Abstract
Objective
The purpose of this study was to compare clinical and surgical outcomes between laparo-endoscopic single-site (LESS) surgery and traditional multiport laparoscopic (TML) surgery for treatment of adnexal tumors.
Methods
Medical records were reviewed for patients undergoing surgery for benign adnexal tumors between January 2008 and April 2012 at our institution. All procedures were performed by the same surgeon. Clinical and surgical outcomes for patients undergoing LESS surgery using Glove port were compared with those patients undergoing TML surgery.
Results
A review of 129 patient cases undergoing LESS surgery using Glove port and 100 patient cases undergoing TML surgery revealed no significant differences in the baseline characteristics of the two groups. The median operative time was shorter in the LESS group using Glove port at 44 minutes (range, 19-126 minutes) than the TML group at 49 minutes (range, 20-196 minutes) (P=0.0007). There were no significant differences between in the duration of postoperative hospital stay, change in hemoglobin levels, pain score or the rate of complications between the LESS and TML groups.
The last four decades have witnessed a surgical shift from laparotomy to laparoscopy in gynecologic surgery [1]. Minimally invasive surgery has resulted in reduced morbidity rate, shorter hospital stays, and more rapid recovery, as reported in various studies. Technical innovations in instrumentation have not only affected simple procedures such as ectopic pregnancy management, but also highly complicated operations, including radical cancer [2,3,4].
Initially, laparoscopy in gynecologic surgery was performed with a single incision. However, due to technical limitations and increasingly complex surgeries, the use of additional incisions has become necessary. Recently, efforts have been made to reduce the number of laparoscopic ports the ultimate goal being the absence of any visible scar [5]. Rapid advances in the development of laparoscopic instruments have allowed the advancement of even less invasive procedures. Laparo-endoscopic single-site (LESS) surgery involves the use of one small skin incision to complete laparoscopic surgical procedures, which would have previously required multiple incisions [1].
To facilitate LESS surgery, the development of a port system, which allows several instruments to enter into the abdominal cavity in a single incision, was crucial. Glove port (Nelis, Seoul, Korea) is a newly developed system consisting of three or four channels within a single port. A single 20-mm to 25-mm incision is needed to introduce the port system into the abdominal cavity. The elastic caps in the channels of the port system allow the use of instruments from 3 to 15 mm in diameter.
Numerous studies have demonstrated the feasibility of LESS surgery using various port systems compared to that of traditional multiport laparoscopic (TML) surgery [6,7,8,9,10,11,12]. However, these studies were limited by relatively small patient populations, and few studies have evaluated the Glove port system. Therefore, the aim of this study was to compare clinical and surgical outcomes between LESS surgery using Glove port system and TML surgery for adnexal tumors in a larger patient population.
Medical records of patients undergoing surgery for benign adnexal tumors at our institution were reviewed. TML surgery was the procedure of choice between January 2008 and December 2009. From May 2010 to April 2012, surgeries were performed using the LESS surgery using the Glove port method. All procedures were performed by a single surgeon at the Department of Obstetrics and Gynecology, Severance Hospital, Yonsei University College of Medicine in Seoul, Korea. Glove port was adopted to LESS surgery in beginning of 2010 for some benign adnexal tumor surgeries. From May 2010 to April 2012, we had performed LESS surgery with Glove port system for every benign adnexal tumor surgery. Age, body mass index (mg/kg2), and prior history of abdominal surgery were reviewed. Moreover, perioperative data, bilaterality of adnexal lesions, presence of pelvic adhesions, operative time, and types of procedures performed were analyzed. The presence of pelvic adhesions was assessed by the surgeon at the time of the procedure. Operative time was defined as the interval between the initial incision to closure. The lengths of hospital stay, preoperative and postoperative hemoglobin levels, postoperative pain scores, and postoperative complication rates were also collected. Hemoglobin levels were measured sequentially for each patient preoperatively, and one and three days postoperatively. Pain was assessed in all patients using a validated visual analogue pain scale, scored from 0-10 (with "0" representing "no pain" and "10" representing "agonizing pain") by a physician. Postoperative complications were defined as any surgery-related symptoms that patients complained of 4 weeks postoperatively. Final pathologic diagnoses were also compared.
