Abstract
Great advances have been made in the field of assisted reproductive technology (ART) since the first in vitro fertilization (IVF) baby was born in Korea in the year of 1985. However, it deserve to say that the invaluable data from fertility centers may serve as a useful source to find out which factors affect successful IVF outcome and to offer applicable information to infertile patients and fertility clinics. This article intended to report the status of ART in 2009 Korean Society of Obstetrics and Gynecology surveyed. The current survey was performed to assess the status and success rate of ART performed in Korea, between January 1 and December 31, 2009. Reporting forms had been sent out to IVF centers via e-mail, and collected by e-mail as well in 2012. With International Committee Monitoring Assisted Reproductive Technologies recommendation, intracytoplasmic sperm injection (ICSI) and non-ICSI cases have been categorized and also IVF-ET cases involving frozen embryo replacement have been surveyed separately. Seventy-four centers have reported the treatment cycles initiated in the year of 2009, and had performed a total of 27,947 cycles of ART treatments. Among a total of 27,947 treatment cycles, IVF and ICSI cases added up to 22,049 (78.9%), with 45.3% IVF without ICSI and 54.7% IVF with ICSI, respectively. Among the IVF and ICSI patients, patients confirmed to have achieved clinical pregnancy was 28.8% per cycle with oocyte retrieval, and 30.9% per cycle with embryo transfer. The most common number of embryos transferred in 2009 is three embryos (40.4%), followed by 2 embryos (28.4%) and a single embryo transferred (13.6%). Among IVF and ICSI cycles that resulted in multiple live births, twin pregnancy rate was 45.3% and triple pregnancy rate was 1.1%. A total of 191 cases of oocyte donation had been performed to result in 25.0% of live birth rate. Meanwhile, a total of 5,619 cases of frozen embryo replacement had been performed with 33.7% of clinical pregnancy rate per cycle with embryo transfer. When comparing with international registry data, clinical pregnancy rate per transfer from fresh IVF cycles including ICSI (34.1%,) was comparable to clinical pregnancy rate per transfer in European Society for Human Reproduction and Embryology report was 32.5% though lower than 45.0% for USA data. There was no remarkable difference in status of assisted reproductive technology in Korea between the current report and the data reported in 2008. The age of women trying to get pregnant was reconfirmed to be the most important factor that may have impact on success of ART treatment.
Ever since the first in vitro fertilization (IVF) baby was born in Korea in the year of 1985, great advances have been made in the field of assisted reproductive technology (ART) yielding noticeable progress in treatment outcome along with the increasing number of the fertility centers as well as the fertility treatment cycles.
Data from fertility centers where ART treatment is performed may serve as an abundant, valuable source to find out which factors affect successful IVF outcome and to offer applicable information to infertile patients and fertility clinics. It is also expected to ultimately suggest the direction of the fertility treatment based on the long-term analyses of the Korean ART data.
According to the pronouncement on the ethics of the artificial conception that certified ART clinics are to report the outcomes of the treatment cycles initiated in their clinics once a year to Korean Medical Association (KMA) or related institutions appointed by KMA (1993), consortium for monitoring IVF centers has been established within KMA in 1994. Bioethics and Safety Act was enacted in 2005, which required all the embryo-developing medical centers to be certified by Department of Health and Human Services. 152 centers have been certified as of June 2012.
Korean Society of Obstetrics and Gynecology (KSOG) has surveyed and reported the current status of Korean ART since 1992, and we hereby report the current status of ART in 2009 as a part of such survey project.
ART data from this survey will not only be helpful in gathering information about the current status of infertile patients as well as the fertility centers, but also serve as a useful data for continuous improvement and development of ART. We would like to pay deepest gratitude to those who have contributed in completing this report, including staff members of KSOG, Dr. Ji-Young Choi from Seoul National University Hospital, residents and fellows from Seoul National University Hospital, Dr. Gyoung Hoon Lee from Bucheon Seoul Women's Hospital, and those who belong to IVF centers in Korea that were willing to take part in the collection of Korea ART data.
