Abstract
Sclerosing stromal tumor is a rare ovarian tumor, occurring in young adults in the second and third decade of life. We report clinical and histopathological features of three cases of sclerosing stromal tumor of the ovary with a review of literature. The tumor has distinct histological features and is easily recognizable when a high index of suspicion is maintained in young patients presenting with an ovarian mass. These tumors are benign and can be treated successfully by enucleation or unilateral ovariotomy.
Ovarian sex cord tumors are relatively infrequent neoplasms that account for approximately 8% of all primary ovarian neoplasms [1]. Sclerosing tumors account for 2% to 6% of ovarian tumors originating from stroma of ovary [2]. Sclerosing stromal tumors were first described by Chalvardjian and Scully in 1973 [3] and less than 100 cases have been described in literature [4].
More than 80% of sclerosing stromal tumors have been observed in young adults in the second and third decades of life [5]. Sclerosing stromal tumors are usually hormonally inactive. If hormonally active, they are usually androgenic and occur most frequently during pregnancy. Menstrual irregularity and pelvic pain are the most frequent complaints during presentation [6].
We describe clinical findings and histopathological features of three cases of sclerosing stromal tumor of the ovary which we recently encountered at the Mahatma Gandhi Institute of Medical Sciences, Sevagram.
A 15-year-old girl presented with pelvic pain and menstrual irregularity of two years duration. Physical examination revealed a large palpable abdominopelvic mass. The patient had a history of sickle cell trait. Ultrasonographic examination revealed a right ovarian mass of 7×6×4 cm of variegated consistency with an irregular surface. On exploratory laparotomy, an irregular mass which was 8×5×3 cm in size was found. It was attached to the right ovary with single twist at its pedicle. The external surface was congested. The cut surface of the ovarian mass revealed solid, cystic and hemorrhagic areas. The left ovary was unremarkable.
A 24-year-old woman presented with complaints of continuous vaginal bleeding since two months. She had complaints of menorrhagia since the last two years. On clinical examination, a large mass was palpable in the lower abdomen. Ultrasonography revealed a well-defined solid-cystic echogenic mass of size 5.3×4×3.9 cm in the left ovary. All other laboratory tests and hormonal assays were normal.
The patient underwent a left salpingo-oopherectomy. Gross examination of the specimen received in histopathology showed an encapsulated mass measuring 6×4×4 cm which was attached to the left ovary. It had a smooth external surface. On cut section the mass was solid, firm in consistency with multiple degenerated cystic foci.
A 25-year-old unmarried female presented with distension of abdomen of 5 days duration. She did not have any menstrual complaints. Physical examination and radiologic findings revealed an abdominopelvic mass. At laparoscopy a yellow lobulated cystic mass was found attached to left ovary. The right ovary was unremarkable. The specimen of left ovarian mass measuring 9×8×4 cm was received in the histopathology section. It was well circumscribed, round to oval with a smooth outer surface. The cut section was pale yellow with solid cystic areas.
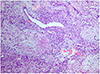
The microscopic appearance of all three cases was similar. Sections from the ovarian mass showed a pseudolobular pattern in which cellular areas were separated by oedematous collagenous hypocellular areas (Fig. 1). The cellular areas were composed of spindle shaped and round to oval cells with vesicular nuclei and a moderate amount of eosinophilic cytoplasm. Cellular areas revealed a thin-walled capillary network giving 'hemangiopericytoma-like' pattern (Fig. 2). In some cells the nuclei were eccentrically placed giving signet ring appearance. Nuclear atypia and mitosis were not seen.
Ovarian neoplasms are rare in adolescents and they are mainly tumors of germ cell origin [6]. Sex cord-stromal tumors of ovary include granulosa cell tumors, fibrothecomas, Sertoli-Leydig cell tumors, steroid cell tumors and sclerosing stromal tumors [7].
Sclerosing stromal tumors account for only 6% of sex cordstromal tumors and have a tendency to occur in younger women (mean age around 30 years) [8]. In our study, all the three patients were aged less than 30 years. The most common clinical symptoms in patients with sclerosing stromal tumors are menstrual irregularities, pelvic pain and non-specific symptoms related to presence of a pelvic mass [5].
Hormonal activity has been reported in a few documented cases. Lam and Geittmann [9] proved that sclerosing stromal tumors synthesized dehydroepiandrosterone. Damajanov et al. [10] have documented that elevated levels of both estrogenic and androgenic hormones were responsible for menstrual irregularity, amenorrhoea and infertility. However none of our patients had any evidence of hormonal disturbances.
The etiology of sclerosing stromal tumors is unknown. Ismail et al. [11] suggested that endocrine milieu might be responsible for the morphology of sclerosing stromal tumors and they may develop from pre-existing ovarian fibromas. On the basis of ultrastructural features, sclerosing stromal tumors were thought to arise from the pluripotent immature stromal cells of the ovarian cortex [9]. However sclerosing stromal tumors have now been proposed to be derived from a population of muscle-specific actin-positive elements from the theca externa, namely, the perifollicular myoid stromal cells [9]. Tiltman and Haffajee [12] suggested that sclerosing stromal tumors and thecomas are probably closely related entities as they share some morphologic features and antigenic determinants like smooth muscle actin and vimentin.
The gross appearance of sclerosing stromal tumors of ovary ranges from small solid masses to large multicystic masses. Microscopically the tumor shows a characteristic pattern with pseudolobulation of the cellular areas separated by hypocellular areas of densely collagenous or edematous tissue. The cellular areas contain prominent thin walled vessels with varying degree of sclerosis admixed with both spindled and lipid containing round to oval cells. The vascular, sclerotic and edematous stromal changes are constant features of these tumors and are related to the local elaboration of some factors like vascular permeability factor and vascular endothelial growth factor [13]. Immunohistochemically, the cells of sclerosing stromal tumor are positive for vimentin, inhibin, smooth muscle actin, α inhibin and CD199. They are negative for S-100 and epithelial markers [4].
