Abstract
Objective
To compare real-life clinical outcomes with the levonorgestrel-releasing intrauterine system (LNG-IUS) and conventional medical therapies (CMTs), including combined oral contraceptives and oral progestins in the treatment of idiopathic heavy menstrual bleeding (HMB) in South Korea.
Methods
This prospective, observational cohort study recruited a total of 647 women aged 18 to 45 years, diagnosed with HMB from 8 countries in Asia, including 209 women from South Korea (LNG-IUS, 169; CMTs, 40), who were followed up to one year. The primary outcome was cumulative continuation rate (still treated with LNG-IUS and CMTs) at 12 months. Secondary outcomes included bleeding pattern, assessment of the treatment efficacy by treating physician and safety profile.
Results
The continuation rate at 12 months was significantly higher with the LNG-IUS than CMTs (85.1% vs. 48.5%, respectively; P<0.0001). The 51.5% of CMTs patients discontinued treatment and 18.8% of LNG-IUS patients discontinued treatment. The most common reasons for discontinuation for CMTs were switching to another treatment and personal reasons. When compared to CMTs, the LNG-IUS offered better reduction in subjectively assessed menstrual blood loss and the number of bleeding days, tolerability and with better efficacy in HMB, as assessed by physician's final evaluation.
Conclusion
This study provides novel information on the real-life treatment patterns of HMB in South Korea. The efficacy of CMTs was inferior compared to the LNG-IUS in the clinical outcomes measured in this study. Due to the better compliance with LNG-IUS, the cumulative continuation rate is higher than CMTs. We conclude that the LNG-IUS should be used as the first-line treatment for HMB in Korean women, in line with international guidelines.
Approximately 30% of women experience heavy menstrual bleeding (HMB) or menorrhagia at some point in their reproductive life, which is defined as excessive menstrual blood loss. It may occur alone or in combination with other symptoms, with a negative impact on a woman's physical, social, emotional and/or material quality of life [1,2,3,4]. Approximately one in 20 women in the age group of 30 to 49 years consult their primary care physician each year for HMB, which is the second most common reason for a hospital referral, and accounts for 12% of all gynecological referrals [5,6]. However, despite this significant disease burden, documented evidence on the actual clinical practice of HMB care is sparse in the Asia-Pacific region.
Data from the Caucasian population indicate that levonorgestrel-releasing intrauterine system (LNG-IUS; Mirena, Bayer HealthCare, Wayne, NY, USA) is a safe and effective treatment for HMB [7]. Similarly, small single-site studies conducted in Hong Kong [8] and Beijing [9] have demonstrated that LNG-IUS may be an effective and acceptable treatment for idiopathic HMB in perimenopausal Chinese women. In addition, recent data indicate higher effectiveness of the LNG-IUS vs. combined oral contraceptives (COCs) [10] and oral medroxy-progesterone acetate [11]. Data in Caucasian women also suggest high acceptance and tolerability in everyday clinical practice [12], although less favorable reports depending on practice settings have also been reported [13]. However, there is limited data available from Korea on the treatment practices for women affected by HMB.
Although COCs and oral progestogens, named conventional medical treatments (CMTs) in this study, are frequently used as first-line therapies for HMB, data is limited on their long-term acceptability and tolerability. Available data from the Caucasian population suggest poor long-term compliance with CMTs [14,15].
While sufficient data is available from the Caucasian studies on the everyday clinical use of treatment patterns with the LNG-IUS [16,17] or CMTs, there is limited insights available from Asian countries such as South Korea. The previously reported MiCo (Mirena or Conventional Medical Treatment for Menorrhagia) study [18] was initiated to address these knowledge gaps, and to verify whether the LNG-IUS improves clinical outcomes compared to CMTs in Asian patients, similar to the data shown in European and North American clinical studies. This publication now reports a sub-analysis of this large Asia-Pacific non-interventional study, with focus on the patient group from South Korea. The proportion of Korean patients was one third of the entire study population, representing the largest group in the study. In view of the limited data available on this subject, the outcome of this subgroup analysis can be discussed in relation to the overall result and studies conducted in other regions to confirm comparable results. Furthermore, it will reflect the unique clinical features of population. Considering that LNG-IUS is currently well established in medical treatment practice in Korea, this study allows a better understanding of its application.
