Abstract
Objective
To investigate the incidence of actinomyces-like organisms in routine cervical smears of Korean women and to evaluate its association with the development of pelvic inflammatory disease (PID) in these women.
Methods
The results of cervical smears between 2011 and 2012 at a single university hospital were searched. If positive for actinomyces-like organisms, the medical record of the patient was searched and development of PID was followed. If the data were not available in the medical record, the patient was contacted by telephone.
Results
The incidence of actinomyces-like organisms in cervical smears was 0.26% (52/20,390). Forty-two women (80.8%) were intrauterine device (IUD) users: the copper-IUD in 25 women and the levonorgestrel-releasing intrauterine system in 13 women (type unknown in 4 women). The majority (71.4%, 30/42) of the IUD users maintained the IUD. Prophylactic antibiotics were prescribed to 12 women. Two continuous IUD users were later diagnosed with PID, but these cases were not pelvic actinomycosis.
Actinomyces are anaerobic gram-positive non-spore forming filamentous bacteria that are present in the normal flora of the mouth, the pharynx and probably the lower ileum and cecum [1]. However, if the integrity of the mucosal membrane is broken, human infection may occur and can cause a fatal disease in some cases.
Human actinomycosis infection was first described in Israel in 1878. Among human actinomycosis, pelvic actinomycosis is a very rare disease, and known to be associated with intrauterine devices (IUDs) and ascending infection from the uterus. Actinomycosis is sensitive to penicillin and can be cured effectively. However, an explorative laparotomy may be required in some cases because it is not easily diagnosed and difficult to distinguish from adnexal malignancy.
Actinomyces-like organisms rarely appear on routine Papanicolaou-stained cervical smears. However, it is reported that the rate of positive actinomyces-like organisms appearing on cervical smears is about 7% in women with an IUD and the incidence varies according to the type and duration of IUD used [2]. The positive finding of actinomyces-like organisms on the cervical smear is neither diagnostic nor a predictor of pelvic actinomycosis. Thus, asymptomatic patients are recommended to be managed expectantly [3,4,5]. However, some clinicians remove the IUD or prescribe antibiotics to treat the incidentally found actinomyces-like organisms.
We herein investigated the incidence of actinomyces-like organisms found in the cervical smears of Korean women, and their association with the presence of an IUD, the clinician's management options, and the development of pelvic inflammatory disease (PID).
The results of 20,390 cervical smears, performed at the Seoul National University Bundang Hospital between 2011 and 2012, were searched (7,442 smears in 2011 and 12,948 smears in 2012). If actinomyces-like organisms were found on the cervical smears, the medical record of the patient was searched and age, parity, other co-infection of candidiasis or bacterial vaginosis, presence of an IUD, duration of the IUD use, subsequent clinician's management options, symptoms or signs suggestive of PID such as abdominal pain, fever and vaginal discharge, and overt development of PID were investigated. If the data were not available in the medical records, the patient was contacted by telephone. The chart review and telephone contact were approved by the Institutional Review Board of the Seoul National University Bundang Hospital.
The cervical smears were performed using liquid-based cytology (Surepath; TriPath Imaging Inc., Burlington, NC, USA) and stained with the Papanicolaou method. The smears were read by more than 5 cytologists in the Department of Pathology at the Seoul National University Bundang Hospital, each with over 5 years of experience and without knowing the patients' medical history or IUD insertion status. When there were basophilic conglomerates with a dense central part surrounded by intertwined filament-type formations in the Papanicolaou smear, it is diagnosed as containing actinomyces-like organisms.
Statistical analyses were performed using SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA). The mean was compared by the Student's t-test and proportion by the chi square test. The result was considered significant when the P-value was less than 0.05.
Among the 20,390 cervical smears examined during two years, actinomyces-like organisms were found in 52 specimens (0.26%). The age of these 52 women ranged from 29 to 77 years (mean, 46.7 years) and the parity ranged from zero to six. Forty-two women (80.8%) were IUD users: the copper-IUD (Multiload Cu 375; Merck & Co., Rahway, NJ, USA) in 25 women and the levonorgestrel-releasing intrauterine system (Mirena, Bayer HealthCare, Leverkusen, Germany) in 13 women (type unknown in four women). Among the IUD users, 65.8% of the women used the IUD for more than 60 months and 18% used it for less than 36 months. The duration of IUD usage ranged from 15 months to over 5 years.