All operations, including TML surgery and LESS surgery, were performed by one surgeon. In TML surgery, a 10-mm vertical intraumbilical incision was made, and a 10-mm trocar was inserted bluntly. After creating a CO2 pneumoperitoneum, a rigid 30°, 10-mm laparoscope was introduced into the abdomen through the trocar. Additional ancillary 5-mm trocars were placed at McBurney's point, the counter-McBurney point, and 5 cm above the counter-McBurney point for insertion of conventional laparoscopic instruments. Organs were removed with the Endopouch retriever (Ethicon Endo-Surgery, Johnson & Johnson Korea, Seoul, Korea) through the umbilicus.
In LESS surgery using Glove port system, a single 20- to 25-mm sized vertical incision was made in the navel area for Glove port system (Fig. 1). Glove port utilizes a manual retractor used in laparoscopy, which can be adjusted to the thickness of the port system. Three to four channels with the elastic gel-caps in the Glove port permit the introduction of instruments 3 to 15 mm in diameter into the abdominal cavity without CO2 gas leakage. Additional two valves allow CO2 gas in and out separately. A cord attached to the inner ring of the port system allows quick and easy removal of the Glove port. After the CO2 penumoperitoneum is created, a rigid 30°, 5-mm laparoscope was introduced through one of the channels. Simultaneously, conventional laparoscopic instruments were introduced through the remaining channels, as needed for the surgery.
Data were analyzed using parametric and nonparametric statistics, with the SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were used for patient characteristic data, and the results are summarized as means and standard deviations. Continuous variables were examined for a normal distribution (Kolmogorov-Smirnov test) before adopting parametric statistics. Generally, for all analyses P<0.05 was considered significant.
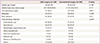
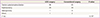
A total of 229 patients were included in this study; 129 in the LESS surgery group and 100 in the TML surgery group. None of the patients required laparotomy, and in the LESS group, no patients required an additional port during the operation. The most common surgical indications, based on pathologic diagnoses, were endometriotic cyst and dermoid cyst in both groups respectively (Table 1). Patient characteristics, including age, BMI, prior abdominal surgery, bilaterality of lesions, pelvic adhesions, and final pathological diagnoses, were not significantly different between the two groups (Table 1). The types of procedures performed were not significantly different between the two groups (Table 2).
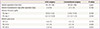
Surgical outcomes are listed in Table 3. The median operative time was shorter in the LESS group at 44 minutes (range, 19-26 minutes) than in the TML group at 49 minutes (range, 20-196 minutes). This difference was statistically significant (P=0.0007). The median postoperative hospital stay was approximately 2 days for both groups. The median hemoglobin level changes were nearly the same in both groups (postoperative day 1, 1.9 g/dL [range, 0.1-5.0 g/dL] vs. 1.9 g/dL [range, 0.1-5.4 g/dL] P=0.703; postoperative day 3, 2.2 g/dL [range, -0.1-6.9 g/dL] vs. 2.1 g/dL [range, -0.1-3.5 g/dL], P=0.292). There were no significant differences postoperative pain score between the two groups.
Postoperative complications in the LESS group included five patients with difficulty voiding, eight patients with bowel distention and irritation, four patients with wound dehiscence and one patient with an abdominal wall hematoma near the incision site. In the TML group, one patient complained of difficulty voiding, two patients complained of bowel distention, and two patients developed abdominal wall hematoma. The incidence of these postoperative complications was equally distributed in both groups as illustrated in Table 4.
In this study, LESS surgery showed comparable clinical and surgical outcomes to TML surgery. Additionally, operative time for the removal of adnexal tumors significantly reduced. Therefore, LESS surgery may be a preferred option for patients suspected to having benign adnexal tumors.
Rapid development of operative laparoscopy in the field of gynecologic surgery is evidence of the advantages of minimally invasive surgery. Since Shapiro and Adler first reported the use of the laparoscope for salpingectomy in 1973 [2], therapeutic laparoscopy in gynecology has evolved immensely. Many procedures previously performed as traditional abdominal and vaginal operations are currently readily performed under laparoscopic direction. Operative laparoscopy has the benefit of shorter hospital stays, lesser adhesion formation, lesser postoperative pain, and faster returns to normal activity [3,4].
More recently, efforts are being made to reduce the number of laparoscopic ports in minimally invasive surgery, and LESS surgery has been actively adopted in the surgical gynecology field with the development of various supplementary instruments. LESS surgery further enhances the cosmetic benefits of minimally invasive surgery while minimizing the potential morbidity associated with multiple incisions [13]. Preliminary advances in LESS as applied to urologic and gastrointestinal surgery demonstrated that the techniques were feasible [14,15]. This was accomplished by utilizing both advances in minimally invasive techniques and technological innovation, including use of the newest generation of port systems that allow several conventional laparoscopic instruments to be handled simultaneously through a single operating trocar [13,14,15]. In this study, we used Glove port with three-channel system for passage of instruments.