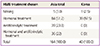
This global non-interventional study is a prospected, cohort study which enrolled women aged 18 to 45 years with complaints of idiopathic HMB over several cycles with no intention to conceive within one year from the start of therapy. A total of eight countries participated from Asia, including China, Taiwan, Hong Kong, Indonesia, Malaysia, Pakistan, South Korea, and Thailand. The Korean arm of the study recruited 209 patients from 19 sites (32.3% of the total study population) within South Korea during September 2008 to December 2010. The study protocol was approved by the local independent ethics committee or institutional review board when required. All participants provided written, informed consent before study enrolment. The study was conducted in accordance with the amended version of the Declaration of Helsinki and in compliance with the principles of Good Clinical Practice. The study was registered at ClinicalTrials.gov (NCT00864136, March 9, 2010). The inclusion and exclusion criteria are described in Table 1. Participating physicians were asked to complete a questionnaire to understand their preferred lines of therapy and average time spent on counseling a patient about HMB. Physicians participating in the study treated patients with LNG-IUS and CMTs in routine practice. The study enrolment did not warrant additional investigations and the choice of treatment was determined by the treating physician, who prescribed LNG-IUS or CMTs according to their clinical judgment, independent of enrolment into the study. The physicians had to document at least one and maximum three follow-up visits during a one-year timeframe and standardized case report forms were used for documentation, which formed the basis for all analysis. At baseline, demographic data, gynecologic and obstetrical history, and data on the duration of idiopathic HMB and previous treatments, if any, were documented. In addition, subjective evaluation of the amount of bleeding (5-degree Likert like scale, none to very heavy), the number of bleeding/spotting days during the last 30 days as informed by the questions, and subjective evaluation of menstrual pain and premenstrual symptoms (PMS) (4-degree Likert like scale, none to severe) were collected. Documentation of each item was mandatory at each follow-up visit, along with documentation of concomitant medications, change of therapy and adverse events. At the last visit (at 12 months or at premature discontinuation), the subjective satisfaction (by patient) as well as final assessment of the efficacy and the tolerability of the treatment (by physician) was collected.
The primary outcome measure of this study was the cumulative continuation rate at 12 months stratified by the history of previous treatment(s) for HMB. Observations up to 402 days (365 days+6 weeks) were considered to represent this continuation rate. In addition, secondary outcome parameters such as bleeding pattern, patient satisfaction at end of documentation, impact of the therapy in terms of patient-derived health outcomes (based on the Menorrhagia Multi-Attribute Scale [19] and to be reported elsewhere) and safety profile were included as part of the study. These variables were analyzed at one year after start of the therapy or at the end of therapy (if earlier). The analyses were primarily of an explorative and descriptive nature, performed using summary statistics for categorical and quantitative (continuous) data. Fisher's exact test was used for the calculation of cumulative continuation rate, and analyzed with Kaplan-Maier plot. Adverse events were summarized using the MedDRA (Medical Dictionary for Regulatory Activities) coding system version 14.0 by system organ classes and preferred terms.
A total of 18 physicians from South Korea completed the physician questionnaire. Most physicians spent 6 to 10 minutes per patient discussing HMB, which was in line with overall data from the Asia-Pacific region (data discussed elsewhere). The most common first-line treatments for idiopathic HMB were COCs and NSAIDs, and LNG-IUS and COCs were the most preferred second-line option, while GnRH analogs and oral progestogens were the preferred third-line options (Fig. 1). Out of a total of 647 women from the 8 participating Asian countries, a total of 209 patients (32.3%) (LNG-IUS, 169; CMTs, 40) were recruited from South Korea. All patients were included for the safety analysis (full analysis set), while the per-protocol sample of 187 patients (LNG-IUS, 154; CMTs, 33) were included for efficacy analysis.
Demographic and baseline bleeding characteristics of the study population are presented in Table 2. The majority of the patients (approximately two-thirds) belonged to the age group of 36 to 45 years. The baseline characteristics of patients in both the treatment arms were comparable. Out of the 209 participants, 121 women (57.9%) had a history of gynecological disorder or procedure, most commonly Caesarian section, uterine fibroids, and cervical dilatation and curettage. Majority of the patients (LNG-IUS, 88.2%; CMTs, 65.0%) did not have a previous menorrhagia treatment. The most frequent previous therapies were surgery and COCs.
