GWG group, primary CS delivery, preterm labor, and LGA rates were higher in diabetic women. The results were similar after adjustment of maternal age and parity.
Currently IOM guidelines are often used as ideal GWG, but there are no weight gain guidelines specific for diabetic women [18192021]. So, currently, the GWG goal of diabetic women was same as non-diabetic women. We found that rates of some adverse perinatal outcomes were higher in high GWG or low GWG groups (primary CS delivery, LBW, SGA, and LGA). These results suggest that adequate GWG is not only important for non-diabetic women, but also for diabetic women. But, we found that primary CS delivery, HBW, and LGA rates were significantly higher in diabetic women than non-diabetic women, although diabetic women achieved their recommended (adequate) GWG. We also found similar results in pre-pregnancy normal BMI women. These results suggest that diabetic condition is independently associated with increased risk of adverse perinatal outcomes, and that current IOM GWG goal is insufficient for diabetic women.
Although it was not constant trend, some other adverse perinatal outcomes were increased in diabetic women than non-diabetic women. But, in low GWG group, NICU admission rate was higher in non-diabetic women than diabetic women. This result may be associated with fetal birth weight. Previous study showed that singletons born to women with low total GWG have higher risks of preterm birth and LBW [22]. In low GWG group, mean fetal birth weight of diabetic women was 2.84 kg, and non-diabetic women was 2.72 kg, but it was not significantly different. Mean fetal birth weight of total low GWG group (diabetic and non-diabetic women) was 2.73 kg, and it was significantly lower than high or adequate GWG groups (2.97 and 2.92 kg). We used multivariate logistic regression to analyze risk factors of NICU admission in low GWG group. Multivariate binary logistic regression analysis showed that preterm birth (P<0.001), LBW (P<0.001), and maternal diabetes (P=0.049) were significantly associated with increased risk of NICU admission, but SGA, HBW, and LGA were not significantly associated. Although it was not significantly different, mean fetal birth weight was lower and LBW rate was higher in non-diabetic women. These may be associated with increased NICU admission rate of non-diabetic women in low GWG group. These results also imply that specific weight gain guideline may be needed for diabetic women.
In addition, we evaluate the risk of primary CS along the whole range of maternal weight gain to establish optimal GWG for normal weight BMI diabetic women by using similar method with previous study [23]. The number of individuals in each weight gain class was compared with the number of individuals in all other weight gain classes, and optimal weight gain range was based on significant risk estimates below 1 for each maternal weight gain. According to the results, possible optimal weight gain range in normal weight BMI diabetic women was 9 to 13 kg, but estimates of 95% confidence intervals were not statistically significant. The other BMI groups of this study could not be evaluated because study population number was too small to do this analysis, and it was our limitation of the study. Currently IOM recommended GWG in normal weight BMI group is 11.5 to 16.0 kg. Although it was not statistically significant meaningful, this possible optimal weight gain range (9 to 13 kg) may suggest that diabetic women need stricter GWG control than normal population in spite of same BMI. Thus, further large population studies are needed to evaluate and estimate adequate GWG goals in diabetic women.
Limitation of this study is that type of therapy of diabetes and degree of diabetes control may be associated with perinatal outcomes. However, the purpose of this study was to suggest the necessity of specific GWG guidelines for diabetic women. Considering the impact of specific situation may be needed, but that may also make it unnecessarily complicated to make guidelines for diabetic women.
In summary, our study shows that diabetic women had higher primary CS delivery, HBW and LGA rate than non-diabetic women, although they achieved same GWG. It suggests that current GWG guideline may be not adequate for diabetic women, and that diabetic women may need stricter GWG control than general population.
Figures and Tables
References
1. Bloomgarden ZT. Gestational diabetes mellitus and obesity. Diabetes Care. 2010; 33:e60–e65.
2. Viswanathan M, Siega-Riz AM, Moos MK, Deierlein A, Mumford S, Knaack J, et al. Outcomes of maternal weight gain. Evid Rep Technol Assess (Full Rep). 2008; (168):1–223.
3. Institute of Medicine (US) and National Research Council (US) Committee to Reexamine IOM Pregnancy Weight Guidelines. Rasmussen KM, Yaktine AL, editors. Weight gain during pregnancy: reexamining the guidelines. Washington, DC: National Academies Press;2009.
4. Jensen DM, Korsholm L, Ovesen P, Beck-Nielsen H, Molsted-Pedersen L, Damm P. Adverse pregnancy outcome in women with mild glucose intolerance: is there a clinically meaningful threshold value for glucose? Acta Obstet Gynecol Scand. 2008; 87:59–62.
