Abstract
When retroperitoneal leiomyosarcoma develops in pelvic cavity, it often presents similar symptoms and radiological findings to adnexal tumor, therefore obscures diagnostic approaches until an exploratory laparotomy is performed. We report an unusual presentation of retroperitoneal leiomyosarcoma mimicking an adnexal tumor with extremely elevated serum CA-19-9. Though the most of the prominent mass was removed during surgery, there was massive bleeding due to tearing of internal iliac vein while dissecting the ureter close to vessels. This case focuses on the significance of considering retroperitoneal tumor even if the mass is located in ovarian fossa and has highly elevated serum level of CA-19-9. And in attempt of tumor removal, the excision needs to be clean-cut without damaging nerves or vessels around the mass and avoid causing any prospective complications.
Leiomyosarcoma is a malignant tumor originated from smooth muscle and it constitutes 5% to 10% of all sarcoma originated from soft tissue [1]. It usually develops in uterus, gastrointestinal tract, retroperitoneum, and rarely in skeletal tissue. It is common that retroperitoneal leiomyosarcoma is detected as a massive abdominal mass due to lack of specific sign or symptoms while it grows [2]. Complete surgical removal is the most critical point in the treatment of retroperitoneal leiomyosarcoma. Despite poor response to postoperative therapy, it has been reported that postoperative radiation as well as chemotherapy elongates the overall survival [3,4]. We report an unusual presentation of retroperitoneal leiomyosarcoma mimicking an adnexal tumor with extremely elevated serum CA-19-9.
A 77-year-old woman was admitted with vague lower abdominal fullness and pain over six months. Tingling sensation on her right lower extremity has been developed since two months ago. Her menopause occurred at age of 45 years and she has never taken any hormone replacement therapy.
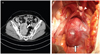
A hard, fixed, and non-tender mass as large as a man's fist was palpated in right lower abdomen on pelvic examination. Contrast-enhanced abdominal computerized tomography (CT) showed 9.4 × 6.3 × 5.1 cm sized lobulated mass in right pelvic cavity (Fig. 1A). It was seen relatively high enhanced and heterogenic mass on CT and causing hydronephroureterosis as a result of direct invasion of the ureter. The liver and renal function tests, and tumor markers such as CA-125, carcinoembryonic antigen, and alpha-fetoprotein were normal except the highly elevated level of CA-19-9 (70,000 U/mL).
Under the general anesthesia, surgical exploration was performed on suspicion of an ovary-origin tumor. The uterus and both adnexa showed normal appearance, however a 9 × 6 × 5 cm sized spherical mass with clear margin was found around right internal iliac artery in right retroperitoneal space (Fig. 1B). No enlargement of lymph nodes around the mass and metastasis were found. Intraoperative frozen section analysis suggested of a leiomyosarcoma. Radical surgical resection was done including total hysterectomy, both adnexectomy, and right pelvic lymph node sampling. Surgical excision was attempted in order to completely remove the tumor after dissecting mesenteric adhesion. However, the tumor was firmly adhered to the ureter as well as right internal iliac artery and the tissue of tumor crumbled very easily. Tearing of internal iliac vein that occurred during dissection the mass from the ureter and internal iliac vessels was repaired by vascular surgeon. Most of the prominent mass was removed and the operation was finished with inserting an internal ureteral stent in the right ureter to prevent leakage or stricture due to undiagnosed latent ureteral injury.
Pathologic examination revealed a high-grade leiomyosarcoma with spindle-shaped tumor cells arranged in fascicles with intermediate dysplasia and also rich mitotic cell division (Fig. 2A). On immunohistochemical staining, the sample showed positive results for vimentin, smooth muscle actin, and desmin; on the contrary, the sample was negative for CD31, CD34, and S-100 protein test (Fig. 2B). The tumor was surgically staged as stage IIB (T2b2 N0 M0) leiomyosarcoma.
The patient started late oral diet after 7 days of operation due to a mild paralytic ileus, and then exercised well and showed no symptoms or signs of postoperative complication until 20 days when she could discharge after the operation. We had scheduled postoperative radiation therapy considering the patient's general condition 4 weeks later after surgery. The radiation treatment with 3 dimensional conformal radiotherapy using a 10 MV photon beam (Varian, Palo Alto, CA, USA) was applied to the tumor bed and total dose of 5,040 cGy was administered with a fractionated daily dose of 180 cGy, five days a week. Serum CA-19-9 returned to normal level (25.85 U/mL) in the end of radiation therapy. She is currently alive 12 months after treatment without recurrence or metastasis.