The efficacy population (per-protocol pample cohort, n=187) was evaluated for cumulative treatment continuation rate within a timeframe of 402 days (1 year+6 weeks). The cumulative treatment continuation rate in the LNG-IUS arm was significantly higher than in the CMT arm (85.1% vs. 48.5%, respectively; P<0.0001). In the LNG-IUS group, previous treatment experience had no significant impact on the continuation rate (continuation rate with vs. without previous treatment experience: 87.5% vs. 84.4%, respectively). In the CMT group, however, the treatment continuation rate was lower with previous treatment experience (40.0%), as compared to treatment naïve patients (52.2%). The odds ratio for discontinuation in the CMT vs. the LNG-IUS groups was 6.05 (95% confidence interval, 2.68 to 13.66). The duration until discontinuation was compared via a Kaplan-Meier analysis. In this evaluation, for patients without documented end of therapy, the duration of observation was computed and interpreted as censored duration until discontinuation. The Kaplan-Meier plot of the two treatment groups is shown in Fig. 2. Fig. 2 shows that the proportion of patients without discontinuation of therapy decreased very slowly in the LNG-IUS group, compared to the CMT group. While the proportions for the CMT group decreased below 50% within the observation period, more than 80% of the LNH-IUS group still continued their treatment. Stratification of continuation rate by age, body mass index or duration of HMB symptoms did not have a marked impact on these overall results (data not shown).
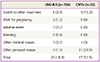
Among the 18.8% patients who discontinued treatment in the LNG-IUS group, most common reason for discontinuation was bleeding, while among the 51.5% of patients who discontinued the treatment in the CMT group, the most common reason for discontinuation was switch to other treatment except other personal reason (Table 3).
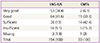
The number of bleeding and spotting days during the observation period is shown in Fig. 3. Overall, a larger decrease of bleeding days was observed from the initial visit to the last follow up within the LNG-IUS group (mean±SD, 1.6±3.4 days) as compared to the CMT group (mean±SD, 3.2±1.5 days) (Fig. 3A). The mean reduction in spotting days of LNG-IUS and CMT group was 1.8 day and 0.6 days, respectively, and there was an increase of 2.3 days in the mean number of spotting days in the LNG-IUS group compared to baseline spotting days (mean±SD, 3.5±3.6) (Fig. 3B). The subjective evaluation of the amount of bleeding showed a higher percentage of patients reporting "no" or "slight" bleeding in the LNG-IUS group, compared to the CMT group where the patients reported higher proportion of "slight" or "moderate" bleeding (Fig. 4)-this difference was observed already starting from the first follow up and increased over time. In addition, the LNG-IUS also offered better control of other associated symptoms, with higher proportion of women on LNG-IUS experiencing complete remission of menstrual pain (last documented visit; LNG-IUS, 104/154, 67.5%; CMTs, 15/30, 50.0%). Also, the proportion of patients on LNG-IUS who reported complete resolution of PMS, were comparable to the CMTs group (last documented visit; LNG-IUS, 103/154, 66.9%; CMTs, 23/30, 76.7%). The physicians' evaluation (Table 4) indicated better efficacy and tolerability with LNG-IUS as compared to CMTs in the management of HMB, which was concordant with the patient-reported outcomes. In this study, the following points showed differences in clinical practice when comparing the Korean patients with the overall results. In the question about previous HMB treatment, the number of "no treatment received" in the entire group was 355 (54.9%) compared to 175 (83.7%) in the South Korean group. This would mean that physician's active intervention, at least from these figures, for the treatment of HMB is less in Korea than in the overall population of this study. Regarding the type of treatment chosen in the conventional therapy group, use of antifibrinolytics only or combined hormone and antifibrinolytic treatment group in total study group was 39 (23.8%) and 36 (22%), respectively. In comparison, in the South Korean group, antifibrinolytics were not chosen, and hormonal therapy was favored in 97.5% of cases (Table 5).
The nature and frequency of adverse events and treatmentrelated adverse events occurring during therapy were consistent with the established safety profile of the treatments administered. Overall, adverse events were reported in 17.1% (29/169) patients in the LNG-IUS group and 12.5% (5/40) in the CMTs group, of which 14.2% (24/169) in the LNG-IUS group and 10% (4/40) in the CMT group were treatment-related. In the LNG-IUS group, the most common adverse events were reproductive system and breast disorders (n=17, 10.1%), including HMB (n=7) and uterine hemorrhage (n=7). No serious adverse events leading to prolonged bleeding or requiring hospitalization were reported in the LNG-IUS or CMTs group.
