Abstract
Objective
To compare the pregnancy-related complications after laparoscopic and laparotomic uterine myomectomy.
Methods
A retrospective study of 415 women who received laparoscopic (n = 340) or laparotomic (n = 75) resection of uterine leiomyomas in one center. The mean follow-up period was 26.5 months in laparoscopic group and 23.9 months in laparotomic group.
Results
Fifty-four and 12 pregnancies occurred in laparoscopic and laparotomic myomectomy group, respectively. The major obstetric outcomes were similar between two groups. There was no ectopic pregnancy or preterm birth. There were two cases of obstetric complication in laparoscopic group only; one experienced neonatal death and postpartum hemorrhage due to placental abruption and the other underwent subtotal hysterectomy due to uterine dehiscence identified during Cesarean section.
About 10% of women with reproductive age have myomas. Some patients have symptoms related with myoma such as menorrhagia, abdominal pain, anemia and abdominal discomfort or have difficulty in conceive. A number of management options exist including observation, medical therapy, or surgical resection. Among them myomectomy has been known to be treatment of choice in women wish to conceive. According to previous studies, myoma may cause dysfunctional uterine contractility that may interfere with sperm migration and ovum transport and may disturb implantation due to focal endometrial vascular disturbance [1,2].
Laparoscopic myomectomy is currently one of common surgical procedure since Semm and colleague first described the procedure in late 1970s. A laparoscopic approach is more advantageous than laparotomy in postoperative pain, necessity of analgesia, recovery time, febrile morbidity and blood loss [3,4].
Some insists that laparoscopic myomectomy is more challenging procedure than laparotomic myomectomy because it requires advanced handling of instrument, labor of surgeon and has more risk of complication related to pregnancy such as uterine rupture during pregnancy or labor due to insufficient closure or healing defect of a uterine incision site. One study denoted that laparoscopic myomectomy scar is commonly thinner with more tension than laparotomic approach [4].
Despite of these concerns recently published studies indicate that laparoscopic myomectomy may be an appropriate alternative to laparotomic approach in well-selected patients [4]. Many studies reported the subsequent fertility and obstetrical outcome after laparoscopic myomectomy is comparable with the result of laparotomic myomectomy [5,6].
The feasibility and safety of laparoscopic myomectomy has been reported in a recent randomized controlled trial [7] and a meta-analysis of randomized controlled trials of laparoscopic versus open myomectomy showed no significant differences between the two groups in terms of pregnancy and even higher probability to conceive in laparoscopic procedures, possibly because of a reduced occurrence of postoperative adhesions [3].
A recent Korean study shows favorable pregnancy outcome following laparoscopic myomectomy. They included pregnancy cases only after laparoscopic myomectomy and there is no uterine rupture of 99 pregnancies [8].
Based on these considerations, we here reported the pregnancy outcomes following laparoscopic or laparotomic myomectomy in our institution.
In this retrospective study, four hundred fifteen women with 40 years old or less at the time of surgery were selected. We reviewed the medical records in patients who underwent laparoscopic (n = 340) or laparotomic myomectomy (n = 75) from January 2003 through December 2010 at the Seoul National University Bundang Hospital. The Institutional Review Board of our hospital approved the use of the patients' medical records.
Clinical characteristics, operative findings and subsequent obstetric outcomes were reviewed. Criteria for myomectomy included the presence of symptomatic myoma and presence of myoma without any revealed cause of recurrent abortion or infertility. In all cases, preoperative trans-vaginal or trans-abdominal ultrasonography was performed to evaluate number, size and location of myoma and to find possible associated pelvic diseases such as ovarian cyst and adnexal mass. If obstetric outcomes were absent in the medical records, we contacted the patient by telephone interview. In the pregnant cases, detailed obstetric outcomes such as normal term delivery without any complication, spontaneous abortion, ectopic pregnancy, preterm or term birth, mode of delivery, peripartum events, especially uterine rupture were investigated. In addition, operative time, and hemoglobin drop after operation was recorded.
Laparoscopic or laparotomic approach was dependent on surgeon's preference. Laparoscopic myomectomy was performed with standard techniques using two ports (suprapubic and counter Mcburney) or three ports (suprapubic, counter Mcburney and Mcburney). To decrease blood loss, diluted vasopressin was injected occasionally. For intramural and subserosal myoma, vertical incision was made and enucleation of myomas was carried out by traction of myoma using screw or claw forceps. Hemostasis during dissection was done using bipolar coagulation and one or two layered suture was done depending on the depth of incision. The procedures of laparotomic myomectomy were similar except using laparoscopic instruments.