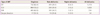
The purpose of this survey is to gather information about the current status and success rates of ART performed in Korea, between January 1 and December 31, 2009. Registration forms had been sent to 166 IVF centers which had been certified as embryo-generating medical institutions as of May 2011 (Fig. 1). Amongst these IVF centers, 74 had reported their outcome and the outcome data of 72 centers, which had actually performed ART treatment at that time, were gathered and analyzed accordingly. The IVF centers that had taken part in this survey are listed at Suppl. 1, and those that had performed ART treatment are marked with asterisks. IVF centers have been categorized according to the total number of treatment cycles initiated in 2009, as shown in Table 1.
Registration forms had been sent out to IVF centers via e-mail, and collected by e-mail as well. The example of the registration form that had been used is shown at Suppl. 2.
In this report, intracytoplasmic sperm injection (ICSI) and non-ICSI cases have been categorized, and also IVF-ET cases involving frozen embryo replacement have been surveyed separately.
All data is related to the treatment cycles to begin in 2009. Therefore, the analysis was made for the data from the treatment cycles that began in 2009. Clinical pregnancy was defined only in the cases which presented with clinical symptoms of pregnancy such as the presence of an intrauterine gestational sac on ultrasound examination or confirmation of gestational material through dilatation and curettage, but excluded the cases of biochemical pregnancy where only serum β-subunit of human chorionic gonadotrophin (β-hCG) was elevated. Gestational age had been marked down as 14 days (2 weeks) added to the time period between the fertilization and cessation of the pregnancy. SPSS ver. 14.0 (SPSS Inc., Chicago, IL, USA) was used to analyze the collected data.
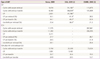
Seventy-four centers, which have reported the treatment cycles initiated in the year of 2009, had performed a total of 27,947 cycles of ART treatments (Table 2). Fifty-eight centers have performed 15,619 cases in 2000, 53 centers have performed 14,667 cases in 2001, 69 centers have performed 18,310 cases in 2002, 48 centers have performed 14,667 cases in 2003, 65 centers have performed 17,802 cases in 2004, 76 centers have performed 19,149 cases in 2005, 81 centers have performed 29,733 cases in 2006, 74 centers have performed 27,150 cases in 2007, and 78 centers have performed 28,029 cases in 2008 [1].
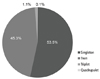
Among a total of 27,947 treatment cycles, IVF and ICSI cases added up to 22,049 (78.9%), 9,999 cases (45.3%) of IVF without ICSI and 12,050 cases (54.7%) of IVF with ICSI, elucidating the fact that most of the ART treatment cycles involved fresh embryos. 5,704 cases (20.4%) of frozen embryo replacement (FER), 191 cases (0.7%) of oocyte donation, and three cases of zygote intrafallopian transfer (ZIFT) had been performed. There was not a single case of gamete intrafallopian transfer (GIFT) performed in 2009 (Table 2, Fig. 2).
Among the patients who have had IVF and ICSI done, a total of 6,062 patients were confirmed to have achieved clinical pregnancy, which is 28.8% per cycle with oocyte retrieval, and 30.9% per cycle with embryo transfer, and 5,196 patients were estimated to have given live births, which is 24.7% per cycle with oocyte retrieval and 26.5% per cycle with embryo transfer (Table 2).
The age distribution of the patients who have had IVF and ICSI performed is as follows: age group below 25 was 0.7%, 25-29 was 10.1%, 30-34 was 46.1%, 35-39 was 36.0%, and age group over 40 was 7.1%. The age group of 30-39 was 82.1% of all cases, composing the majority of the cases (Table 3, Fig. 3).
The clinical pregnancy rate per retrieval is as follows according to each age group: age group below 25 was 13.1%, 25-29 was 12.3%, 30-34 was 19.9%, and 35-39 was 21.6%, and age group over 40 was 10.9%, showing statistically significant difference amongst the age groups (P < 0.001) (Table 3, Fig. 4).
The distribution of the indications of ART treatment, or rather the causes of infertility, of the subjects who have had IVF and ICSI performed is as follows: female factor only comprised 44.7%, male factor only comprised 21.2%, mixed male and female factors was 7.4%, unexplained infertility comprised 24.5%, and other miscellaneous factors comprised 2.2% (Table 4, Fig. 5).