Even though various treatment modalities have been introduced for the management of HMB in South Korea, there is limited data on the real-life clinical practice and treatment choices. This study reports real-world treatment preferences of HMB treatments in South Korea, providing insights to the current practices and clinical decision making processes, which to the best knowledge of the authors is a first of its kind.
This prospective non-interventional cohort study compares LNG-IUS and CMTs, which are the two most commonly used medical treatment modalities for idiopathic HMB. The term 'CMTs' encompasses hormonal treatments such as COCs and oral or injectable progestogens. Previous history of HMB treatments is also taken into account, as the continuation rate was also analyzed stratified by exposure to previous treatments. The observational setting used in this study provides us a reallife model, with routine clinical criteria used in the diagnosis of HMB, and treatment allocation made on the discretion of the investigator as in normal clinical practice. This is probably one of the major strengths of this study. In contrast, the routine interventional clinical studies of HMB, with rigorous methodology for menstrual blood loss measurement (quantify blood loss measurement method: alkaline hematin method, the pictorial blood assessment chart method) and strict inclusion/exclusion criteria, have high screening failure rates, and may miss out the routine clinical spectrum of HMB patients [11]. Therefore, these latter studies represent results from a highly selected patient population, which may not be applicable to HMB patients seen in everyday clinical practice.
This study is an observational cohort study, which can be considered as one of the major limitations of this study. Due to the observational nature, both cohorts in the treatment arms are not necessarily identical. However, in this study the baseline characteristics of both the cohorts were comparable. The diagnosis of HMB was made based on patients' subjective complaints, as per the existing international guidelines on HMB [1]. This study does not employ objective measurements such as alkaline hematin method for quantification of menstrual blood loss, due to the observational nature of study methodology. However, such methods only have theoretical importance, as they are not practical to apply in routine clinical use, and hence should not form the basis of clinical diagnosis.
One of the glaring findings from this study, both from the Korean as well as the overall Asian population, is that the clinicians allocate only a limited time slot in counseling patients on HMB. This is one of the aspects of HMB care that needs special attention in our region. The study results also indicate that despite availability of global data on efficacy of LNG-IUS in HMB, CMTs are still considered as first-line therapies for HMB in Korea, while the LNG-IUS is considered mostly as a 2nd line treatment option. Higher patient load and shorter time allocated per patient in Korea may be one the reasons behind this preference of CMTs over LNG-IUS, as there may be a perception among the clinicians that CMTs may take shorter time to initiate vs. LNG-IUS, which requires pre-insertion counseling and fitting. In this study, even though antifibrinolytics are proven as conventional treatment for HMB treatment through the literature and guidelines, in almost all Korean cases physicians chose the use of hormonal treatment for HMB for their patients, in this study. The present study results demonstrated a clear superiority of the LNG-IUS compared to the CMTs in the treatment of HMB for the outcomes measured, including continuation rate, treatment efficacy, and reduction in the number of bleeding days, dysmenorrhea and PMS related symptoms. The difference between the treatments in the continuation rate at 12 months was more than 30%, which can be considered as robust evidence of clear clinical benefit of the LNG-IUS over CMTs in the treatment of HMB. The continuation rate was higher with the LNG-IUS, regardless of the CMT treatment type.
The present study results are in line with previous randomized clinical studies, comparing the LNG-IUS to oral progestins and combined oral contraceptives [7]. Thus the results can be considered to confirmatory of the previous studies using more rigorous methodologies.
The continuation rates in the LNG-IUS group were similar regardless of exposure to previous HMB treatment, whereas in the CMT group, continuation rate was clearly lower among patients who had already tried at least one treatment for HMB. This is an interesting novel finding, as continuation rates or other clinical outcomes have usually not been reported separately for naïve and non- naïve patients in most HMB trials.