Retroperitoneal sarcoma is a rare tumor accounting for 1% to 2% of all solid malignancies. In a population-based series reported in the Surveillance, Epidermiology, and End Results database, the average annual incidence of retroperitoneal sarcoma was approximately 2.7 cases per one million population [5]. Retroperitoneal leiomyosarcoma is a malignant cancer that develops in soft tissue of retroperitoneal cavity and it often grows without pain; such characteristic leads to incidental discovery and mostly as an enormous mass. It accounts for 21% to 60% of soft tissue sarcoma originated from retroperitoneum. Leiomyosarcoma can occur at any age, but mainly occurs in menopausal women at age of 50 to 70 years. Clinically, retroperitoneal leiomyosarcoma mostly presents no symptom, however if it is accompanied by any symptoms, they are usually obscure features such as abdominal pain, abdominal fullness, or neurological symptoms. With such trait, retroperitoneal leiomyosarcoma is often discovered as a massive tumor at the time of diagnosis. Lewis et al. [6] reported 70% of 500 patients diagnosed retroperitoneal leiomyosarcoma with tumors larger than 10 cm and the other 23% with 5 to 10 cm sized mass.
In order to diagnose, history taking, physical examination, chest and abdominal X-ray, abdominal ultrasonography, CT, and magnetic resonance imaging (MRI) may be used. Especially, CT is useful for visualizing location of tumor and association with surrounding organs as well as metastasis to liver or intraperitoneal cavity. MRI can be a supplementary tool to determine staging of cancer [7]. Serum tumor markers may be useful to diagnose malignancy, to detect cancer relapse, and, in some cases, to evaluate a cancer response to the treatment. CA-19-9, a tumor-associated antigen, is used as a tumor marker of cancers in gastrointestinal, lung, ovarian, and endometrial carcinoma. Such extremely elevation of CA-19-9 in case of retroperitoneal leiomyosarcoma has never been reported, so the increased CA-19-9 up to 70,000 U/mL played significant role in misidentifying pelvic mass as an ovarian tumor. Although there is a limitation to explain the cause of extremely increased serum CA-19-9, we speculated that two possibilities are implicated in this clinical situation. First, this tumor may be originated from a different primary tumor and represent serum marker of primary cancer cells. Secondly, the enhanced production of CA-19-9 could be stimulated by the inflammatory process induced from cancer cells metastasizing to peritoneum [8].
The pathological diagnosis of retroperitoneal mass before operation can aid planning an operation method. However, an exact preoperative diagnosis of retroperitoneal mass by aspiration biopsy is difficult and may cause complications such as infection, metastasis, or hemorrhage in abdominal cavity. Guz et al. [9] performed CT-guided aspiration biopsy on 3 retroperitoneal schwannoma patients, and all preoperative diagnoses provided incorrect results.
Surgically complete excision of tumor is the most crucial aspect in treatment for retroperitoneal leiomyosarcoma in early stage and successful complete removal is the significant prognostic factor to predict local recurrence and metastasis [10]. Nevertheless, there are several characteristics of the tumor making complete excision challenging, such as rapid growth of tumor which affect on the large size of tumor at the time of diagnosis, difficulty in dissecting from surrounding tissue, and metastasis of tumor to mesentery, lung, liver, or lymph nodes. Gronchi et al. [11] reported the complete excision rate varies from 54% to 88% when radical excision was done in retroperitoneal soft tissue sarcoma. The complete removal of tumor have been performed successfully without any complications such as massive hemorrhage, if preoperative consultation with other departments was thoroughly deliberated when a possibility of retroperitoneal tumor was presented with hydronephrosis and neurological symptoms.
Most of studies have shown local recurrence within 3 years after excision of primary mass, and particularly, Zhang et al. [12] reported that approximately 80% to 87% of all local recurrences become evident within 2 years and 100% are detected within 3 years. In cases of local tissue invasion or recurrence, chemotherapy and intrapelvic radiation therapy can be applied. Van Doorn et al. [13] reported postoperative high-dose radiation therapy in 13 of 34 retroperitoneal sarcoma patients with significantly decreased recurrence rate, nevertheless, the beneficial range of radiation therapy is limited unlike other soft tissue sarcoma. Also, the benefits and the effectiveness of radiation therapy have not been rigorously studied due to scarcity of cases. In cases of general metastasis, doxorubicin and ifosfamide are possible chemotherapy regimen, however, the exact usage and dosage have not been established clearly due to lack of cases [14,15].