Clinical pregnancy rate retrieval was 17.1% for female factor only, 14.9% for male factor only, 23.9% for mixed male and female factors, 22.1% for unexplained infertility, and other miscellaneous factors comprised 23.6%, showing statistically significant difference among the causes of infertility (P < 0.001) (Table 4, Fig. 6).
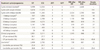
The number of embryos transferred in 2009 is as follows: a single embryo was transferred in 13.6%, two embryos were transferred in 28.4%, three embryos were transferred in 40.4%, four embryos were transferred in 13.9%, five embryos were transferred in 3.3%, and six or more embryos were transferred in 0.3% of the cases (Table 5).
The clinical pregnancy rate per transfer was 18.8% for a single embryo, 33.5% for two embryos, 33.7% for three embryos, 33.6% for four embryos, 25.3% for five embryos, and 37.3% for six embryos or more, showing significant difference in the pregnancy rate among different number of embryo(s) transferred (P < 0.001) (Table 5).
Among IVF and ICSI cycles that resulted in live births, singleton pregnancy rate was 53.5%, twin pregnancy rate was 45.3%, triplet pregnancy rate was 1.1%, and quadruplet pregnancy rate was 0.1%. Compared to the incidence of the twin pregnancy in general population which is known as 3% [1], multiple pregnancy rates is in fact very high (Table 6, Fig. 7).
A total of 191 cases of oocyte donation had been performed, followed by 168 cases of embryo(s) transfer. Clinical pregnancy rate per cycle with embryo(s) transfer was 45.8%, and live birth rate was 25.0% (Table 2).
There was not a single case of GIFT performed in 2009 (Table 2). Compared to 63 cases of GIFT performed in 2001, there had been much decrease in the number of GIFT cases. In 2005 and 2006, one case of GIFT had been performed each year, and in 2007, there had not been a single case performed, followed by two cases of GIFT in 2008 [1]. A total of three cases of ZIFT had been performed in 2009, without successful result (Table 2).
A total of 5,704 cases of frozen embryo replacement had been attempted in 2009, and a total of 5,619 cases of frozen embryo replacement had been actually performed. Clinical pregnancy rate per cycle with embryo transfer was 33.7%, whereas live birth rate was 24.9% (Table 2). In 2008, a total of 5,399 cases of frozen embryo replacement had been attempted, followed by 5,272 cases of frozen embryo replacement which resulted in clinical pregnancy rate per transfer of 33.1% and live birth rate of 27.7%. There was no statistically significant difference between the clinical pregnancy rate per transfer of 2009 and 2008, unlike that of live birth rate per transfer (P = 0.556 and P = 0.001, respectively). Clinical pregnancy rate and live birth rate per transfer of 2007 and 2008, (30.0% and 23.9%) had been reported earlier to have no significant difference (P = 0.875 and P = 0.513, respectively) [1].
The age distribution of the patients who had undergone frozen embryo replacement is as follows: the age group below 25 was 0.8%, 25-29 was 11.9%, 30-34 was 48.7%, 35-39 was 31.4%, and the age group over 40 was 7.3%, thus the age group of 30-39 composing the majority of the cases by taking 80.1% of all the reported cases (Table 7).
Clinical pregnancy rate per transfer according to the age group were 34.9% for the age group under 25, 35.8% for 25-29, 35.8% for 30-34, 33.6% for 35-39, 20.2% for over 40, showing no significant difference among the age groups (P < 0.001) (Table 7).
The number of embryos transferred is as follows: a single embryo was transferred in 17.1%, two embryos 34.7%, three embryos 30.8%, four embryos 13.8%, five embryos 3.3% and six embryos 0.4% (Table 8). Clinical pregnancy rate per transfer according to the number of embryos transferred was 26.1% for one embryo, 36.0% for two embryos, 39.0% for three embryos, 37.2% for four embryos, 31.3% for five embryos, and 13.0% for six embryos, showing significant difference in pregnancy rate amongst them (P < 0.001) (Table 8).
