Abstract
Splenosis is defined as heterotopic autotransplantation of spleen tissue following traumatic rupture of the spleen, or surgery. It is a benign disease that is generally without any symptoms and is discovered incidentally. Surgical intervention is recommended if symptoms are present. We report the successful laparoscopic management of a 49-year-old Korean woman with splenosis-associated symptoms who had undergone splenectomy.
Splenosis is defined as heterotopic autotransplantation of spleen tissue following traumatic rupture of the spleen, or surgery. It is an acquired condition that may occur anywhere in the abdominal cavity and occasionally in brain tissue, subcutaneous tissue, or intrathoracic tissue [1,2].
In 1995, Higgins and Crain [3] reported the first successful laparoscopic procedure for pelvic splenosis. Since then, laparoscopic removal of splenic tissue has become the treatment of choice for patients with surgery-requiring splenosis [3-5]. We report the successful laparoscopic management of splenosis in a 49-year-old Korean woman who had undergone splenectomy after traumatic splenic rupture.
A 49-year-old Korean menopausal woman was referred to our hospital for lower abdominal pain and incidentally detected ovarian mass. She had undergone a laparotomy because of a traffic accident 25 years previously, and at that time a splenectomy had been performed to remove a ruptured spleen.
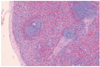
On physical examination, the patient had left lower abdominal tenderness without specific signs of peritoneal irritation or pelvic symptoms. A gynecological ultrasonogram showed a normal uterus and right ovary in terms of size and shape. However, a 45 × 30 mm homogeneous cystic mass adhered to the left ovary without ascites. Hematological values and serum levels of CA-125 and CA-19-9 were within the normal ranges. Abdominal pelvic computerized tomography, pelvic magnetic resonance imaging and chest computerized tomography scans revealed a 50 mm cystic mass in the left pelvic cavity and several small pleural nodules in the left lower lobe of the lung. We performed laparoscopic surgery to confirm the final diagnosis and relieve the patient's persistent abdominal pain. Adhesions of the greater omentum and the anterior wall of the abdominal cavity were found along the ligamentum teres. Adhesiolysis was performed using a harmonic scalpel (Ultracision Harmonic Scalpel, Ethicon Endo Surgery, Cincinnati, OH, USA). The lesions varied in size, were a purplish color, and were lobulated and hypervascularized along the mesocolon of the bowel from the sigmoid colon to the rectum (Fig. 1A). The splenic nodules were entirely removed after dissecting them from the bowel. Rectum tearing was observed in the serosal layer, and primary closure was performed using 3-0 polyglactin 910 sutures (Vicryl, Ethicon Inc., Somerville, NJ, USA). In the pelvic cavity, 50×30 mm splenic nodules were seen on the upper side of the left uterosacral ligament, ureter, and lower lateral side of the left ovary (Fig. 1B). The left pelvic wall peritoneum was carefully dissected and the splenic nodules were removed after locating the ureter in the retroperitoneal area. The largest mass adhered to the mesocolon, and was sent for frozen section examination and confirmation as normal splenic tissue (Fig. 2). The nodules were placed in an endo-bag (Lap-bag, Sejong Medical, Paju, Korea) and retrieved via a 12 mm trocar. The patient recovered without any complications and was discharged on the eighth postoperative day. The patient is currently being followed up without any other complications or specific symptoms.
Splenosis is the autotransplantation of splenic tissue with normal splenic function. It is a benign disease that is different from having an accessory spleen. Accessory spleens are congenital and arise from the dorsal mesogastrium during the embryonic period [6]. They have normal splenic histology with blood supply from the splenic artery, and are located near the splenopancreatic or gastrosplenic ligament. On the other hand, splenosis tissues have a distorted architecture with no hilum, poorly formed capsules, and tissues of variable shape and size [2,6]. The blood supply is derived from the surrounding tissue and vessels, not from the splenic artery. There are multiple splenic implants [7]. And the most common causes of splenosis are trauma and hematological disease [2,4].