Treatment discontinuations in the CMT group were mostly related to switch to other treatment or personal reasons. The former can be considered as a sign of insufficient treatment efficacy, while it was not possible to collect detailed information on the personal reasons indicated as reason for discontinuation. The occurrence of adverse events was low, and serious adverse events occurred at a frequency of <1%. While the adverse event rate in the LNG-IUS group was higher than in the CMT group, a comparison of the crude incidences of adverse events between the treatment groups is hindered by the disparate observation and exposure time in the two groups, with a longer, continuous exposure and observation time in the LNG-IUS group compared to conventional treatment for the women included in the safety analysis.
This study provides us with insights into the management of HMB in Asia in real-life situations. It concurs with the data which has been the basis of international HMB treatment guidelines, placing the LNG-IUS as the first-line treatment for HMB [1,20]. The data from this study could also help in understanding the typical characteristics of Asian HMB patient population, showing that they benefit equally from the treatment with the LNG-IUS, as compared to previously published studies in Caucasians [7]. In view of these conclusive data, LNG-IUS should be considered as the first-line treatment for the management of HMB in Korean women, in line with existing international guidelines.
Figures and Tables
Fig. 1
Current treatment preferences in the management of HMB (multiple responses allowed). Physicians (n=18) were asked to select 1st, 2nd, and 3rd line treatments for HMB according to their current prescription preference. Multiple choices were allowed for each category. The graph shows the treatment options by percentage of physicians choosing them. HMB, heavy menstrual bleeding; COCs, combined oral contraceptives; NSAIDs, non-steroidal anti-inflammatory drugs; LNG-IUS, levonorgestrel-releasing intrauterine system; GnRH, gonadotropin-releasing hormone.

Fig. 2
Kaplan-Maier plot of time to discontinuation of treatment stratified by treatment group: levonorgestrel-releasing intrauterine system vs. conventional medical treatment.
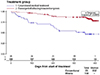
Fig. 3
Number of bleeding days (A) and spotting days (B) during last 30 days according to treatment group. LNG-IUS, levonorgestrel-releasing intrauterine system; CMT, conventional medical treatment.

Fig. 4
Subjective evaluation of the amount of bleeding by treatment group. (A) Levonorgestrel-releasing intrauterine system and (B) conventional medical treatment.

Acknowledgments
This study was funded by Bayer Healthcare Pharmaceuticals. This study would not have been possible without the support of co-investigators. The authors like to gratefully acknowledge the enthusiastic efforts of Min Hyung Jung (Kyunghee University Medical Center, Seoul, Korea), Hee Dong Chae (Ulsan University, Asan Medical Center, Seoul, Korea), Byong Ick Lee (Inha University Hospital, Incheon, Korea), Seok Ju Seoung (CHA University, CHA Gangnam Medical Center, Seoul, Korea), Joon Cheol Park (Kyemyung University, Dongsan Medical Center, Daegu, Korea), Dr. Tai June Kim (Mizmedi Hospital, Seoul, Korea), Dr. KyungA Kim (Presbyterian Medical Center, JeonJu, Korea), Dr. MeeHyea Yang (Yangmeehyea OBGY Clinic, Seoul, Korea), Dr. Sung-Phil Bang (Miraero Women's Hospital, Pusan, Korea), Dr. HoJin Cheong (Baylorewha OB&GY Clinic, Seongnam, Korea), Dr. Jung Ah Kwag (KwagJungah OB&GY Clinic, Yongin, Korea) and Dr. SangHyun Kim (Dongwong OB&GY Clinic, Ilsan, Korea) for this study. Four of the authors are employees of Bayer Healthcare Pharmaceuticals. UBM Medica Asia Pte. Ltd. provided writing and editorial support which was funded by Bayer Healthcare Pharmaceuticals.
Notes
BSL, XL, and SA have no conflicts of interest. PK and PI are employees of Bayer HealthCare Pharmaceuticals. JEL is an employee of Bayer HealthCare Korea. The study was sponsored by Bayer HealthCare, which was also involved in protocol development. Data analysis was conducted by an external clinical research organization (Institute Dr Schauerte, Oberhaching, Germany).
References
1. National Institutes for Health and Care Excellence. Heavy menstrual bleeding: NICE guidelines CG44 [Internet]. London: National Institutes for Health and Care Excellence;c2012. cited 2012 Jan 4. Available from: http://www.nice.org.uk/nicemedia/pdf/CG44NICEGuideline.pdf.
