This article has been
cited by other articles in ScienceCentral.
Abstract
Metastatic ovarian cancer is not an uncommon finding. Such tumors almost always originate from female genital tract, colon, stomach, or breast. Lung cancer is not a common origin of ovarian metastases. Of all metastatic ovarian tumors, approximately 0.3% arise from lung cancer. Ovarian torsion is not an uncommon finding, but ovarian torsion with cancer is rare. Here, we report a 44-year-old woman who was previously diagnosed with advanced stage lung cancer and who emergently visited our hospital for abdominal pain. An imaging work-up revealed, ovarian torsion and exploratory laparotomy was performed. Pathological examination led to the diagnosis ovarian metastasis from lung cancer. This is the first case of ovarian metastasis from lung cancer, ovarian torsion.
Go to :

Keywords: Lung cancer, Metastatic ovarian cancer, Ovarian torsion
Introduction
Metastatic ovarian cancer accounts for approximately 5% of all ovarian cancer case [
1]. Tumors originate from various sites, but most arise from the gastrointestinal tract or breast [
2]. Lung cancer is a rare origin of metastases, accounting for 0.3% of all metastatic ovarian tumors [
3]. The most common presenting symptoms are abdominal pain and distension that result from the presence of mass.
To the best of our knowledge, ovarian metastasis from lung cancer, with a manifestation of ovarian torsion has not been previously reported.
Go to :

Case report
A 44-year-old non-smoking Korean woman visited the local clinic with chest and back pain. A pulmonary nodule was seen on chest computed tomography (CT), and the patient was diagnosed with an unresectable pulmonary adenocarcinoma after performing bronchoscopy washing and right supraclavicular lymph node biopsy. After being diagnosed, she was transferred to Samsung Medical Center (SMC). At that time, brain, bone and pleural metastases were seen, therefore, the patient was treated with pemetrexed-cisplatin-based chemotherapy. After the forth cycle, the chest CT showed that the nodule had slightly decreased in size. At that point, the patient was planned to undergo the remaining chemotherapy cycles.
Three weeks later, she felt abrupt low abdominal pain. She then visited the hospital and underwent CT and laboratory testing. The CT revealed no specific findings except for a myoma-like mass in the pelvis. She was then transferred back to SMC. On physical examination, a fetal head size mass was detected in the lower abdomen, and the patient felt mild abdominal pain and tenderness. Tarchycardia and a mild fever were also noted.
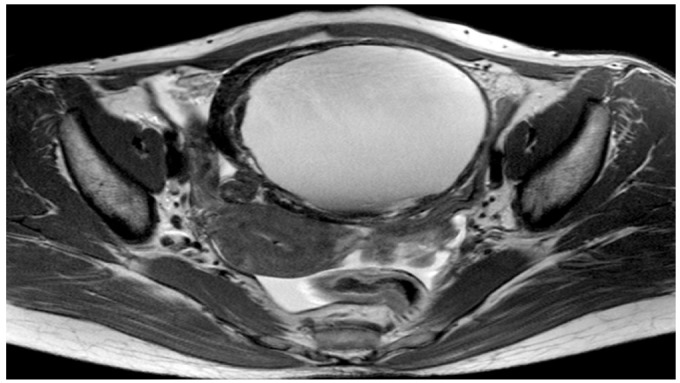
Ultrasound revealed, a 12.55 × 8.29 cm diffuse hypoechoic cystic mass with papillary projection in the pelvic cavity. Magnetic resonance imaging (MRI) and CT imaging revealed a 12 × 9.3 cm cystic and solid mass arising from the right adnexa as well as a torsion knob and hemorrhage, suggesting torsion of a cyst on the right ovary (
Fig. 1). CA-125 and CA-19-9 values were within the normal ranges.
