Abstract
Objective
To investigate the prevalence of subclinical hypothyroidism (SH) diagnosed by thyrotropin-releasing hormone (TRH) stimulating test in infertile women with basal thyroid-stimulating hormone (TSH) levels of 2.5 to 5.0 mIU/L.
Methods
This study was performed in 39 infertile women with ovulatory disorders (group 1) and 27 infertile women with male infertility only (group 2, controls) who had basal serum TSH levels of 2.5 to 5.0 mIU/L and a TRH stimulating test. Serum TSH levels were measured before TRH injection (TSH0) and also measured at 20 minutes (TSH1) and 40 minutes (TSH2) following intravenous injection of 400 µg TRH. Exaggerated TSH response above 30 mIU/L following TRH injection was diagnosed as SH. Group 1 was composed of poor responders (subgroup A), patients with polycystic ovary syndrome (subgroup B) and patients with WHO group II anovulation except poor responder or polycystic ovary syndrome (subgroup C).
Results
The prevalence of SH was significantly higher in group 1 of 46.2% (18/39) compared with 7.4% (2/27) in group 2 (P=0.001). TSH0, TSH1, and TSH2 levels were significantly higher in group 1 than the corresponding values in group 2 (P<0.001, P<0.001, P<0.001). In group 1, TSH1 and TSH2 levels were significantly lower in subgroup C compared with those in subgroup A and B (P=0.008, P=0.006, respectively).
Subclinical hypothryrodism (SH) is defined as an abnormaly high thyroid-stimulating hormone (TSH) level with a normal free thyroxine (FT4) level, and without frank symptoms of hypothyroidism [1]. The prevalence of SH is about 4% to 8.5% in the general population [2,3], and significantly higher in patients with infertility [4]. Patients with SH is usually asymptomatic, but they have 2% to 5% annual risk of progression to overt hypothryroidism as an early stage of hypothroidism [3]. The increased need for thyroid hormones during pregnancy can leads to an aggravation of SH in pregnant women [3].
Hypothyroidism is related with menstrual disturbances, infertility, increased risk of miscarriage, obstetrical complications and adverse outcomes in the offspring [5]. Women with antithyroid antibodies (ATAs) may be at an increased risk of miscarriage and obstetrical complications even in a SH and euthyroid state [5,6]. Thyroid hormones have direct effects on granulosa cells, corpus luteum and oocytes and therefore Increased TSH and thyrotropin-releasing hormone (TRH) can cause ovulatory dysfunction or corpus luteum dysfuction [7]. Also, thyroid underfunction can affect the ovarian function indirectly by decreased binding activity of sex hormone binding globulin, increased prolactine levels and delayed luteinizing hormone response to gonadotropin-releasing hormone [7,8]. Actually, it has been reported that 11% to 24% of infertile women with ovulatory dysfunction or corpus luteal problems have SH [9].
If infertile patients or women planning pregnancy are diagnosed as SH as well as overt hypothyroidism, they are recommended to be treated to reduce risks of miscarriage and fetal developmental impairment and to improve the in vitro fertilization outcome [3,10]. Therefore, it is necessary to identify patients with not only overt hypothyroidism but also even SH. Some scholars suggest that the upper limit of normal value for serum TSH level should be 2.5 mIU/L in a population requiring a rigorous screening to exclude thyroid disease [11], because it is likely that the individuals with serum TSH between 2.5 and 5.0 mIU/L include patients with early stage SH. Therefore, the strict screening for excluding thyroid disease including even early stage SH is required in infertile patients with serum TSH 2.5 to 5.0 mIU/L.
The TRH stimulation test is widely used to identify the patients with SH, especially in the field of gynecologic endocrinology [7,12]. This test can be useful for identifying the patients with the early stage of SH in women with serum TSH levels of 2.5 to 5.0 mIU/L. Although there is no definite cut-off value of TRH stimulation test for the diagnosis of SH, most investigators have used a cut-off value for stimulated TSH of >20-30 µU/L. Abnormal response to the TRH stimulation, defined as exaggerated TSH reponse to TRH challenge means early stage SH.
Recently, several clinical studies to investigate the prevalence of SH in infertile women have been attempted but results have been very limited. Moreover, the prevalance of SH diagnosed by TRH stimulation test in Korean women with TSH 2.5 to 5.0 mIU/L as well as the prevalance of SH in Korean infertile women have not been reported. Therefore, we performed this study to assess the prevalance of SH diagnosed by TRH stimulation test in Korean infetile patients with serum TSH levels of 2.5 to 5.0 mIU/L who have ovulatory disorder and male infertility only.