A total of 23 cases of microsurgical epididymal sperm aspiration had been performed in 2009, and pregnancy rate per retrieval was 34.8%, whereas live birth rate per retrieval was 4.3%. A total of 730 cases of testicular sperm extraction had been performed, and pregnancy rate per retrieval was 29.3%, whereas live birth rate per retrieval was 12.9%. 3,729 cases of assisted hatching had been performed in 2009, and the pregnancy rate per retrieval was 28.9%, whereas the live birth rate per retrieval was 12.1% (Table 9).
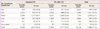
Korean ART outcome of 2009 has been compared with international registers as shown in Table 10. ART success rates (2009): National summary and fertility clinic reports [2] by Centers for Disease Control and Prevention in 2011 as for United States of America and Assisted Reproductive Technology in Europe [3] (2008) generated from 36 European countries by European Society for Human Reproduction and Embryology (ESHRE) is compared. When comparing fresh IVF cycles including ICSI, clinical pregnancy rate per transfer was 45.0% for USA, significantly higher than that of Korea (34.1%, P < 0.001), whereas clinical pregnancy rate per transfer in ESHRE report was 32.5% (Table 10). As for frozen embryo replacement, clinical pregnancy rate per transfer was 36.4% in USA, significantly higher than that of Korea (33.7%, P < 0.001). However, when the outcomes of frozen embryo replacement between Korea and European countries are compared, clinical pregnancy rate per transfer reported by ESHRE was 19.3%, statistically significantly lower than that of Korea (P < 0.001) (Table 10).
There was no remarkable difference of current status of ART in Korea between the current report and the data reported in 2008. As seen in international registers, frozen embryo replacement yielded significantly lower pregnancy rate statistically when compared to that of fresh cycles (P < 0.001) (Table 2). As part of important factors that may have impact on success of ART treatment, the age of women and the number of embryos transferred remained the same as those reports that had been reported before.
Figures and Tables
Fig. 2
Types of assisted reproductive technology procedures. IVF-ET, in vitro fertilization and embryo transfer; ICSI, intracytoplasmic sperm injection; FER, frozen embryos replacement; OD, oocyte donation.
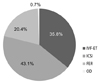
Fig. 3
Percentage of assisted reproductive technology users by ages: in vitro fertilization and intracytoplasmic sperm injection.
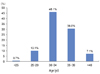
Fig. 4
Clinical pregnancy rates by age of woman, in vitro fertilization and intracytoplasmic sperm injection. CP, clinical pregnancy.
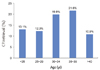
Fig. 5
Primary diagnosis for assisted reproductive technology procedures, in vitro fertilization and intracytoplasmic sperm injection.
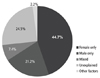
Fig. 6
Clinical pregnancy rates by cause of infertility, in vitro fertilization and intracytoplasmic sperm injection.
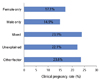
Table 9
Oocyte retrieval cycles, transfer cycles and pregnancies using special techniques of sperm collection and/or assisted hatching

References
1. ART committee, Korean Society of Obstetrics and Gynecology. Current status of assisted reproductive technology in Korea, 2006. Korean J Obstet Gynecol. 2009; 52:1212–1238.
2. Centers for Disease Control and Prevention, American Society for Reproductive Medicine, Society for Assisted Reproductive Technology. 2009 Assisted reproductive technology success rates: national summary and fertility clinic reports. Atlanta: U.S. Department of Health and Human Services;2011.
3. Ferraretti AP, Goossens V, de Mouzon J, Bhattacharya S, Castilla JA, Korsak V, et al. Assisted reproductive technology in Europe, 2008: results generated from European registers by ESHRE. Hum Reprod. 2012; 27:2571–2584.
Supplementary materials
Suppl. 1
IVF centers participated in this survey.
Supplementary material can be found via http://ogscience.org/src/sm/ogs-56-353-s001.pdf
Suppl. 2
Registration form of assisted reproduction: 2009.
Supplementary material can be found via http://ogscience.org/src/sm/ogs-56-353-s002.pdf




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download