Abstract
Uterine arterial pseudoaneurysm is a very rare condition usually associated with postpartum hemorrhage. It almost never occurs after cervical conization; however, since ruptured pseudoaneurysm could be life threatening, we should consider the possibility of vascular injury such as pseudoaneurysm when we find a patient with vaginal bleeding after the process of surgical operation. Emergency arterial embolization is a well established therapeutic option to control the ruptured pseudoaneurysm. This is a case report of uterine arterial pseudoaneurysm causing intra-abdominal bleeding followed by cervical conization, which was successfully treated by uterine artery embolization.
Cervical conization is a rapid and relatively safe surgical method. Bleeding after cervical conization is a common complication of this procedure, but the blood loss is usually not fatal [1]. The Uterine arterial pseudoaneurysm (UAP) is rare but generally outbreaks subsequent to cesarean section, uterine curettage or vaginal delivery. However, it is very rare after cervical conization [2]. This is a case report of UAP causing intra-abdominal and vaginal bleeding after cervical conization.
A 32-year-old woman, gravida 2, para 1, abortion 1, was referred for vaginal bleeding after the cervical conization. The patient underwent cervical knife conization at a local hospital. The confirmed pathologic diagnosis was 'carcinoma in situ with glandular involvement.' During conization there was excessive bleeding from inside of cervix, gynecologist from private clinic performed multiple suturing bleeding site in the cervix. After conization, only a small amount of vaginal spotting lasted for the first few days. However, ten days later, the bleeding suddenly increased and abdominal pain started.
On physical examination, the patient had blood pressure 100/60 mmHg, heart rate 64 beats/min, respiratory rate 18 breaths/min, and body temperature 36.8 ℃. The abdomen was soft and not distended. However she had tenderness and also rebound tenderness on her lower part of abdomen. On the speculum examination, multiple suture materials were found on the cervix and the bleeding was continuing.
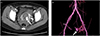
On the laboratory finding, the hemoglobin level was 11.4 g/dL and the other findings were within normal range. Transvaginal ultrasonography revealed a hypoechoic lesion in the cervix (Fig. 1A) and both of the ovaries were normal and color doppler ultrasonography demonstrated blood flow within the hypoechoic lesion (Fig. 1B).
Abdomen and pelvic angiographic computed tomography (CT) showed that an aneurysmal sac from the left uterine artery with a large amount of hemoperitoneum and hematometra (Fig. 2). Therefore, we decided to perform an emergency embolization. Embolization of the cervicovaginal branch of the left uterine artery was successfully performed with gelfoam and PVA particle, and the vaginal bleeding stopped.
At the routine follow-up visit after a week and a month, no additional bleeding was found. After one month follow-up visit, through the ultrasonography, pelvic cavity fluid collection have markedly decreased.
UAP is a very rare condition and usually associated with postpartum hemorrhage but usually not after cervical conization. To the best of our knowledge, this is the very unusual case report of UAP associated with cervical conization.
Pseudoaneurysm is a well known complication of vascular injury. It is an extra luminal collection of blood with turbulent flow that communicates with flowing arterial blood through a defect in the arterial wall. When the uterine arteries are injured and are not sealed completely, blood escapes and dissects the adjacent tissue. Finally, it results in collection of the blood in the perivascular areas. If this collection keeps communicating with the parent vessel, a pseudoaneurysm can be formed and the rupture of it can cause profuse bleeding [3].
We assume that the pseudoaneurysm might develop as a result of incomplete vessel occlusion in the process of repeated deep suturing of bleeding site in the cervix during conization. Trauma to uterine artery during conization and suturing may resulted in formation of hematoma around the adjacent tissues. Continuous blood flow from artery to this hematoma may forms pseudoaneurysm [4].
The formation of pseudoaneurysm is usually found after cesarean section, curettage, or vaginal delivery, but it is very rare for cervical conization. Therefore, it is so hard to come up with the possibility of pseudoaneurysm when we meet a patient with vaginal bleeding after conization.
While true aneurysm has a three layered arterial wall, pseudoaneurysm doesn't have it. In this case report, the bleeding was not life-threatening, however delaying of accurate diagnosis can make clinical course more difficult. Given the fact that the ruptured pseudoaneurysm can be life threatening, we need to consider the possibility of vascular injury like pseudoaneurysm when we find a patient with vaginal bleeding after the procedure [5].
Doppler ultrasonography and CT angiography are very useful techniques to diagnose this condition. On the color Doppler examination, aneurismal sac is imaged with a cystic area filled with a turbulent, multidirectional, mosaic type of blood flow pattern. Gray-scale imaging reveals an echogenic capsule around it. A feeding artery is imaged with a high peak systolic velocity. CT angiography is very helpful for demonstrating the location of the pseudoaneurysm and identifying feeding vessels through three-dimensional reformatted images [2].