Beneficial surgical outcomes of LESS surgery over TML surgery have been suggested by several previous studies [6,7,8,9,10,11,12,16]. Outcomes, including operative times, length of hospital stay, and complication rates appear comparable. Improved cosmetic outcomes with less scarring, further reduction in postoperative pain, and reduction in incision-related morbidity were demonstrated. Kim et al. [7] and Yim et al. [8] noted lesser postoperative pain and reduced need for postoperative pain medications in the LESS group. In previous studies, in women undergoing laparotomy for pelvic masses, malignancy was seen in only 10% of women <39 years of age, and most of these tumors had a low malignancy potential [17]. In another report, the chance that a primary ovarian tumor is malignant in a patient <45 years of age was <1 in 15 [18]. Therefore, for women in their reproductive years, most adnexal masses are benign [19]. Thus, dealing with benign adnexal masses of women in reproductive ages, LESS surgery may be a less invasive option with comparable or superior surgical compared to TML surgery.
According to our study, LESS surgery showed comparable clinical and surgical outcomes to TML surgery and required shorter operative time than TML surgery. We did not compare the cosmetic outcome of postoperative scars in our study. Postoperative pain was comparable in both groups in our study. Postoperative complications were similar with the exception that 4 patients in the LESS group (3.1%) developed wound dehiscence, while no wound dehiscence was reported in the TML group. Several studies reporting wound complications after LESS surgery have mainly noted incisional hernia [20,21,22]. Kadar et al. [20] reported a 3.1% of incisional hernia at a 1.2-mm trocar site. In our study, no incisional hernias were observed in either group. However, more importantly we found out that less operative time was required in LESS group, which could be a core contributor to the general postoperative outcomes of the patients including low cardio-pulmonary complications due to general anesthesia.
Although comparable results were obtained with LESS and, in some cases, superior outcomes were obtained with LESS surgery; there remain obstacles to the widespread adoption of this technique, especially because of the longer duration of learning the surgery. Thus, the learning curve appears to be longer. However, Escobar et al. [23] has observed significant decreases in operative times after a surgeon has performed 10 to 15 LESS, and he suggested that a larger operative port shortened operative time by allowing easier removal of resected tumors. Moreover, less time is required by surgeons to close the single port used in LESS surgery. He additionally pointed out that those training in LESS techniques are usually already proficient in TML, as in our study, making the transition more easily. All of these factors may lead to shortening of the learning curve.
Several strengths of this study could be listed. Firstly, relatively large patient populations were recruited in both groups, compared to previous studies about LESS surgery. Glove port, a new port system that could facilitate LESS surgery more in Gynecology, has been introduced. Our study had also revealed that LESS surgery might require shorter operative time than TML surgery. However, this study had not narrowed down detailed contributors that make LESS surgery spends shorter operative time, which could be a limitation of this study.
In conclusion, LESS surgery has been rapidly evolving with developing supplementary instrumentations. Based on this study, LESS surgery showed comparable clinical and surgical outcomes to TML surgery, and even took shorter operation time in dealing with adnexal tumors. Therefore, LESS surgery might be a better option for younger patients who are usually suspected to have benign adnexal tumors. Future prospective trials are warranted to define the benefit of LESS surgery for adnexal tumor treatment.
References
1. Bradford LS, Boruta DM. Laparoendoscopic single-site surgery in gynecology: a review of the literature, tools, and techniques. Obstet Gynecol Surv. 2013; 68:295–304.
2. Shapiro HI, Adler DH. Excision of an ectopic pregnancy through the laparoscope. Am J Obstet Gynecol. 1973; 117:290–291.
3. Medeiros LR, Rosa DD, Bozzetti MC, Fachel JM, Furness S, Garry R, et al. Laparoscopy versus laparotomy for benign ovarian tumour. Cochrane Database Syst Rev. 2009; (2):CD004751.
4. Nieboer TE, Johnson N, Lethaby A, Tavender E, Curr E, Garry R, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev. 2009; (3):CD003677.
5. Escobar PF, Starks D, Fader AN, Catenacci M, Falcone T. Laparoendoscopic single-site and natural orifice surgery in gynecology. Fertil Steril. 2010; 94:2497–2502.
