Abstract
Perivascular epithelioid cell neoplasm (PEComa) is a rare tumor with unknown malignant potential. We report a case of a 6-year-old child with history of brain tumor (pineoblastoma), who presented with intermittent vaginal spotting for 6 months. A vaginoscopy revealed a 1.5×1.0-cm mass on the vaginal wall. Pathological examination demonstrated that the tumor was composed of clear cells with organoid patterns, which were immunohistochemically positive for HMB-45 and TFE3, and negative for CK, HNF1-B, SOX10, Melan A, and S-100 protein. These findings were consistent with PEComa arising from the vagina. Regular follow-up with magnetic resonance imaging has shown no signs of recurrence. This case shows that early detection of PEComa and subsequent regular follow-ups are important because of the neoplasm's unknown malignant potential.
Perivascular epithelioid cell neoplasms (PEComas) were first described by Bonetti et al. in 1992 [1]. They are rare soft tissue neoplasms with histologically and immunohistochemically distinct perivascular epithelioid cells [2]. They present with clear and acidophilic cytoplasm, perivascular distribution, and immunoreactivity for melanocytic markers such as HMB-45 [3]. They have been described in the liver, lung, pancreas, rectum, and female genital tract [4,5,6]. There have been four reported cases of vaginal PEComas in the literature, two of which were in pediatric patients [6,7,8,9]. Here, we present an extremely rare case of a vaginal PEComa in a 6-year-old girl.
A 6-year-old girl presented with intermittent vaginal spotting for 6 months. Her urinalysis at a local clinic showed a 2+ positive occult blood test without any other abnormality. The patient was referred to our hospital for further evaluation. She had been diagnosed with pineoblastoma at the age of 2, for which she received three cycles of neoadjuvant chemotherapy and underwent tumor resection. She has been followed up regularly, and her pineoblastoma has been in complete remission without the need for any additional treatment. Her family history was unremarkable. Physical examination and laboratory results were normal except for the 2+ occult blood result on urinalysis. Follicle-stimulating hormone, luteinizing hormone, estradiol and thyroid-stimulating hormone levels were also normal.
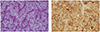
Transabdominal ultrasound showed a normal prepubertal uterus, 2.8 cm in length. Instead of ordering additional imaging studies, we decided to perform a vaginoscopy. Under general anesthesia, she was placed in lithotomy position. Twenty-seven French hysteroscope was gently inserted into her vagina. Using the optical part of the scope, the entire lining of the vagina was inspected. And it revealed a 1.5×1.0-cm benign looking mass arising from the left lateral vaginal wall (Fig. 1A). The mass was completely resected with a wire electrode called cutting loop with clear margins (Fig. 1B). We electrocoagulated the excision site to control the bleeding. Following the surgery, the mass was submitted to the pathology department for review. On histological examination, the tumor showed clear cells with organoid patterns, which is consistent with PEComa (Fig. 2A). Immunohistochemistry of the tumor cells was positive for HMB-45 (Fig. 2B) and TFE3, and negative for cytokeratin, HNF1-B, SOX10, Melan A, and S-100 protein.
One month after the vaginoscopic resection, pelvic magnetic resonance imaging was performed and showed no residual mass without any evidence of lymph node metastasis. Repeat pelvic pelvic magnetic resonance imaging performed 1 year later also showed normal findings.
PEComas are very rare tumors that can occur in various sites, and have a non-uniform description. Their natural history and behavior remain poorly understood. They are usually benign but can present with some malignant features [3]. In the majority of reported cases, these tumors behaved in a benign fashion and remained confined to their primary sites of origin [1,2,3,4,5]. However, there have been a few cases of local recurrence and a single reported case of distant metastasis, years after resection of the primary tumor [8,9]. Therefore, they are considered tumors with unknown malignant potential, and there are no proven demographic or morphological criteria predicting aggressiveness or malignant transformation in PEComas [10].
Since these lesions may exhibit an extensive range of biological behavior, there are no well-established treatment guidelines for patients with PEComa [6]. Metastases of PEComa have been successfully managed by resection alone [8]. The role of adjuvant therapy remains unclear. However, if there are some high-risk features such as lymph node metastases, tumor necrosis and a large tumor size, adjuvant chemotherapy can be considered. Patients with PEComa should also be closely monitored for recurrence for long periods of time.