Selective embolization of an affected vessel can be done to control bleeding. Emergency arterial embolization is a well established therapeutic option for controlling ruptured pseudoaneurysm [5].
Yeniel et al. [6] reported UAP after cesarean section. They diagnosed UAP through Doppler ultrasonography but they didn't perform emergency arterial embolization, eventually in the day after diagnosis they could not help performing laparotomy due excessive vaginal bleeding. To the best of our knowledge, this is the first case report on the cause-and-effect relation between pseudoaneurysm and conization in South Korea. Kwon [7] has reported 21 cases of acquired uterine arteriovenous malformations including eight cases of pseudoaneurysm. His previous report, however, only stated that pseudoaneurysm was occured after curettage or cesarean section and did not after conization. Acquired uterine arteriovenous malformations are characterized by multiple communications of varying sized between arteries and veins in the same vicinity, whereas pseudoaneurysms result from inadequate sealing of a laceration or puncture of the arterial wall during surgery or penetrating trauma [8]. Similar cases were reported in France by Zanati et al. [9] in the year 2006 and in the US by Jain et al. [10] in 2014 respectively. Both reports have stated that UAP was occurred due to cold-knife conization, and they used angiography to demonstrate the vascular injury and cure the condition through embolization. The success rate of embolization is 97%. Also, there are several advantages of uterine arterial embolization compare to surgical management such as hysterectomy. First, the embolization makes it possible to avoid general anesthesia. Second, we may spare the fertility of a patient. Finally, we can also identify the exact bleeding site [3].
Arterial embolization is an effective and safe procedure, but the effectiveness has never been evaluated in a large cohort of patient with pseudoaneurysm. It would probably because of the rarity of this condition [11].
As mentioned earlier, the formation of UAP after cervical conization is so rare that it is easy to overlook the chance of it. In this case report it is concluded that UAP should be considered in the differential diagnosis in a woman with unusual vaginal bleeding after cervical conization. For this reason, we emphasize the necessity of performing radiologic examination such as CT angiography or Doppler ultrasonography for the patient with vaginal bleeding and unexplained hemoperitoneum after cervical conization.
Figures and Tables
References
1. Kurata H, Aoki Y, Tanaka K. Delayed, massive bleeding as an unusual complication of laser conization: a case report. J Reprod Med. 2003; 48:659–660.
2. Marnela K, Saarelainen S, Palomaki O, Kirkinen P. Sonographic diagnosis of postpartum pseudoaneurysms of the uterine artery: a report of 2 cases. J Clin Ultrasound. 2010; 38:205–208.
3. Chitra TV, Panicker S. Pseudoaneurysm of uterine artery: a rare cause of secondary postpartum hemorrhage. J Obstet Gynaecol India. 2011; 61:641–644.
4. Sharma AM, Burbridge BE. Uterine artery pseudoaneurysm in the setting of delayed postpartum hemorrhage: successful treatment with emergency arterial embolization. Case Rep Radiol. 2011; 2011:373482.
5. Dohan A, Soyer P, Subhani A, Hequet D, Fargeaudou Y, Morel O, et al. Postpartum hemorrhage resulting from pelvic pseudoaneurysm: a retrospective analysis of 588 consecutive cases treated by arterial embolization. Cardiovasc Intervent Radiol. 2013; 36:1247–1255.
6. Yeniel AO, Ergenoglu AM, Akdemir A, Eminov E, Akercan F, Karadadas N. Massive secondary postpartum hemorrhage with uterine artery pseudoaneurysm after cesarean section. Case Rep Obstet Gynecol. 2013; 2013:285846.
7. Kwon JH. Radiologic diagnosis and treatment of iatrogenic acquired uterine arteriovenous malformation. J Korean Radiol Soc. 2002; 46:483–490.
8. Kwon JH, Kim GS. Obstetric iatrogenic arterial injuries of the uterus: diagnosis with US and treatment with transcatheter arterial embolization. Radiographics. 2002; 22:35–46.
9. Zanati J, Sergent F, Clavier E, Marpeau L. Late post-conization hemorrhage and false aneurysm of the uterine pedicle. J Gynecol Obstet Biol Reprod (Paris). 2006; 35:725–728.
10. Jain J, O'Leary S, Sarosi M. Uterine artery pseudoaneurysm after uterine cervical conization. Obstet Gynecol. 2014; 123:2 Pt 2 Suppl 2. 456–458.
11. Dohan A, Soyer P, Subhani A, Hequet D, Fargeaudou Y, Morel O, et al. Postpartum hemorrhage resulting from pelvic pseudoaneurysm: a retrospective analysis of 588 consecutive cases treated by arterial embolization. Cardiovasc Intervent Radiol. 2013; 36:1247–1255.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download