Patient's age, marital status, parity, coexistence of other pelvic diseases, size and number of myomas, mean operation time, postoperative drop of hemoglobin level, and obstetric outcomes were analyzed using the Student's t-test or chi-square test, appropriately. Numeric data were shown as mean±standard deviation. P-value <0.05 was considered statically significant.
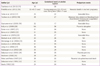
At the time of surgery, age of women and marital status was similar between two groups (Table 1). The proportion of parous women with at least one children was also similar (66.4% vs. 65.9%, P > 0.05). Between two groups, the proportion of women lost to follow-up or not responded was similar (13.8% vs. 8.0%, P > 0.05). The mean follow-up period was 26.5 months in laparoscopic group and 23.9 months in laparotomic group. At the time of investigation, 66 pregnancies were identified; 54 in laparoscopic group and 12 in laparotomic group. Overall pregnancy rate was similar between two groups (15.9% vs. 16.0%, P > 0.05). No women received assisted conception.
In subsequently pregnant women, age and marital status at the time of surgery was similar between two groups (Table 2). Co-operation of uterine adnexa was performed in nine women all from laparoscopic group. Size of the largest myoma enucleated and hemoglobin drop after operation was greater in the laparotomic group, however, number of myomas enucleated and mean operative time was similar between two groups.
As shown in Table 2, the principal obstetric outcomes were similar between two groups. There was no ectopic pregnancy or preterm birth. The majority of women were delivered by elective Cesarean section. In three women in laparoscopic group, vaginal delivery was initially tried but underwent emergency Cesarean section due to failure to progress. In one of these women, placental abruption and postpartum hemorrhage occurred and then uterine arterial embolization was performed. The mother was uneventful but the neonate was expired. Uterine dehiscence or rupture before or during delivery was not identified. However, in one woman in laparoscopic group, approximately 5 cm sized posterior uterine wall defect was identified during elective Cesarean section. The patient underwent subtotal hysterectomy because of uncontrolled uterine bleeding. The uterine muscle defect might be attributed to prior laparoscopic myomectomy because the defect site coincided with region of prior laparoscopic procedures.
The prevalence of myoma increases with age and is estimated 3% to 10% of women in reproductive age [9]. Uterine myomas have been reported in 27% of infertile women and 50% of unexplained infertile women who became pregnant after myomectomy and pregnancy-associated complications, such as early pregnancy loss, recurrent miscarriage [10-12].
Myomectomy is the best and, probably, only approach for treating symptomatic uterine myomas in reproductive-aged women desiring to preserve childbearing potential, even if various treatments have been proposed (e.g., expectant management, medical therapy, uterine artery embolization or ligation). Several consensus statements and guidelines agreed that myomectomy may be the best therapeutic option in women who desire a pregnancy and/or patients in infertility [13].
Many studies reported the superiority of laparoscopic myomectomy compared to laparotomic approach, because the former is associated with a shorter hospital stay and recovery time and less postoperative pain and less blood loss compared with laparotomic myomectomy [3,4]. In the present retrospective study, we also found that laparoscopic myomectomy had less decrease of postoperative hemoglobin, despite similar operative time. It has been reported that incidence of intra-abdominal adhesions is significantly lower following laparoscopy than after laparotomy [14].
Despite these benefits, the biggest barrier to widespread implementation of laparoscopic myomectomy is the lack of experience and skill in enucleating and extracting myomas, and in performing multilayer suture. In general, selection of appropriate patients depends on the size and number of myomas, location of myomas relative to vessels, depth of penetration into myometrium, and adhesions associated with endometriosis [4]. And limitations in implementation of laparoscopic myomectomy have been allayed by selecting proper patients.
Several complications have been urged in laparoscopic myomectomy, the most concerned and worrisome complication of laparoscopic myomectomy is a pregnancy related uterine rupture. Though it composed only small proportion of complication, it can be lethal to both pregnant women and her baby when it occurs. Table 3 showed case reports of peripartum uterine rupture after laparoscopic myomectomy found in the literature [15-33]. Among them, 4 ended in nonviable fetus in mid-trimester, 2 ended in neonatal death and placental accident such as placental abruption or percreta were reported in 3 cases. The majority of uterine rupture occurred before the start of labor in mid- or early third-trimester. Interestingly, there was one neonatal death without placenta accident in a woman with twin pregnancy at 24 weeks of gestation. With exceptions of nonviable fetuses, it is the case of uterine rupture in the earliest period of gestation. Even though it may be impetuous to make a conclusion, enlarged uterine size in twin pregnancy could be responsible for this disastrous result.