2. Oehler MK, Rees MC. Menorrhagia: an update. Acta Obstet Gynecol Scand. 2003; 82:405–422.
3. El-Hemaidi I, Gharaibeh A, Shehata H. Menorrhagia and bleeding disorders. Curr Opin Obstet Gynecol. 2007; 19:513–520.
4. Lopes JE Jr, Sherer E. Managing menorrhagia: evaluating and treating heavy menstrual bleeding. Adv NPs PAs. 2010; 1:21–24.
5. Royal College of Obstetricians and Gynaecologists. The initial management of menorrhagia: evidence-based clinical guidelines no.1 [Internet]. London: Royal College of Obstetricians and Gynaecologists;c1998. cited 2012 Jan 20. Available from: http://www.rcog.org.uk.
6. Duckitt K, McCully K. Menorrhagia. Clin Evid. 2003; (10):2151–2169.
7. Kaunitz AM, Inki P. The levonorgestrel-releasing intrauterine system in heavy menstrual bleeding: a benefitrisk review. Drugs. 2012; 72:193–215.
8. Tang GW, Lo SS. Levonorgestrel intrauterine device in the treatment of menorrhagia in Chinese women: efficacy versus acceptability. Contraception. 1995; 51:231–235.
9. Xiao B, Wu SC, Chong J, Zeng T, Han LH, Luukkainen T. Therapeutic effects of the levonorgestrel-releasing intrauterine system in the treatment of idiopathic menorrhagia. Fertil Steril. 2003; 79:963–969.
10. Shaaban MM, Zakherah MS, El-Nashar SA, Sayed GH. Levonorgestrel-releasing intrauterine system compared to low dose combined oral contraceptive pills for idiopathic menorrhagia: a randomized clinical trial. Contraception. 2011; 83:48–54.
11. Kaunitz AM, Bissonnette F, Monteiro I, Lukkari-Lax E, Muysers C, Jensen JT. Levonorgestrel-releasing intrauterine system or medroxyprogesterone for heavy menstrual bleeding: a randomized controlled trial. Obstet Gynecol. 2010; 116:625–632.
12. Robinson R, China S, Bunkheila A, Powell M. Mirena intrauterine system in the treatment of menstrual disorders: a survey of UK patients' experience, acceptability and satisfaction. J Obstet Gynaecol. 2008; 28:728–731.
13. Ewies AA. Levonorgestrel-releasing intrauterine system: the discontinuing story. Gynecol Endocrinol. 2009; 25:668–673.
14. Cooper KG, Jack SA, Parkin DE, Grant AM. Five-year follow up of women randomised to medical management or transcervical resection of the endometrium for heavy menstrual loss: clinical and quality of life outcomes. BJOG. 2001; 108:1222–1228.
15. Coulter A, Bradlow J, Agass M, Martin-Bates C, Tulloch A. Outcomes of referrals to gynaecology outpatient clinics for menstrual problems: an audit of general practice records. Br J Obstet Gynaecol. 1991; 98:789–796.
16. Tariq N, Ayub R, Jaffery T, Rahim F, Naseem F, Kamal M. Efficacy of levonorgestrel intrauterine system (LNG-IUS) for abnormal uterine bleeding and contraception. J Coll Physicians Surg Pak. 2011; 21:210–213.
17. Yoo HJ, Lee MA, Ko YB, Yang JB, Kang BH, Lee KH. The efficacy of the levonorgestrel-releasing intrauterine system in perimenopausal women with menorrhagia or dysmenorrhea. Arch Gynecol Obstet. 2012; 285:161–166.
18. Lee BS, Ling X, Asif S, Kraemer P, Hanisch JU, Inki P. Levonorgestrel-releasing intrauterine system versus conventional medical therapy for heavy menstrual bleeding in the Asia-Pacific region. Int J Gynaecol Obstet. 2013; 121:24–30.
19. Shaw RW, Brickley MR, Evans L, Edwards MJ. Perceptions of women on the impact of menorrhagia on their health using multi-attribute utility assessment. Br J Obstet Gynaecol. 1998; 105:1155–1159.
20. Marret H, Fauconnier A, Chabbert-Buffet N, Cravello L, Golfier F, Gondry J, et al. Clinical practice guidelines on menorrhagia: management of abnormal uterine bleeding before menopause. Eur J Obstet Gynecol Reprod Biol. 2010; 152:133–137.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download