This retrospective cohort study included 39 infertile patients with ovulatory disorder (group 1) and 27 patients with male infertility only (group 2, control) who had a TRH stimulation test in our reproductive medicine and infertility clinic between January 2010 and September 2012. A TRH stimulation test was performed in 78 of 289 consecutive infertile patients with ovulatory disorder or male infertility when basal TSH level was between 2.5 and 5.0 mIU/L. All women included in the present study were between 20 and 41 years of age and had a body mass index between 18 and 25 kg/m2. Twelve patients who had any endocrine and metabolic disorders such as diabetes mellitus, overt hypothyroidism, and a history of hyperprolactinemia, treatment with dopaminergic agent and previous (within 12 months) or current abuse of alcohol or drugs were excluded from this study. The institutional review board of the University of Ulsan College of Medicine, Asan Medical Center, approved the study.
A TRH stimulation test was performed at the next visit after measuring basal TSH level in patients who met the inclusion criteria. Serum TSH levels were measured before TRH (Relefact; Aventis, Frankfurt, Germany) injection (TSH0) and also measured at 20 minutes (TSH1) and 40 minutes (TSH2) following intravenous injection of 400 µg TRH. Exaggerated TSH response above 30 mIU/L at 20 or 40 minutes following TRH injection was considered SH [13]. Group 1 including patients with ovulatory disorders was composed of poor responders (subgroup A, n=12), patients with polycystic ovary syndrome (PCOS) (subgroup B, n=14) and patients with World Health Organization (WHO) group II anovulation except poor responder or PCOS (subgroup C, n=13). The diagnosis of poor responder was based on the Bologna criteria of the 2011 European Society of Human Reproduction and Embryology consensus [14]. PCOS was diagnosed according to the revised criteria of the 2003 Rotterdam consensus [15].
Serum TSH was measured by immunoradiometric assay using a TSH-CTK-3 kit (DiaSorin SpA, Saluggia, Italy) with interassay and intraassay variances of <10% and 5%, respectively.
Mean values were expressed as mean±standard deviation. Statistical analysis of the results was performed using Student's t-test and Kruscal-Wallis test with post-hoc Bonferroni test for comparing the mean values. Chi-square test and Fisher's exact test were used for the comparisons of fraction. A P-value of <0.05 was considered statistically significant. All analyses were performed using the SPSS ver. 11.0 (SPSS Inc., Chicago, IL, USA).
There were no differences in patients' characteristics such as the age of patients, infertility duration, body mass index and antimüllerian hormone except antral follical count between the two groups (Table 1). Antral follical count was significantly higher in the group 1 than in the group 2. The basal serum TSH (TSH0) levels in the group 1 were significantly higher than in the group 2 (P=0.010). TSH levels measured at 20 minutes and 40 minutes following TRH injection (TSH1 and TSH2) were also higher in the group 1 than those in the group 2 (P<0.001, P<0.001). The prevalence of SH was significnatly higher in the group 1 of 46.2% (18/39) compared with 7.4% (2/27) in the group 2 (P=0.001) (Table 2). In the group 1, SH prevalence in the subgroup A consisting of poor responders was significantly higher than that in the subgroup C including patients with WHO group II anovulation except poor responder or PCOS (P=0.047). TSH1 and TSH2 levels were significantly lower in the subgroup C, as compared with those in the subgroup A and B (P=0.008, P=0.006, respectively) (Table 3).
It is well known that overt hypothyroidism frequently results in ovulatory dysfunction, impaired fertility and unfavorable outcome for both mother and fetus, and these problems are improved by restoring the euthyroid state [3,5,6,7,8,9,10]. Especially, maternal overt hypothyroidism during pregnancy leads to serious psychoneurological consequences for the offspring [5,16]. Therefore, thyroid evaluation has become an essential test for infertile women. In infertile women with overt hypothyroidism, early detection and immediate treatment are certainly needed before treatment for infertility. Even in SH, adequate treatment for this condition has been recommended to reduce the risks of embryo implantation failure, miscarriage and delayed fetal development [3,10].
SH is a common disorder in general population, and its prevalence is reported to be higher in infertile women of 13.9% compared with 3.9% in healthy fertility-proven women [4]. The prevalence of SH reported in infertile women is variable. The variability of prevalence of SH may be related to the causes of infertility. A recent study assessed the prevalence of SH after administering TRH stimulation test in women with normal TSH levels. This study demonstrated that the prevalence of SH is significantly higher in infertile women with ovulatory disorders of 20.5% compared with 8.3% in women with other causes of infertility [13].
