Abstract
Omental torsion is a rare cause of acute abdominal pain. It presents with nonspecific symptoms and signs of an acute abdomen, making it difficult to diagnose preoperatively, because symptoms mimic those caused by other conditions such as appendicitis, cholecystitis, diverticulitis, and other gynecologic diseases. Computed tomography is an effective and useful method to diagnose and exclude other acute abdominal conditions. Our case presented with sudden right upper abdominal pain with tenderness, rebound tenderness, mild fever (37.2℃), increased erythrocyte sedimentation rate (37 mm/hr), increased high-sensitivity C-reactive protein level (5.97 mg/dL). Computed tomography showed a large, well-circumscribed heterogeneous fatty mass and a 7.3 cm subserosal myoma. We could not exclude the myoma as the cause of acute abdominal pain, so we performed an emergency operation with suspicion of omental torsion or necrotic degeneration of the myoma. During the operation, we diagnosed primary omental torsion with infarction and subserosal myoma without secondary degeneration.
Omental torsion and infarction are rare and unusual causes of acute abdominal pain. Omental infarction was first described by Bush in 1896 [1], and Eitel in 1899 [2] reported a case of omental torsion. Very few cases have been reported in adults [3]. Omental torsion is caused by twisting of parts of the omentum around its axis, resulting in perfusion defects and vascular compromise, which cause simple edema, infarction, or ischemia [4]. Omental torsion presents with nonspecific symptoms and signs of an acute abdomen, so it can mimic other causes of acute abdominal pain such as appendicitis, cholecystitis, diverticulitis, renal stones, and other gynecologic diseases. Therefore, surgeons should consider omental torsion in the preoperative differential diagnosis of acute abdomen.
We report an uncommon case of primary omental torsion with infarction that was definitively diagnosed during hysterectomy for a subserosal myoma.
A 49-year-old woman scheduled to undergo a hysterectomy because of a uterine myoma visited the emergency department complaining of right upper quadrant abdominal pain one week before her scheduled operation. She appeared to be acutely ill. Her symptoms had started 1 day before her admission and had increased in severity in the hours before she visited the emergency department. The pain was severe and progressive. Tenderness and rebound tenderness on the right side of the umbilicus were noted, and lesser pain and tenderness on the lower abdomen was found. The patient did not complain of symptoms such as anorexia, nausea, vomiting, or diarrhea.
There was nothing remarkable in the patient's prior medical history. She had given birth twice previously by cesarean section 30 years prior. Her menstrual cycle was regular. A physical examination revealed a body temperature of 37.2℃ and blood pressure of 154/93 mmHg, and her pulse rate was 83 beats/min with a regular rhythm. Erythrocyte sedimentation rate (37 mm/hr) and high-sensitivity C-reactive protein (5.97 mg/dL) were above the normal ranges; all other laboratory test parameters were within normal limits.
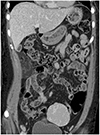
Computerized tomography (CT) scan showed focal, ovoid, fatty infiltration in the right upper abdomen, with a concentric distribution of fibrous and fatty folds converging toward the torsion with edema. The vascular pedicle extended caudally and entered a large, well-circumscribed heterogeneous fatty mass. A 7.3-cm subserosal myoma was also observed in the uterus (Fig. 1).
Although the patient was scheduled to undergo a hysterectomy the following week, we could not exclude the myoma as the cause of acute abdominal pain, so we performed an emergency operation the day of her admission with suspicion of omental torsion or necrotic degeneration of the myoma. During the operation, a 10.0×8.0 cm dark brown clockwise torsion with infarction changes was observed in the right side of the greater omentum. There is no adhesion and any other connection between omentum and uterine myoma. A partial omentectomy was therefore performed followed by a total abdominal hysterectomy due to the presence of the uterine myoma. We confirmed an omental hemorrhagic infarction by primary torsion and subserosal myoma without degeneration by biopsy (Fig. 2).
Omental torsion is an unusual and infrequent cause of acute abdomen in the adult population [3]. Omental torsion occurs mainly between the 3rd to 5th decades of life with a male predominance [5]. Omental torsion of the right side is more frequent than that of the left side, because of the greater length and mobility of the omentum on the right side of the body [6]. Epstein et al. [7]. attributed this to the different embryological origin of the right side of the omentum than the left side of the omentum, and the right omentum having congenitally anomalous fragile blood vessels, predisposing it to venous thrombosis. Most patients with omental torsion therefore present with sudden right abdominal pain that is enhanced by abdominal movement with signs of tenderness and rebound tenderness that may be accompanied by nausea, vomiting, and low grade fever [5]. Our patient had clinical manifestations of omental torsion; sudden right upper abdominal pain with tenderness, rebound tenderness, mild fever (37.2℃ ), increased ESR (37 mm/hr), and increased HS-CRP level (5.97 mg/dL), but she did not have nausea, vomiting, or leukocytosis.