Previous report suggests that the risk factors for uterine rupture are single layered closure of uterine wall and frequent use of electrocautery. Single-layer suturing on myometrial defect has been reported to have 4-fold risk of rupture during labor when compared with 2-layer closure [34]. Thus it seems reasonable for surgeons to adhere to techniques developed for abdominal myomectomy including limited use of electrocautery and multilayered closure of the myometrium. Surgical factors potentially related wound healing in myometrium including the method used for myometrial hemostasis, the extent of local tissue destruction, the method used to close the myometrial defect, the presence of infection or hematoma formation within myometrium, individual healing characteristics related to production of growth factor, and body mass index may contribute to uterine rupture during pregnancy [35]. Indeed, it was reported that in some patients, uterine rupture during pregnancy after laparoscopic myomectomy is rare even following single layered myometrial closure [4].
Laparoscopic myomectomy can be performed by adequately trained and experienced surgeon in well selected patients. Nevertheless, uterine rupture is a fatal complication and the risk is unpredictable. When considering laparoscopic myomectomy in reproductive aged women, the risk should not be overlooked.
Figures and Tables
References
1. Vollenhoven BJ, Lawrence AS, Healy DL. Uterine fibroids: a clinical review. Br J Obstet Gynaecol. 1990; 97:285–298.
2. Buttram VC Jr, Reiter RC. Uterine leiomyomata: etiology, symptomatology, and management. Fertil Steril. 1981; 36:433–445.
3. Jin C, Hu Y, Chen XC, Zheng FY, Lin F, Zhou K, et al. Laparoscopic versus open myomectomy: a meta-analysis of randomized controlled trials. Eur J Obstet Gynecol Reprod Biol. 2009; 145:14–21.
4. Parker WH. Laparoscopic myomectomy and abdominal myomectomy. Clin Obstet Gynecol. 2006; 49:789–797.
5. Li TC, Mortimer R, Cooke ID. Myomectomy: a retrospective study to examine reproductive performance before and after surgery. Hum Reprod. 1999; 14:1735–1740.
6. Paul PG, Koshy AK, Thomas T. Pregnancy outcomes following laparoscopic myomectomy and single-layer myometrial closure. Hum Reprod. 2006; 21:3278–3281.
7. Palomba S, Zupi E, Falbo A, Russo T, Marconi D, Tolino A, et al. A multicenter randomized, controlled study comparing laparoscopic versus minilaparotomic myomectomy: reproductive outcomes. Fertil Steril. 2007; 88:933–941.
8. Yoo EH, Kim D. Obstetric outcomes after laparoscopic myomectomy. Korean J Obstet Gynecol. 2008; 51:1481–1486.
9. Borgfeldt C, Andolf E. Transvaginal ultrasonographic findings in the uterus and the endometrium: low prevalence of leiomyoma in a random sample of women age 25-40 years. Acta Obstet Gynecol Scand. 2000; 79:202–207.
10. Bulletti C, DE Ziegler D, Levi Setti P, Cicinelli E, Polli V, Stefanetti M. Myomas, pregnancy outcome, and in vitro fertilization. Ann N Y Acad Sci. 2004; 1034:84–92.
11. Bulletti C, De Ziegler D, Polli V, Flamigni C. The role of leiomyomas in infertility. J Am Assoc Gynecol Laparosc. 1999; 6:441–445.
12. Saravelos SH, Yan J, Rehmani H, Li TC. The prevalence and impact of fibroids and their treatment on the outcome of pregnancy in women with recurrent miscarriage. Hum Reprod. 2011; 26:3274–3279.
13. Sinclair D, Gaither K, Mason TC. Fertility outcomes following myomectomy in an urban hospital setting. J Natl Med Assoc. 2005; 97:1346–1348.
14. Gutt CN, Oniu T, Schemmer P, Mehrabi A, Buchler MW. Fewer adhesions induced by laparoscopic surgery? Surg Endosc. 2004; 18:898–906.
15. Tsankova M, Nikolov A, Bosev D, Pirnareva E. Spontaneous uterine rupture in third trimester twin ivf pregnancy following myomectomy. Akush Ginekol (Sofiia). 2012; 51:50–53.