In conclusion, a retroperitoneal-space-origin tumor must be ruled out even if it is located in ovarian fossa and has highly elevated serum level of CA-19-9. When a tumor of unknown primary site is excised from retroperitoneum, retroperitoneal leiomyosarcoma should be considered as one of the possible diagnosis. If tumor removal is attempted, the excision needs to be clean-cut without damaging nerves or vessels around the tumor and avoid causing any prospective complications.
Figures and Tables
Fig. 1
(A) A large, lobulated, and heterogenously enhancing mass occupies the right retroperitoneal space (arrow). (B) Intraoperative findings: a 9.4 × 6.3 × 5.1 cm sized smooth round mass (arrow) surrounded by light grayish membrane is attached to right retroperitoneal wall close to the right adnexa (arrowhead).
References
1. Kransdorf MJ. Malignant soft-tissue tumors in a large referral population: distribution of diagnoses by age, sex, and location. AJR Am J Roentgenol. 1995; 164:129–134.
2. Felix EL, Wood DK, Das Gupta TK. Tumors of the retroperitoneum. Curr Probl Cancer. 1981; 6:1–47.
3. Bretan PN Jr, Williams RD, Hricak H. Preoperative assessment of retroperitoneal pathology by magnetic resonance imaging: primary leiomyosarcoma of inferior vena cava. Urology. 1986; 28:251–255.
4. Hill MA, Mera R, Levine EA. Leiomyosarcoma: a 45-year review at Charity Hospital, New Orleans. Am Surg. 1998; 64:53–60.
5. Dalal KM, Kattan MW, Antonescu CR, Brennan MF, Singer S. Subtype specific prognostic nomogram for patients with primary liposarcoma of the retroperitoneum, extremity, or trunk. Ann Surg. 2006; 244:381–391.
6. Lewis JJ, Leung D, Woodruff JM, Brennan MF. Retroperitoneal soft-tissue sarcoma: analysis of 500 patients treated and followed at a single institution. Ann Surg. 1998; 228:355–365.
7. Van Rooij WJ, Martens F, Verbeeten B Jr, Dijkstra J. CT and MR imaging of leiomyosarcoma of the inferior vena cava. J Comput Assist Tomogr. 1988; 12:415–419.
8. Marcouizos G, Ignatiadou E, Papanikolaou GE, Ziogas D, Fatouros M. Highly elevated serum levels of CA-19-9 in choledocholithiasis: a case report. Cases J. 2009; 2:6662.
9. Guz BV, Wood DP Jr, Montie JE, Pontes JE. Retroperitoneal neural sheath tumors: Cleveland Clinic experience. J Urol. 1989; 142:1434–1437.
10. Hueman MT, Herman JM, Ahuja N. Management of retroperitoneal sarcomas. Surg Clin North Am. 2008; 88:583–597.
11. Gronchi A, Casali PG, Fiore M, Mariani L, Lo Vullo S, Bertulli R, et al. Retroperitoneal soft tissue sarcomas: patterns of recurrence in 167 patients treated at a single institution. Cancer. 2004; 100:2448–2455.
12. Zhang G, Chen KK, Manivel C, Fraley EE. Sarcomas of the retroperitoneum and genitourinary tract. J Urol. 1989; 141:1107–1110.
13. Van Doorn RC, Gallee MP, Hart AA, Gortzak E, Rutgers EJ, van Coevorden F, et al. Resectable retroperitoneal soft tissue sarcomas: the effect of extent of resection and postoperative radiation therapy on local tumor control. Cancer. 1994; 73:637–642.
14. Todd CS, Michael H, Sutton G. Retroperitoneal leiomyosarcoma: eight cases and a literature review. Gynecol Oncol. 1995; 59:333–337.
15. Sutton G, Blessing JA, Malfetano JH. Ifosfamide and doxorubicin in the treatment of advanced leiomyosarcomas of the uterus: a Gynecologic Oncology Group study. Gynecol Oncol. 1996; 62:226–229.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download