6. Lee YY, Kim TJ, Kim CJ, Park HS, Choi CH, Lee JW, et al. Single port access laparoscopic adnexal surgery versus conventional laparoscopic adnexal surgery: a comparison of peri-operative outcomes. Eur J Obstet Gynecol Reprod Biol. 2010; 151:181–184.
7. Kim TJ, Lee YY, Cha HH, Kim CJ, Choi CH, Lee JW, et al. Single-port-access laparoscopic-assisted vaginal hysterectomy versus conventional laparoscopic-assisted vaginal hysterectomy: a comparison of perioperative outcomes. Surg Endosc. 2010; 24:2248–2252.
8. Yim GW, Jung YW, Paek J, Lee SH, Kwon HY, Nam EJ, et al. Transumbilical single-port access versus conventional total laparoscopic hysterectomy: surgical outcomes. Am J Obstet Gynecol. 2010; 203:26.e1–26.e6.
9. Fagotti A, Rossitto C, Marocco F, Gallotta V, Bottoni C, Scambia G, et al. Perioperative outcomes of laparoendoscopic single-site surgery (LESS) versus conventional laparoscopy for adnexal disease: a case-control study. Surg Innov. 2011; 18:29–33.
10. Yoon BS, Park H, Seong SJ, Park CT, Jun HS, Kim IH. Single-port versus conventional laparoscopic salpingectomy in tubal pregnancy: a comparison of surgical outcomes. Eur J Obstet Gynecol Reprod Biol. 2011; 159:190–193.
11. Escobar PF, Frumovitz M, Soliman PT, Frasure HE, Fader AN, Schmeler KM, et al. Comparison of single-port laparoscopy, standard laparoscopy, and robotic surgery in patients with endometrial cancer. Ann Surg Oncol. 2012; 19:1583–1588.
12. Chen YJ, Wang PH, Ocampo EJ, Twu NF, Yen MS, Chao KC. Single-port compared with conventional laparoscopic-assisted vaginal hysterectomy: a randomized controlled trial. Obstet Gynecol. 2011; 117:906–912.
13. Fader AN, Escobar PF. Laparoendoscopic single-site surgery (LESS) in gynecologic oncology: technique and initial report. Gynecol Oncol. 2009; 114:157–161.
14. Podolsky ER, Rottman SJ, Poblete H, King SA, Curcillo PG. Single port access (SPA) cholecystectomy: a completely transumbilical approach. J Laparoendosc Adv Surg Tech A. 2009; 19:219–222.
15. Canes D, Desai MM, Aron M, Haber GP, Goel RK, Stein RJ, et al. Transumbilical single-port surgery: evolution and current status. Eur Urol. 2008; 54:1020–1029.
16. Fagotti A, Bottoni C, Vizzielli G, Alletti SG, Scambia G, Marana E, et al. Postoperative pain after conventional laparoscopy and laparoendoscopic single site surgery (LESS) for benign adnexal disease: a randomized trial. Fertil Steril. 2011; 96:255–259.e2.
17. Hernandez E, Miyazawa K. The pelvic mass. Patients' ages and pathologic findings. J Reprod Med. 1988; 33:361–364.
18. Cannistra SA. Cancer of the ovary. N Engl J Med. 2004; 351:2519–2529.
19. Hillard PJ. Benign diseases of the female reproductive tract. In : Berek JS, editor. Berek & Novak's gynecology. 15th ed. Philadelphia: Lippincott Williams & Wilkins;2011. p. 410–412.
20. Kadar N, Reich H, Liu CY, Manko GF, Gimpelson R. Incisional hernias after major laparoscopic gynecologic procedures. Am J Obstet Gynecol. 1993; 168:1493–1495.
21. Podolsky ER, Curcillo PG 2nd. Single port access (SPA) surgery: a 24-month experience. J Gastrointest Surg. 2010; 14:759–767.
22. Worley MJ, Slomovitz BM, Ramirez PT. Complications of laparoscopy in benign and oncologic gynecological surgery. Rev Obstet Gynecol. 2009; 2:169–175.
23. Escobar PF, Starks DC, Fader AN, Barber M, Rojas-Espalliat L. Single-port risk-reducing salpingo-oophorectomy with and without hysterectomy: surgical outcomes and learning curve analysis. Gynecol Oncol. 2010; 119:43–47.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download