Splenosis can occur anywhere in the abdominal cavity. It is occasionally found in the intrathoracic and pancreatic regions, inguinal ring, nephrectomy sites, port sites of previous surgery, or in the brain [2,7]. It has been reported to occur in 16% to 17% of patients who undergo elective splenectomy because of hematological disease, and was found in 44% to 76% of patients undergoing post-traumatic splenectomy due to spillage of splenic tissue after splenic rupture caused by trauma [2,8]. A high incidence of residual splenic tissue has been reported in routine postoperative scintigraphy after laparoscopic splenectomy [9].
Because splenosis is usually asymptomatic, it is most commonly discovered incidentally, during surgery or evaluation for another disease. It does not require any additional treatment if the patient does not present with symptoms. Patients often present with non-specific abdominal pain due to infarction, an enlarging abdominal mass, intestinal obstruction due to adhesive bands of implants, gastrointestinal hemorrhage, hydronephrosis, or pressure on adjacent organs [10]. If splenosis occurs in the pelvic cavity, symptoms such as pelvic pain, dysmenorrhea, dyspareunia or other gynecologic symptoms may occur [2,11]. It is difficult to diagnose splenosis since it can occur at various sites and has non-specific symptoms.
Nuclear scintigraphy is the preferred method for the non-interventional diagnosis of splenosis. The intravenous use of scintigraphic agents such as Tc-99m sulfur colloid and Tc-99m heat-damaged erythrocytes has high diagnostic sensitivity [10]. If the splenosis causes symptoms, surgical management is the treatment of choice [3,5,12]. Previously, identification and removal of ectopic spleen tissue by surgery was the preferred treatment of choice. However, since laparoscopic surgery now allows visualization of the retrogastric pouch, which is not visible through open surgery, laparoscopic surgery is now preferred.
The most important goal of laparoscopic surgery is the complete identification and removal of splenic nodules. It is important to remove all of the nodules at once to prevent dissemination. Spillage should be prevented by using an endo-bag.
A successful diagnosis was made and treatment was performed on a patient with a history of splenectomy who presented with abdominal symptoms. Splenosis should be suspected in patients with a history of splenectomy. Minimally invasive surgery such as laparoscopy is the ideal treatment for patients with symptomatic splenosis.
Figures and Tables
References
1. Khosravi MR, Margulies DR, Alsabeh R, Nissen N, Phillips EH, Morgenstern L. Consider the diagnosis of splenosis for soft tissue masses long after any splenic injury. Am Surg. 2004; 70:967–970.
2. Vydianath B, Gurumurthy M, Crocker J. Solitary ovarian splenosis. J Clin Pathol. 2005; 58:1224–1225.
3. Higgins RV, Crain JL. Laparoscopic removal of pelvic splenosis: a case report. J Reprod Med. 1995; 40:140–142.
4. Sato M, Motohiro T, Seto S, Kogire M, Takada K, Hamada Y. A case of splenosis after laparoscopic splenectomy. Pediatr Surg Int. 2007; 23:1019–1021.
5. Barbaros U, Dinccag A, Kabul E. Minimally invasive surgery in the treatment of splenosis. Surg Laparosc Endosc Percutan Tech. 2006; 16:187–189.
6. Fremont RD, Rice TW. Splenosis: a review. South Med J. 2007; 100:589–593.
7. Kumar RJ, Borzi PA. Splenosis in a port site after laparoscopic splenectomy. Surg Endosc. 2001; 15:413–414.
8. Wold PB, Farrell MA. Pleural nodularity in a patient with pyrexia of unknown origin. Chest. 2002; 122:718–720.
9. Gigot JF, Jamar F, Ferrant A, van Beers BE, Lengele B, Pauwels S, et al. Inadequate detection of accessory spleens and splenosis with laparoscopic splenectomy: a shortcoming of the laparoscopic approach in hematologic diseases. Surg Endosc. 1998; 12:101–106.
10. Tsitouridis I, Michaelides M, Sotiriadis C, Arvaniti M. CT and MRI of intraperitoneal splenosis. Diagn Interv Radiol. 2010; 16:145–149.
11. Celiloglu M, Dogan E, Kocoglu S, Sarihan E. Splenosis presenting with adnexal mass: a case report. Arch Gynecol Obstet. 2004; 270:129–130.
12. Hashimoto K, Orita H, Koga T, Kawanaka H, Kono H, Maehara Y. Laparoscopic treatment of splenosis: report of a case. Surg Today. 2009; 39:1098–1102.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download