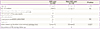
According to the IUD use status, the subsequent management options and the occurrence of PID are listed in Table 1. The majority of the IUD users (71.4%, 30/42) chose to keep the IUD, but eight women chose to remove it after confirmation of actinomyces-like organisms on cervical cytology. Among these eight women, there were two cases of hysteroscopic IUD removal due to an invisible IUD thread. No culture was performed in the women who underwent an IUD removal because there were no symptoms related to PID. Two cases of concomitant candidiasis and one case of concomitant bacterial vaginosis were identified among the 52 patients with positive actinomyces-like organisms on the smear. Prophylactic antibiotics were prescribed to ten IUD users and two non-IUD users (P>0.05).
We identified two women who were diagnosed with PID later. Both of these women were IUD users and maintained the IUD despite a positive actinomyces-like organism on the cervical smear. One woman was a copper-IUD user for 5 years and maintained the IUD without prophylactic antibiotics; she underwent surgical treatment in our hospital to treat a right tuboovarian abscess and it was confirmed that the pelvic infection was not actinomycosis. Another woman was a copper-IUD user for 2 years and maintained the IUD with prophylactic antibiotics; she underwent surgical treatment due to the PID at another hospital and it was also confirmed that the PID was not pelvic actinomycosis (by personally contacting the hospital).
The main findings of our study are as follows: 1) the incidence of positive actinomyces-like organisms on a cervical smear was 0.26%, 2) the majority of the women (81.1%) with positive results were IUD users, and 3) two IUD users were diagnosed with PID later but it was not pelvic actinomycosis.
The incidence of positive actinomyces-like organisms in this study is very similar to a previous report in which the incidence of positive actinomyces-like organisms was approximately 0.27% [6]. We could not estimate the incidence of positive actinomyces-like organisms on the cervical smear in IUD users; however, many studies have reported that the incidence is markedly higher. Bonacho et al. [7] reported that 5.9% of IUD users showed positive actinomyces-like organisms on the cervical smear, and Chatwani and Amin-Hanjani [8] reported 6.7% positivity in copper-IUD users and 13.3% to 22.2% in plastic IUD users. The incidence of actinomyces-like organisms was reported to be much lower in levonorgesterol-releasing IUD users than copper-IUD users [9].
Currently, there are no identified risk factors of developing pelvic actinomycotic abscesses, but IUD type, duration, and sexual behavior tend to be related to actinomycosis [10]. Matsuda et al. [11] reported that the detection rate of actinomyces-like organisms on cervical and endometrial cytology in pelvic actinomycotic abscesses was 77.7%. However, the occurrence of pelvic actinomycosis is reported to be a much rarer event (<0.001%) [3]. The relationship between positive actinomyces-like organisms on cervical smears and the development of actual pelvic actinomycosis is not yet specified. Taken together with our results, treating incidentally-found actinomyces-like organisms in asymptomatic patients appears to be unnecessary [12].
IUD users have a higher chance of developing bacterial vaginosis compared to the general population [13]. The favorable environment of anaerobes might be established inside the vagina, facilitating the growth of actinomyces. In some cases, PID or pelvic abscesses related to actinomycosis are observed in women who have been using an IUD for a long time [8]. But as commensal organisms in the female genital tract, actinomyces israelii cannot be a predictor or diagnostic factor for actinomycosis, only because of the identification of actinomyces in cervical smear or immunofluorescence or culture [2]. Indeed, up to 7% of women who are using an IUD obtain actinomyces-like organism positive cervical smears. However, this test has a low sensitivity, specificity and positive predictive value, thus it has no clinical significance, and it is recommended that special treatment is not required when symptoms are not detected [3].