Among women with normal serum TSH concentrations, progression rate to over hypothyroidism and the prevalence of antithyroid antibodies were higher in individuals with serum TSH higher than 2.5 mIU/L compared with those with serum TSH levels of 0.5 to 2.5 mIU/L [17]. These results suggest that the patients with the early stage of SH can be included among the women with serum TSH between 2.5 and 5.0 mIU/L. Rigorous evaluation for excluding thyroid disease including early stage SH is needed in infertile women contemplating pregnacy. Therefore, we performed a TRH stimulation test to identify some patients with the early stage of SH among those with serum basal TSH levels of 2.5 to 5.0 mIU/L.
In the present study, the prevalence of SH was significantly higher in patients with ovulatory disorders than in the control group composed of patients with male infertility only. The prevalence of SH in patients with ovulatory disorders was higher in our study of 46.2% compared with 20.5% in the previous study by Eldar-Geva et al. [13]. Only infertile patients having normal serum TSH levels higher than 2.5 mIU/L were included in our study, while patients included in the study by Eldar-Geva et al. [13] had normal serum TSH levels of 0.4 to 5.0 mIU/L. This difference between the two studies can result in the difference in the prevalence of SH among infertile women with ovulatory disorders.
In our study, basal serum TSH levels as well as TSH levels masured before TRH injection and at 20 and 40 minutes after TRH administrtion were significantly higher in ovulatory disorder group. Thyroid underfunction induces an increase of TRH and a decrease of dopamine levels, which stimulate prolactin secretion. In addition, this condition causes the decrease of binding activity of sex hormone binding globulin which results in the increase of serum free estradiol and testosterone levels, thereby altering the hypothalamic-pituitary-ovarian axis [7,8]. Therefore, thyroid underfunction is closely related to the ovulatory dysfunction.
SH is likely to be more common in infertile women and it can be aggravated during or after controlled ovarian stimulation as well as during pregnancy [13]. In addition, it has been reported that fertility is improved by thyroxine therapy in infertile patients with SH [3,10,18] although SH has never been proven to be a cause of infertility. These findings suggest that early detection and appropriate management of SH is very important in infertile women planning pregnancy. However, even studies on the prevalence of SH in infertile women is very limited and its prevalence in Korean women with infertility has not been reported yet. Moreover, the prevalence of SH among infertile women with basal serum TSH concentrations of 2.5 to 5.0 mIU/L is not elucidated yet and the clinical significance of serum TSH between 2.5 and 5.0 mIU/L is still controversial. Reduced thyroid function is closely related to the ovulatory dysfunction. Therefore, we investigated the prevalence of SH in infertile women with ovulatory dysfunction who had basal serum TSH levels of 2.5 to 5.0 mIU/L. We used TRH stimulation test for diagnosis of early stage SH. Even the ealiest stage of SH can be detected by exaggerated response to TRH. Although there are debates on the reliablity of the TRH stimulation test as infertility screening tool, this test is widely accepted as a diagnostic tool for detection of early stage SH with normal TSH level. It is clear to treat the patients who has overt hyperthyroidism and SH with serum TSH above 5.0 mIU/L especially in pregnant women and women contemplating pregnacy. However, the treatment for infertile patients with serum TSH level of 2.5 to 5.0 mIU/L who endeavor to achieve pregnancy is still controversial. Thus, we performed a TRH stimulation test in infertile patients with basal serum TSH levels between 2.5 and 5.0 mIU/L. A TRH stimulation test may be useful for confirmation as well as earlier detection of SH especially in these patients.
In the present study, infertile patients with ovulatory disorders were divided into poor responders, PCOS group and WHO group II anovulation except poor responder or PCOS according to the underlying causes of ovulatory disorders. In patients with ovulatory disorders, the prevalence of SH was comparable among three subgroups. However, our data showed that TSH levels measured at 20 and 40 minutes following TRH injection were significantly lower in patients with WHO group II anovulation except poor responder or PCOS than in poor responders and PCOS patients. It is not easy to explain the reason for these results, and further large-scale studies are needed for the confirmation of our results.
In conclusion, TRH stimulation test is needed in infertile women with ovulatory disorders who have normal TSH levels particularly between 2.5 and 5.0 mIU/L in order to enable the early detection and appropriate treatment of SH.
Figures and Tables
Table 2
Prevalence of SH and TSH levels before and after 400 mcg thyrotropin-releasing hormone injection in ovulatory disorder group and control group

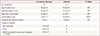
Table 3
Prevalence of SH and TSH levels before and after 400 mcg thyrotropin-releasing hormone injection in three subgroups of ovulatory disorder group

Values are means±standard deviation or number (%).