Depending on which component is most prominent in the tumor, other entities have to be considered in the differential diagnosis [14]. The important differential diagnoses include other sex cord-stromal tumors including fibroma, thecoma, lipid cell tumor, vascular tumors, malignant tumors such as Krukenberg's tumor, and non-neoplastic conditions such as massive odema of ovary.
Thecomas and fibromas usually occur in the fifth to sixth decades of life. Thecomas are typically estrogenic tumors whereas fibromas are non-functioning tumors which may have diffuse oedema [15]. Calretinin, inhibin, CD34, and α-glutathione S-transferase (α-GST) positivity has been reported to be useful in differentiating sclerosing stromal tumors from other sex cord-stromal tumors. Thecomas show diffuse staining with α-GST, while fibromas do not take up this stain. In sclerosing stromal tumors α-GST positivity is seen in scattered cells. CD34 positivity of sclerosing stromal tumors clearly distinguishes it from thecoma and fibroma. Vascular tumors are included in differential diagnosis due to prominent vascularity, but inhibin positivity suggests the diagnosis of sclerosing stromal tumor [9,12]. Sometimes massive edema of ovary may be confused with sclerosing stromal tumors. But preserved ovarian tissue within the edematous stroma and absence of heterogeneity favors the diagnosis of massive ovarian edema. Sclerosing stromal tumors can be differentiated from Krukenberg's tumors as the latter are mostly bilateral, occur in the sixth and seventh decades of life and lack of pseudolobular pattern. Also signet-ring cells of Krukenberg's tumors contain mucin rather than lipid and they exhibit mitotic activity and nuclear atypia [12].
The definite diagnosis of sclerosing stromal tumor is made only by pathologic evaluation, but a diagnosis is possible intraoperatively via frozen section analysis by examining the background of pseudolobular pattern, heterogeneity of the cellular areas and densely hyalinized or markedly edematous stroma.
Sclerosing stromal tumor is an extremely rare and distinctive sex cord-stromal tumor, occurring predominantly in the second and third decades of life. Due to the rarity of this neoplasm it is not always possible to predict the presence of this tumor preoperatively on the basis of clinical and radiological findings. The possibility of sclerosing stromal tumor should always be kept in young patients with ovarian mass, as these benign and can be treated successfully by enucleation or unilateral ovariotomy.
Figures and Tables
References
1. Young RH. Sex cord-stromal tumors of the ovary and testis: their similarities and differences with consideration of selected problems. Mod Pathol. 2005; 18:Suppl 2. S81–S98.
2. Peng HH, Chang TC, Hsueh S. Sclerosing stromal tumor of ovary. Chang Gung Med J. 2003; 26:444–448.
3. Chalvardjian A, Scully RE. Sclerosing stromal tumors of the ovary. Cancer. 1973; 31:664–670.
4. Chang W, Oiseth SJ, Orentlicher R, Agarwal G, Yahr LJ, Cayten CG. Bilateral sclerosing stromal tumor of the ovaries in a premenarchal girl. Gynecol Oncol. 2006; 101:342–345.
5. Kaygusuz EI, Cesur S, Cetiner H, Yavuz H, Koc N. Sclerosing stromal tumour in young women: clinicopathologic and immunohistochemical spectrum. J Clin Diagn Res. 2013; 7:1932–1935.
6. Fox H, Wells M. Haines and Taylor obstetrical and gynaecological pathology. 5th ed. New York: Churchill Livingstone;2003.
7. Chang CM, Shin SL. Sclerosing stromal tumor of the ovary in a three three-year-old girl. J Radiol Sci. 2011; 36:59–62.
8. Stylianidou A, Varras M, Akrivis C, Fylaktidou A, Stefanaki S, Antoniou N. Sclerosing stromal tumor of the ovary: a case report and review of the literature. Eur J Gynaecol Oncol. 2001; 22:300–304.
9. Lam RM, Geittmann P. Sclerosing stromal tumor of the ovary: a light, electron microscopic and enzyme histochemical study. Int J Gynecol Pathol. 1988; 7:280–290.
10. Damajanov I, Drobnjak P, Grizelj V, Longhino N. Sclerosing stromal tumor of the ovary: a hormonal and ultrastructural analysis. Obstet Gynecol. 1975; 45:675–679.
11. Ismail SM, Walker SM. Bilateral virilizing sclerosing stromal tumours of the ovary in a pregnant woman with Gorlin's syndrome: implications for pathogenesis of ovarian stromal neoplasms. Histopathology. 1990; 17:159–163.
12. Tiltman AJ, Haffajee Z. Sclerosing stromal tumors, thecomas, and fibromas of the ovary: an immunohistochemical profile. Int J Gynecol Pathol. 1999; 18:254–258.
13. Kawauchi S, Tsuji T, Kaku T, Kamura T, Nakano H, Tsuneyoshi M. Sclerosing stromal tumor of the ovary: a clinicopathologic, immunohistochemical, ultrastructural, and cytogenetic analysis with special reference to its vasculature. Am J Surg Pathol. 1998; 22:83–92.
14. Suit PF, Hart WR. Sclerosing stromal tumor of the ovary: an ultrastructural study and review of the literature to evaluate hormonal function. Cleve Clin J Med. 1988; 55:189–194.
15. Akbulut M, Colakoglu N, Soysal ME, Duznca SE. Sclerosing stromal tumor of the ovary: report of a case and review of the literature. Aegean Pathol J. 2004; 1:84–89.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download