Omental torsion is either primary or secondary. The etiology is not clear in idiopathic primary omental torsion, but anatomical variations of the omentum and actions that displace the omentum such as obesity, sudden position changes, rigorous exercise, bicycle racing, hard labor, coughing, trauma of the abdominal wall, and hyperperistalsis after a heavy meal are considered to be risk factors [4,8,9]. Secondary omental torsion is more common than primary omental torsion and is associated with pre-existing pathologies such as cysts, tumors, inflammation, hernias, adhesions, or scarring or surgical wounds due to prior surgery [10]. These factors may cause the omentum to twist around a pivotal point, usually in a clockwise direction. Engorgement of tortous veins, which are easily compressed, may compromise venous return, causing the distal omentum to become congested and edematous [11]. As torsion progresses, arterial occlusion leads to acute hemorrhagic infarction, and necrosis of the omentum will eventually occur [12]. Our patient had primary idiopathic omental torsion without any predisposing factors; the torsion was clockwise and accompanied by hemorrhagic infarction.
Omental torsion is difficult to diagnose preoperatively due to the nonspecific clinical symptoms and signs, therefore it is often misdiagnosed. The most likely differential diagnoses include acute appendicitis, acute cholecystitis, diverticulitis, and other gynecologic diseases such as ovarian cyst torsion, rupture, and secondary degeneration of a myoma [3,4,9]. CT is an effective and useful modality to diagnose omental torsion and exclude other acute abdominal conditions [13]. CT scans of omental torsion often show a whirling pattern of fibrous, fatty folds or an infarcted omentum as an area of high-attenuated fat containing hyperattenuated streaks just beneath the parietal peritoneum [13]. However, definitive diagnosis is most usually established at the time of exploratory surgery. In most cases, the standard treatment for omental torsion is resection of the involved segment of the omentum, and laparoscopy is more useful than laparotomy as the diagnostic and therapeutic method of choice [14]. Earlier preoperative diagnosis by CT can help avoid surgery, and in selected cases may lead to conservative treatment without complications. Some papers have reported successful recovery with conservative management [5,13,15]. However, because we could not exclude the myoma as the cause of acute abdominal pain, we performed an emergency operation on the day of the patient's admission due to suspicion of omental torsion and/or myoma degeneration. During the operation, we diagnosed primary omental torsion with infarction and a subserosal myoma without secondary degeneration.
In conclusion, primary omental torsion presents with nonspecific symptoms and signs of an acute abdomen, making preoperative diagnosis difficult. CT scanning is very useful for earlier diagnosis as it can rule out various other causes of acute abdomen. Although surgical removal is required for infarcted omental torsion, conservative treatment can be considered in some uncomplicated cases. Therefore, surgeons, including gynecologists, should always consider omental torsion in the differential diagnosis of acute abdomen.
Figures and Tables
References
1. Bush P. A case of hæmorrhage into the great omentum. Lancet. 1896; 147:286.
2. Eitel GG. Rare omental torsion. NY Med Rec. 1899; 55:715–716.
3. Basson SE, Jones PA. Primary torsion of the omentum. Ann R Coll Surg Engl. 1981; 63:132–134.
4. Adams JT. Torsion of the omentum: abdominal wall, omentum, mesentery and retroperitoneum. In : Schwartz SI, Shires GT, Spencer FC, editors. Principles of surgery. 5th ed. New York: McGraw-Hill;1989. p. 1495–1496.
5. Tsironis A, Zikos N, Bali C, Pappas-Gogos G, Koulas S, Katsamakis N. Primary torsion of the greater omentum: report of two cases and review of the literature. Int J Surg. 2007; 17:12884.
6. Puylaert JB. Right-sided segmental infarction of the omentum: clinical, US, and CT findings. Radiology. 1992; 185:169–172.
7. Epstein LI, Lempke RE. Primary idiopathic segmental infarction of the greater omentum: case report and collective review of the literature. Ann Surg. 1968; 167:437–443.
8. Theriot JA, Sayat J, Franco S, Buchino JJ. Childhood obesity: a risk factor for omental torsion. Pediatrics. 2003; 112(6 Pt 1):e460.
9. Van Breda Vriesman AC, Lohle PN, Coerkamp EG, Puylaert JB. Infarction of omentum and epiploic appendage: diagnosis, epidemiology and natural history. Eur Radiol. 1999; 9:1886–1892.
10. Young TH, Lee HS, Tang HS. Primary torsion of the greater omentum. Int Surg. 2004; 89:72–75.
11. Andreuccetti J, Ceribelli C, Manto O, Chiaretti M, Negro P, Tuscano D. Primary omental torsion (POT): a review of literature and case report. World J Emerg Surg. 2011; 6:6.
12. Karayiannakis AJ, Polychronidis A, Chatzigianni E, Simopoulos C. Primary torsion of the greater omentum: report of a case. Surg Today. 2002; 32:913–915.
13. Kim J, Kim Y, Cho OK, Rhim H, Koh BH, Kim YS, et al. Omental torsion: CT features. Abdom Imaging. 2004; 29:502–504.
14. Costi R, Cecchini S, Randone B, Violi V, Roncoroni L, Sarli L. Laparoscopic diagnosis and treatment of primary torsion of the greater omentum. Surg Laparosc Endosc Percutan Tech. 2008; 18:102–105.
15. Nubi A, McBride W, Stringel G. Primary omental infarct: conservative vs operative management in the era of ultrasound, computerized tomography, and laparoscopy. J Pediatr Surg. 2009; 44:953–956.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download