Our case is special because of both the site of the tumor and the age of the patient. Although PEComas have been described in a variety of locations such as the ligamentum teres/falciform ligament, the palate, and the orbit, there have been only a few cases of PEComas arising from the vaginal wall [11,12,13]. In addition, there have only been a few documented cases of PEComas in young children. Among them, our case involves the youngest patient reported to have a tumor arising from the vagina.
The vaginal PEComa in our case was treated with surgery alone because of its small size and benign appearance. Regular follow-up was recommended to this patient because of the unknown malignant potential and recurrence rate. So far no evidence of recurrence has been detected, and we believe that this is due to the early surgical intervention with complete resection. This case shows that early detection and treatment of PEComa is important because of its unknown malignant potential. Since the incidence of vaginal PEComas is very rare, and this is only the third reported case in children, additional case studies are warranted to better understanding of this disease.
Figures and Tables
References
1. Bonetti F, Pea M, Martignoni G, Zamboni G. PEC and sugar. Am J Surg Pathol. 1992; 16:307–308.
2. Zamboni G, Pea M, Martignoni G, Zancanaro C, Faccioli G, Gilioli E, et al. Clear cell "sugar" tumor of the pancreas. A novel member of the family of lesions characterized by the presence of perivascular epithelioid cells. Am J Surg Pathol. 1996; 20:722–730.
3. Silva EG, Deavers MT, Bodurka DC, Malpica A. Uterine epithelioid leiomyosarcomas with clear cells: reactivity with HMB-45 and the concept of PEComa. Am J Surg Pathol. 2004; 28:244–249.
4. Tazelaar HD, Batts KP, Srigley JR. Primary extrapulmonary sugar tumor (PEST): a report of four cases. Mod Pathol. 2001; 14:615–622.
5. Cheung TT, Trendell-Smith N, Poon RT. Primary perivascular epithelioid cell tumour (PEComa) of the liver. BMJ Case Rep. 2013; 2013.
6. Folpe AL, Mentzel T, Lehr HA, Fisher C, Balzer BL, Weiss SW. Perivascular epithelioid cell neoplasms of soft tissue and gynecologic origin: a clinicopathologic study of 26 cases and review of the literature. Am J Surg Pathol. 2005; 29:1558–1575.
7. Ong LY, Hwang WS, Wong A, Chan MY, Chui CH. Perivascular epithelioid cell tumour of the vagina in an 8 year old girl. J Pediatr Surg. 2007; 42:564–566.
8. Kalyanasundaram K, Parameswaran A, Mani R. Perivascular epithelioid tumor of urinary bladder and vagina. Ann Diagn Pathol. 2005; 9:275–278.
9. Ye HY, Chen JG, Luo DL, Jiang ZM, Chen ZH. Perivascular epithelioid cell tumor (PEComa) of gynecologic origin: a clinicopathological study of three cases. Eur J Gynaecol Oncol. 2012; 33:105–108.
10. Fadare O, Parkash V, Yilmaz Y, Mariappan MR, Ma L, Hileeto D, et al. Perivascular epithelioid cell tumor (PEComa) of the uterine cervix associated with intraabdominal "PEComatosis": a clinicopathological study with comparative genomic hybridization analysis. World J Surg Oncol. 2004; 2:35.
11. Folpe AL, Goodman ZD, Ishak KG, Paulino AF, Taboada EM, Meehan SA, et al. Clear cell myomelanocytic tumor of the falciform ligament/ligamentum teres: a novel member of the perivascular epithelioid clear cell family of tumors with a predilection for children and young adults. Am J Surg Pathol. 2000; 24:1239–1246.
12. Iyengar P, Deangelis DD, Greenberg M, Taylor G. Perivascular epithelioid cell tumor of the orbit: a case report and review of the literature. Pediatr Dev Pathol. 2005; 8:98–104.
13. Koutlas IG, Pambuccian SE, Jessurun J, Manivel JC, Gopalakrishnan R. Perivascular epithelioid cell tumor of the oral mucosa. Arch Pathol Lab Med. 2005; 129:690–693.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download