16. Pistofidis G, Makrakis E, Balinakos P, Dimitriou E, Bardis N, Anaf V. Report of 7 uterine rupture cases after laparoscopic myomectomy: update of the literature. J Minim Invasive Gynecol. 2012; 19:762–767.
17. Torbe A, Mikolajek-Bedner W, Kaluzynski W, Gutowska-Czajka D, Kwiatkowski S, Blogowski W, et al. Uterine rupture in the second trimester of pregnancy as an iatrogenic complication of laparoscopic myomectomy. Medicina (Kaunas). 2012; 48:182–185.
18. Tischner I, Tan TL, Uchil D, Brown RN. Prelabor uterine rupture after laparoscopic repair of uterine perforation. J Minim Invasive Gynecol. 2010; 17:265–267.
19. Goynumer G, Teksen A, Durukan B, Wetherilt L. Spontaneous uterine rupture during a second trimester pregnancy with a history of laparoscopic myomectomy. J Obstet Gynaecol Res. 2009; 35:1132–1135.
20. Kelly BA, Bright P, Mackenzie IZ. Does the surgical approach used for myomectomy influence the morbidity in subsequent pregnancy? J Obstet Gynaecol. 2008; 28:77–81.
21. Parker WH, Iacampo K, Long T. Uterine rupture after laparoscopic removal of a pedunculated myoma. J Minim Invasive Gynecol. 2007; 14:362–364.
22. Banas T, Klimek M, Fugiel A, Skotniczny K. Spontaneous uterine rupture at 35 weeks' gestation, 3 years after laparoscopic myomectomy, without signs of fetal distress. J Obstet Gynaecol Res. 2005; 31:527–530.
23. Grande N, Catalano GF, Ferrari S, Marana R. Spontaneous uterine rupture at 27 weeks of pregnancy after laparoscopic myomectomy. J Minim Invasive Gynecol. 2005; 12:301.
24. Malberti S, Ferrari L, Milani R. Spontaneous uterine rupture in the third trimester of gestation after laparoscopic myomectomy: a case report. Minerva Ginecol. 2004; 56:479–480.
25. Matsunaga JS, Daly CB, Bochner CJ, Agnew CL. Repair of uterine dehiscence with continuation of pregnancy. Obstet Gynecol. 2004; 104:1211–1212.
26. Asakura H, Oda T, Tsunoda Y, Matsushima T, Kaseki H, Takeshita T. A case report: change in fetal heart rate pattern on spontaneous uterine rupture at 35 weeks gestation after laparoscopically assisted myomectomy. J Nippon Med Sch. 2004; 71:69–72.
27. Lieng M, Istre O, Langebrekke A. Uterine rupture after laparoscopic myomectomy. J Am Assoc Gynecol Laparosc. 2004; 11:92–93.
28. Hasbargen U, Summerer-Moustaki M, Hillemanns P, Scheidler J, Kimmig R, Hepp H. Uterine dehiscence in a nullipara, diagnosed by MRI, following use of unipolar electrocautery during laparoscopic myomectomy: case report. Hum Reprod. 2002; 17:2180–2182.
29. Dubuisson JB, Fauconnier A, Deffarges JV, Norgaard C, Kreiker G, Chapron C. Pregnancy outcome and deliveries following laparoscopic myomectomy. Hum Reprod. 2000; 15:869–873.
30. Hockstein S. Spontaneous uterine rupture in the early third trimester after laparoscopically assisted myomectomy: a case report. J Reprod Med. 2000; 45:139–141.
31. Pelosi MA 3rd, Pelosi MA. Spontaneous uterine rupture at thirty-three weeks subsequent to previous superficial laparoscopic myomectomy. Am J Obstet Gynecol. 1997; 177:1547–1549.
32. Dubuisson JB, Chavet X, Chapron C, Gregorakis SS, Morice P. Uterine rupture during pregnancy after laparoscopic myomectomy. Hum Reprod. 1995; 10:1475–1477.
33. Harris WJ. Uterine dehiscence following laparoscopic myomectomy. Obstet Gynecol. 1992; 80:545–546.
34. Bujold E, Bujold C, Hamilton EF, Harel F, Gauthier RJ. The impact of a single-layer or double-layer closure on uterine rupture. Am J Obstet Gynecol. 2002; 186:1326–1330.
35. Parker WH, Einarsson J, Istre O, Dubuisson JB. Risk factors for uterine rupture after laparoscopic myomectomy. J Minim Invasive Gynecol. 2010; 17:551–554.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download