Abstract
Physiologic pituitary enlargement is common during normal pregnancy. However, symptoms such as diplopia, blurred vision and headache resulting from physiologic pituitary enlargement are very rare during pregnancy. A 39-year-old woman complained of sudden diplopia and left eye ptosis at 33th weeks of gestation. An magnetic resonance imaging (MRI) demonstrated the pituitary enlargement compressing the optic chiasm. Notwithstanding the medication of bromocriptine, her symptoms did not regress during pregnancy. At 5 months after delivery, her symptoms dramatically resolved without any surgery, and her visual acuity was normalized. Her MRI scan also revealed more decreased size of pituitary gland compared to antenatal MRI. We report a case of visual loss due to the physiologic pituitary enlargement of nonfunctioning adenoma during pregnancy, which regressed spontaneously after delivery without any surgery.
The pituitary gland undergoes global hyperplasia during pregnancy because more estrogen stimulates hyperplasia of lactotrophes. Some studies have revealed that the size of pituitary gland increases an average of 120% during normal pregnancy [1]. The physiologic enlargement of pituitary gland during pregnancy usually does not expand to the extrasellar area to cause symptoms such as headache or blurred vision [1]. Prolactin secreting adenomas are the most commonly encountered pituitary tumors in women of child bearing age. However, undiagnosed pituitary tumor during pregnancy is not common, because prolactinoma is related with infertility or reproductive dysfunction [1]. We here report a rare case of developed diplopia and left ptosis resulting from the enlargement of nonfunctioning pituitary adenoma during pregnancy that have not been diagnosed before pregnancy.
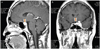
A 39-year-old nulliparous women visited our institution at 34th weeks of gestation with 1-week history of sudden diplopia and left ptosis. After a review by the obstetrician, she was admitted to the high risk pregnancy unit. We consulted neurologist, endocrinologist and ophthalmologist for a review. She had relatively regular menstruation cycle before pregnancy. Therefore, she had not been examined any evaluations for pituitary gland or pituitary hormones before pregnancy. There were no specific past medical or operative histories. Neurologic examination revealed the limitation of her left eye movement to the medial, superior and inferior directions. Magnetic resonance imaging (MRI) demonstrated a macroadenoma with the size of 1.5×1.3×1.0 cm, which was lobulated with suprasellar extension and compression of the optic chiasm. It encased the left cavernous sinus and internal carotid artery (Fig. 1). The narrowing of internal carotid artery by the tumor caused the third nerve palsy. Endocrine tests indicated that prolactin, cortisol and estriol (E2) levels were elevated: prolactin was 176.3 ng/mL; cortisol was at 36.0 µg/dL; E2 was >1,000 pg/mL. There were no features of diabetes insipidus. Serum electrolytes and paired serum/urine osmolalities were within normal limits. Obstetric ultrasound revealed a live singleton fetus weighing 2,390 g with vertex presentation and a 4.7 cm sized myomatous nodule on anterior uterine body.
We initiated dopamine agonist therapy with 1.25 mg once for 2 days, titrated up to the maximum tolerated dose of bromocriptine 2.5 mg three times daily. She was discharged after confirming fetal well-being and treated on outpatient basis. She was commenced on hydrocortisone replacement because, her symptoms had not been improved despite the bromocriptine medication. However, there was no significant her visual field improvement during pregnancy. She complained of depression and fear of irreversible visual loss.
At 39+3 weeks, she delivered a healthy baby boy by vacuum extracted delivery. The patient and the newborn were discharged without complications after delivery. On the second postpartal day, she lifted her left eyelid slightly. The symptoms gradually regressed with clinical improvement. On the 16th day after delivery she opened her left eye more than half and moved her eye to the medial direction. And after 1 month, diplopia disappeared and neurologic examination showed no residual visual defect. She reduced bromocriptine and prednisolone to once a day for five days and then stopped. A pituitary MRI after 5 months of postpartum revealed the decreased size (1.3×1.1×0.7 cm) of the pituitary mass (Fig. 2) and the serum levels of prolactin (14.9 ng/mL) and cortisol (16.1 µg/mL) were also normalized.
The pituitary gland normally enlarges during pregnancy, predominantly because of the hyperplasia of prolactin producing lactotroph cells. Both estrogen and progesterone stimulate the synthesis of prolactin. Serum prolactin level is gradually increased with a parallel increase in the size and number of lactotroph cells during pregnancy [2]. The lactotroph hyperplasia starts in early pregnancy and then disappears spontaneously within 2 weeks to 6 months after delivery [3].
The size of the pituitary gland may expand an average of 120% during a normal pregnancy compared to prepregnancy [1]. It is difficult to differentiate the pathologic diagnoses of pituitary enlargement during pregnancy because MRI is not sufficiently sensitive to specific diseases. Moreover, a normally elevated prolactin level during pregnancy also hinders the diagnosis of pathologic pituitary gland [4].
The height of the pituitary gland is correlated to gestational age (0.08 mm per week) but it seldom increases to more than 10 mm during pregnancy [1]. Pituitary height higher than 9 to 10 mm during pregnancy may arouse suspicion of a pathological reason [5]. The pituitary gland of our patient had enlarged to 15 mm in height, which was larger than that of reported physiological enlargement of pituitary glands during pregnancy. Our patient's MRI demonstrated the asymmetric enlargement and deviation of the stalk, which is not typical for physiologic enlargement of a pituitary gland. This finding may indicate that her pathologic pituitary mass may be adenoma.
Interestingly nonfunctioning adenomas are very rare during pregnancy, since fertility is usually impaired.
Prolactinoma is the most common cause of pituitary enlargement during pregnancy. Prolactinoma is responsive to bromocriptine treatment and resolves dramatically after delivery. However, our patient's clinical presentation was not compatible with prolactinoma, because her symptoms did not improve with aggressive dopamine therapy. Furthermore, her pituitary mass did not return to normal range after delivery though the size of the mass significantly decreased following delivery. Actually, in our case, the definite diagnosis was remained uncertain because of the lack of surgical intervention and histology. We speculated that the combined factors of physiologic enlargement and incidentally detected pituitary adenoma during pregnancy influenced on her sudden developed symptoms such as blurred vision, ptosis, and headache during pregnancy. Fortunately, her symptoms resulting from mass effect resolved postpartum, with the decrease of the size of the adenoma. We here report a rare case of nonfunctiong pituitary macroadenoma during pregnancy.
Figures and Tables
References
1. Dinc H, Esen F, Demirci A, Sari A, Resit Gumele H. Pituitary dimensions and volume measurements in pregnancy and post partum. MR assessment. Acta Radiol. 1998; 39:64–69.
2. Molitch ME. Pituitary diseases in pregnancy. Semin Perinatol. 1998; 22:457–470.
3. Foyouzi N, Frisbaek Y, Norwitz ER. Pituitary gland and pregnancy. Obstet Gynecol Clin North Am. 2004; 31:873–892.
4. Inoue T, Hotta A, Awai M, Tanihara H. Loss of vision due to a physiologic pituitary enlargement during normal pregnancy. Graefes Arch Clin Exp Ophthalmol. 2007; 245:1049–1051.
5. Wolpert SM, Molitch ME, Goldman JA, Wood JB. Size, shape, and appearance of the normal female pituitary gland. AJR Am J Roentgenol. 1984; 143:377–381.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download