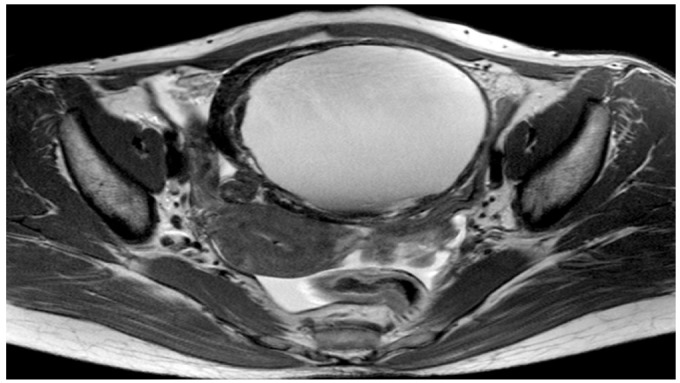 | Fig. 1Magnetic resonance imaging with 12 × 9.3 cm cystic and solid mass arising from the right adnexa as well as a torsion knob and hemorrhage, suggesting torsion of a cyst on the right ovary. 
|
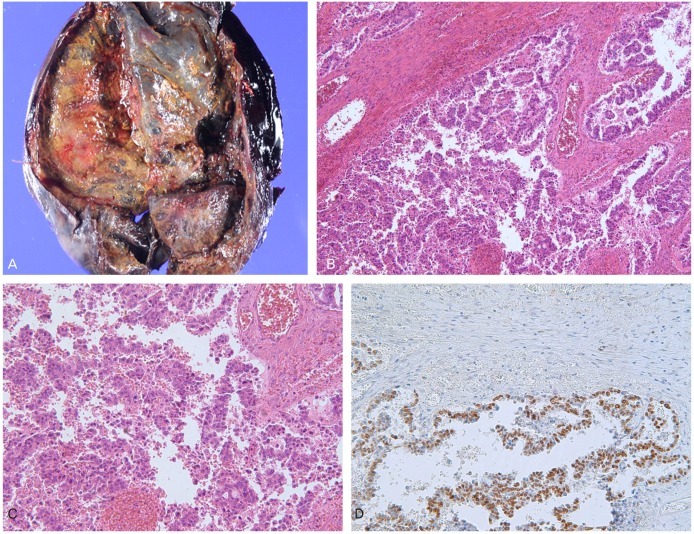
The patient subsequently underwent an exploratory laparotomy, during which a 10 cm right ovarian cyst with significant torsion of >720 degrees. Frozen section of the right ovarian specimen demonstrated malignancy. Bilateral salpingo-oophectomy, total abdominal hysterectomy and partial omentectomy was performed. Gross pathological examination showed 12 ×10 cm of right ovarian tumor and cystic space showing a black hemorrhage and solid portion. Microscopic pathology revealed metastatic adenocarcinoma on the right ovary, no evidence of malignancy was seen in the left ovary, uterus, or omentum (
Fig. 2).
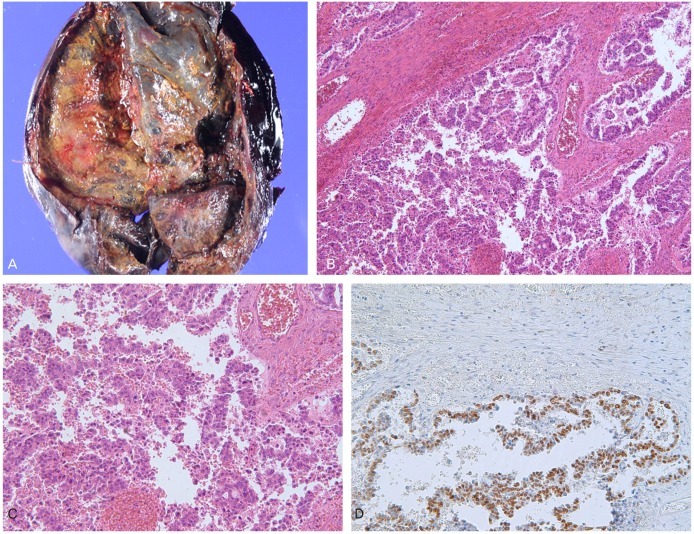 | Fig. 2(A) In gross finding, 12 × 10 cm of right ovarian tumor and cystic space showing a black hemorrhage and solid portion. (B) In microscopic finding, ovarian mass shows glandular structure and resemble the normal lung gland (H&E, ×40). (C) In high power field, tumor cells contain cuboidal to low-columnar cells with cytologic atypia, including hyperchromasia, pleomorphism and prominent nucleoli (H&E, ×200). (D) The tumor cells express TTF-1, which means that they metastasized from lung (TTF-1, ×200). 
|
After the surgery, a chest CT showed no interval change of the lung, pleura, lymph node size, while brain MRI showed slightly increased multiple brain metastatic lesions. Her lung cancer was followed by an oncologist who changed chemotherapy regimen to crizotinib, the target therapy. With regular follow-up imaging, she has remained on crizotinib until now (27 months), and underwent gamma knife surgery twice as well as 2 cycles of radiotherapy (brain, spine). With crizotinib, her condition and cancer mass are stable, therefore, the oncologist is continuing the target therapy.