SH, subclinical hypothyroidism; TSH, thyroid-stimulating hormone; PCOS, polycystic ovary syndrome; WHO, World Health Organization; NS, not significant.
a)Kruscal-Wallis test with post-hoc Bonferroni test; b)Significantly lower than in the poor responder or PCOS group (P=0.028, P=0.016, respectively); c)Significantly lower than in the poor responder or PCOS group (P=0.010, P=0.023, respectively); d)Fisher's exact test; e)Between the poor responder group and WHO II anovulation group except PCOS or poor responder.
References
1. Ross DS. Serum thyroid-stimulating hormone measurement for assessment of thyroid function and disease. Endocrinol Metab Clin North Am. 2001; 30:245–264.
2. Poppe K, Velkeniers B, Glinoer D. The role of thyroid autoimmunity in fertility and pregnancy. Nat Clin Pract Endocrinol Metab. 2008; 4:394–405.
3. Surks MI, Ortiz E, Daniels GH, Sawin CT, Col NF, Cobin RH, et al. Subclinical thyroid disease: scientific review and guidelines for diagnosis and management. JAMA. 2004; 291:228–238.
4. Abalovich M, Mitelberg L, Allami C, Gutierrez S, Alcaraz G, Otero P, et al. Subclinical hypothyroidism and thyroid autoimmunity in women with infertility. Gynecol Endocrinol. 2007; 23:279–283.
5. Poppe K, Glinoer D. Thyroid autoimmunity and hypothyroidism before and during pregnancy. Hum Reprod Update. 2003; 9:149–161.
6. Kim CH, Chae HD, Kang BM, Chang YS. Influence of antithyroid antibodies in euthyroid women on in vitro fertilization-embryo transfer outcome. Am J Reprod Immunol. 1998; 40:2–8.
7. Bals-Pratsch M, De Geyter C, Muller T, Frieling U, Lerchl A, Pirke KM, et al. Episodic variations of prolactin, thyroid-stimulating hormone, luteinizing hormone, melatonin and cortisol in infertile women with subclinical hypothyroidism. Hum Reprod. 1997; 12:896–904.
8. Col NF, Surks MI, Daniels GH. Subclinical thyroid disease: clinical applications. JAMA. 2004; 291:239–243.
9. Franklyn J. 'Subclinical hypothyroidism': to treat or not to treat, that is the question. Clin Endocrinol (Oxf). 1995; 43:443–444.
10. Kim CH, Ahn JW, Kang SP, Kim SH, Chae HD, Kang BM. Effect of levothyroxine treatment on in vitro fertilization and pregnancy outcome in infertile women with subclinical hypothyroidism undergoing in vitro fertilization/intracytoplasmic sperm injection. Fertil Steril. 2011; 95:1650–1654.
11. American Association for Clinical Chemistry. National Academy of Clinical Biochemistry laboratory medicine practice guidelines [Internet]. Washington, DC: American Association for Clinical Chemistry;2014. cited 2014 Oct 6. Available from: http://www.nacb.org/lmpg/main.stm.
12. Raber W, Vierhapper H. The usefulness of thyrotropin-releasing hormone stimulation test in subfertile female patients. Gynecol Endocrinol. 2008; 24:359–360.
13. Eldar-Geva T, Shoham M, Rosler A, Margalioth EJ, Livne K, Meirow D. Subclinical hypothyroidism in infertile women: the importance of continuous monitoring and the role of the thyrotropin-releasing hormone stimulation test. Gynecol Endocrinol. 2007; 23:332–337.
14. Ferraretti AP, La Marca A, Fauser BC, Tarlatzis B, Nargund G, Gianaroli L, et al. ESHRE consensus on the definition of 'poor response' to ovarian stimulation for in vitro fertilization: the Bologna criteria. Hum Reprod. 2011; 26:1616–1624.
15. Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004; 81:19–25.
16. Baskin HJ, Cobin RH, Duick DS, Gharib H, Guttler RB, Kaplan MM, et al. American Association of Clinical Endocrinologists medical guidelines for clinical practice for the evaluation and treatment of hyperthyroidism and hypothyroidism. Endocr Pract. 2002; 8:457–469.
17. Vanderpump MP, Tunbridge WM, French JM, Appleton D, Bates D, Clark F, et al. The incidence of thyroid disorders in the community: a twenty-year follow-up of the Whickham Survey. Clin Endocrinol (Oxf). 1995; 43:55–68.
18. Verma I, Sood R, Juneja S, Kaur S. Prevalence of hypothyroidism in infertile women and evaluation of response of treatment for hypothyroidism on infertility. Int J Appl Basic Med Res. 2012; 2:17–19.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download