IUD removal is still a controversial issue and has been suggested to be unnecessary [3]. On the other hand, other researchers favor removal based on the fact that though the frequency of pelvic actinomycosis is extremely low, if it occurs, it can be fatal. Since it is usually converted to negative cervical cytology after 4 to 6 weeks [14], IUD management has been suggested as follows: 1) reinsertion should be implemented during an interval of 4 to 6 weeks, 2) exchange should be performed during an interval of 3 to 5 days rather than an immediate routine IUD exchange [15].
In 2006, Kalaichelvan et al. [5] compared the treatment modalities for actinomyces-positive asymptomatic IUD users. They compared treatment outcomes between four groups: no treatment, penicillin V 500 mg three times a day for 2 weeks, doxycycline 100 mg twice a day for 2 weeks, and metronidazole 400 mg three times a day for 2 weeks. In that study, they suggested that antibiotic treatment was not necessary for actinomyces-positive asymptomatic women because there were no significant differences in the treatment outcomes between the four groups. Similarly, in our series, clinical actinomycosis did not develop whether prophylactic antibiotics were taken or not.
In conclusion, we investigated for the first time the incidence of actinomyces-like organisms in routine cervical smears and its association with IUD users in Korean women. Considering the very rare development of pelvic actinomycosis, incidentally found actinomyces-like organisms could be managed expectantly.
Figures and Tables
References
1. Evans DT. Actinomyces israelii in the female genital tract: a review. Genitourin Med. 1993; 69:54–59.
2. Mali B, Joshi JV, Wagle U, Hazari K, Shah R, Chadha U, et al. Actinomyces in cervical smears of women using intrauterine contraceptive devices. Acta Cytol. 1986; 30:367–371.
3. Lippes J. Pelvic actinomycosis: a review and preliminary look at prevalence. Am J Obstet Gynecol. 1999; 180(2 Pt 1):265–269.
4. Westhoff C. IUDs and colonization or infection with Actinomyces. Contraception. 2007; 75:6 Suppl. S48–S50.
5. Kalaichelvan V, Maw AA, Singh K. Actinomyces in cervical smears of women using the intrauterine device in Singapore. Contraception. 2006; 73:352–355.
6. Haltas H, Bayrak R, Yenidunya S. To determine of the prevalence of Bacterial Vaginosis, Candida sp, mixed infections (Bacterial Vaginosis + Candida sp), Trichomonas Vaginalis, Actinomyces sp in Turkish women from Ankara, Turkey. Ginekol Pol. 2012; 83:744–748.
7. Bonacho I, Pita S, Gomez-Besteiro MI. Eight years with the same IUD. Contraception. 1999; 59:233–236.
8. Chatwani A, Amin-Hanjani S. Incidence of actinomycosis associated with intrauterine devices. J Reprod Med. 1994; 39:585–587.
9. Merki-Feld GS, Lebeda E, Hogg B, Keller PJ. The incidence of actinomyces-like organisms in Papanicolaoustained smears of copper- and levonorgestrel-releasing intrauterine devices. Contraception. 2000; 61:365–368.
10. Pérez-López FR, Tobajas JJ, Chedraui P. Female pelvic actinomycosis and intrauterine contraceptive devices. Open Access J Contracept. 2010; 1:35–38.
11. Matsuda K, Nakajima H, Khan KN, Tanigawa T, Hamaguchi D, Kitajima M, et al. Preoperative diagnosis of pelvic actinomycosis by clinical cytology. Int J Womens Health. 2012; 4:527–533.
12. Singh MM, Ingham HR, Wadehra V, Morris K. Endometrial culture in IUD users with actinomycosis-like organisms (ALOs) on cervical smears. Br J Fam Plann. 1989; 15:3–6.
13. Barbone F, Austin H, Louv WC, Alexander WJ. A follow-up study of methods of contraception, sexual activity, and rates of trichomoniasis, candidiasis, and bacterial vaginosis. Am J Obstet Gynecol. 1990; 163:510–514.
14. Fiorino AS. Intrauterine contraceptive device-associated actinomycotic abscess and Actinomyces detection on cervical smear. Obstet Gynecol. 1996; 87:142–149.
15. Merki-Feld GS, Rosselli M, Imthurn B. Comparison of two procedures for routine IUD exchange in women with positive Pap smears for actinomyces-like organisms. Contraception. 2008; 77:177–180.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download