Go to :

Discussion
Metastatic ovarian cancer is not an uncommon finding, as it represents approximately 5% to 20% of all ovarian cancers [
1,
4]. Common primary source of ovarian metastases includes breast, colon and gastric cancer. However, the most common sites are inconsistently reported and vary by region. In Sweden, breast cancer is the most common primary origin, in Korea, gastric cancer is the most common primary origin [
5,
6]. Lung cancer is a rare origin of ovarian metastases, but it is consistently reported. Because of its rarity, it was not found in some reports of primary cancers causing metastatic ovarian cancers. In a large study, lung cancer comprised about 0.4% of metastatic ovarian cancer origins [
7].
The 5-year survival rate of metastatic ovarian cancer is poorer than primary ovarian cancer [
6]. Treatment of primary ovarian cancer by maximum tumor resection, has demonstrated a survival benefit [
8]. However, the treatment strategy of metastatic ovarian cancer is ovarian metastatectomy and its benefit is limited. Due to differences in survival rates and treatment modalities, the differentiation between primary and secondary ovarian malignancy is important.
In general, for differentiation, patients must undergo various imaging techniques, including ultrasonography, CT, MRI as well as laboratory testing, including tumor markers. A solid mass and the absence of ascites on ultrasonography were significantly more prevalent among patients with a secondary ovarian malignancy than those with a primary ovarian malignancy [
4]. Nevertheless, preoperative differentiation between primary and metastatic ovarian cancer is difficult. Biopsy is the most accurate preoperative method for differentiating between primary and metastatic ovarian cancers, but there is a risk of disseminating cancer materials, therefore biopsy is not possible in all cases. Surgery is frequently indicated in the form of a diagnostic laparotomy for the ovarian mass as well as for symptom relief in most cases.
Metastasis from a pulmonary adenocarcinoma might be particularly difficult to be distinguished from primary ovarian carcinomas. Although there is no "lung-specific tumor marker", thyroid transcription factor-1 (TTF-1) can be used to discriminate between a primary lung tumor and a primary ovarian tumor. TTF-1 is positive in approximately 63% of primary lung cancers [
9].
Lung cancer is the leading cause of death. In Korea, the mortality rate of lung cancer in women increased by 35% over 10 years and lung cancer has been estimated to cause 21.7% of all cancer-related deaths in 2009, in Korea [
10]. The frequent metastatic sites of lung cancer include the pleura, mediastinal lymph node, bone, liver, and brain. Pulmonary metastases to the ovaries are extremely rare. In a small autopsy study of lung cancer, the tumors of approximately 5% of women had metastasized to the ovaries [
11].
Ovarian torsion consist of twisting of the vascular pedicle of an ovary that results in ischemia and acute onset of pain. Autonomic reflex response, nausea, emesis and tachycardia are usually present. Ovarian torsion is the fifth most common gynecological surgical emergency [
12]. Untreated torsion usually result in ovarian necrosis. Rarely, adnexal torsion may be the origin of complications that occur due to necrosis and the release of cytokines, which can cause pelvic thrombophlebitis or peritonitis [
12]. The most common cause of ovarian torsion is a mature cystic teratoma. Malignant ovarian tumors are the source of adhesions or invade the surrounding tissues therefore, they are less likely to cause adnexal torsion.
Ovarian metastases from lung cancer are uncommon, but clinicians must consider the possibility especially in patients with a history of lung cancer. As the incidence of lung cancer continues to increase, we can expect ovarian metastases from lung cancer to increase as well too.
There is no confident diagnostic tool for the differential diagnosis between primary and metastatic lung cancer, and surgery is frequently needed to make the diagnosis. Despite the fact that most cases of ovarian torsion are associated with benign ovarian cysts, we must keep in mind that the ovarian torsion can be a rare manifestation of cancer. If preoperative and intraoperative findings suggest malignancy, frozen section and a staging operation are necessary.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download