5. Hillier TA, Pedula KL, Schmidt MM, Mullen JA, Charles MA, Pettitt DJ. Childhood obesity and metabolic imprinting: the ongoing effects of maternal hyperglycemia. Diabetes Care. 2007; 30:2287–2292.
6. Jensen DM, Damm P, Sorensen B, Molsted-Pedersen L, Westergaard JG, Klebe J, et al. Clinical impact of mild carbohydrate intolerance in pregnancy: a study of 2904 nondiabetic Danish women with risk factors for gestational diabetes mellitus. Am J Obstet Gynecol. 2001; 185:413–419.
7. Pettitt DJ, Knowler WC, Baird HR, Bennett PH. Gestational diabetes: infant and maternal complications of pregnancy in relation to third-trimester glucose tolerance in the Pima Indians. Diabetes Care. 1980; 3:458–464.
8. HAPO Study Cooperative Research Group. Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U, et al. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008; 358:1991–2002.
9. Sermer M, Naylor CD, Gare DJ, Kenshole AB, Ritchie JW, Farine D, et al. Impact of increasing carbohydrate intolerance on maternal-fetal outcomes in 3637 women without gestational diabetes: the Toronto Tri-Hospital Gestational Diabetes Project. Am J Obstet Gynecol. 1995; 173:146–156.
10. Pettitt DJ, Knowler WC. Long-term effects of the intrauterine environment, birth weight, and breast-feeding in Pima Indians. Diabetes Care. 1998; 21:Suppl 2. B138–B141.
11. Ferrara A, Weiss NS, Hedderson MM, Quesenberry CP Jr, Selby JV, Ergas IJ, et al. Pregnancy plasma glucose levels exceeding the American Diabetes Association thresholds, but below the National Diabetes Data Group thresholds for gestational diabetes mellitus, are related to the risk of neonatal macrosomia, hypoglycaemia and hyperbilirubinaemia. Diabetologia. 2007; 50:298–306.
12. Dodd JM, Crowther CA, Antoniou G, Baghurst P, Robinson JS. Screening for gestational diabetes: the effect of varying blood glucose definitions in the prediction of adverse maternal and infant health outcomes. Aust N Z J Obstet Gynaecol. 2007; 47:307–312.
13. Sacks DA, Greenspoon JS, Abu-Fadil S, Henry HM, Wolde-Tsadik G, Yao JF. Toward universal criteria for gestational diabetes: the 75-gram glucose tolerance test in pregnancy. Am J Obstet Gynecol. 1995; 172(2 Pt 1):607–614.
14. Cheng YW, Chung JH, Kurbisch-Block I, Inturrisi M, Shafer S, Caughey AB. Gestational weight gain and gestational diabetes mellitus: perinatal outcomes. Obstet Gynecol. 2008; 112:1015–1022.
15. Rasmussen KM, Catalano PM, Yaktine AL. New guidelines for weight gain during pregnancy: what obstetrician/gynecologists should know. Curr Opin Obstet Gynecol. 2009; 21:521–526.
16. Catalano PM, McIntyre HD, Cruickshank JK, McCance DR, Dyer AR, Metzger BE, et al. The hyperglycemia and adverse pregnancy outcome study: associations of GDM and obesity with pregnancy outcomes. Diabetes Care. 2012; 35:780–786.
17. Doubilet PM, Benson CB, Nadel AS, Ringer SA. Improved birth weight table for neonates developed from gestations dated by early ultrasonography. J Ultrasound Med. 1997; 16:241–249.
18. Barnes RA, Edghill N, Mackenzie J, Holters G, Ross GP, Jalaludin BB, et al. Predictors of large and small for gestational age birthweight in offspring of women with gestational diabetes mellitus. Diabet Med. 2013; 30:1040–1046.
19. Horosz E, Bomba-Opon DA, Szymanska M, Wielgos M. Maternal weight gain in women with gestational diabetes mellitus. J Perinat Med. 2013; 41:523–528.
20. Morisset AS, Tchernof A, Dube MC, Veillette J, Weisnagel SJ, Robitaille J. Weight gain measures in women with gestational diabetes mellitus. J Womens Health (Larchmt). 2011; 20:375–380.
21. Ouzounian JG, Hernandez GD, Korst LM, Montoro MM, Battista LR, Walden CL, et al. Pre-pregnancy weight and excess weight gain are risk factors for macrosomia in women with gestational diabetes. J Perinatol. 2011; 31:717–721.
22. Han Z, Lutsiv O, Mulla S, Rosen A, Beyene J, McDonald SD, et al. Low gestational weight gain and the risk of preterm birth and low birthweight: a systematic review and meta-analyses. Acta Obstet Gynecol Scand. 2011; 90:935–954.
23. Cedergren MI. Optimal gestational weight gain for body mass index categories. Obstet Gynecol. 2007; 110:759–764.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download