Abstract
Visual disturbances are common among women with pre-eclampsia. The obstetricians should have an understanding of the various conditions associated with visual impairments. We report a case of Purtscher-like retinopathy developed after pre-eclampsia combined with acute pancreatitis. A 33-year-old primigravida with twin pregnancy was admitted to the department of obstetrics and gynecology for preterm labor and pre-eclampsia at 36+4 weeks gestation. After a cesarean section, she complained of abdominal pain and visual acuity loss. She was diagnosed with Purtscher-like retinopathy combined with acute pancreatitis after ophthalmologic examination and an abdominal computed tomography scan. Purtscher-like retinopathy, most often observed after trauma, is very rare in pre-eclampsia. In addition, while visual disturbances from other conditions are transient, it can result in persistent visual impairments. Thus, when a patient with pre-eclampsia complains of visual problems for a long period of time, obstetricians should consider an ophthalmologic evaluation and treatments during the earliest stage of the disease.
Postpartum visual disturbance is often associated with pre-eclampsia or eclampsia, and these symptoms are generally transient [1,2]. Blindness in pre-eclampsia is very rare and may develop from brain damage or retinal lesions [3]. Blindness from retinal lesions is known as Purtscher-like retinopathy, and is caused by either retinal ischemia or infarction [3]. It has been estimated to develop in 0.24 cases per million in the UK [4]. Apart from the treatment of the precipitating conditions, there are no specific treatment guidelines at present [4,5]. Here, we report a rare case of Purtscher-like retinopathy after pre-eclampsia combined with acute pancreatitis, which resulted in persistent visual disturbance.
A 33-year-old primigravida was transferred to the Kyung Hee University Medical Center for preterm labor and pre-eclampsia at 36+4 weeks gestation. She had a twin pregnancy after in vitro fertilization-embryo transfer. Her blood pressure measured 140/100 mm Hg. Her urine protein was 4+ and 24-hour urinary protein excretion was 2,333 mg/day. She did not have headache, visual disturbances, or pitting edema. She had regular uterine contractions and a cervix dilated about 2 cm. An emergency cesarean section was performed uneventfully, and healthy twin babies were born.
On the second postoperative day, the patient had abdominal distension, steady epigastric and whole abdominal pain. An abdominal X-ray examination showed paralytic ileus. Laboratory examination showed white blood cell (WBC) count of 11,890, low Ca+ of 6.4 mg/dL, elevated blood urea nitrogen (BUN) of 64 mg/dL, serum creatinine of 1.5 mg/dL, aspartate transaminase (AST) of 52 IU/L, alanine aminotransferase (ALT) of 21 IU/L, elevated C-reactive protein (CRP) of 20.74 mg/dL, triglyceride 1,080 mg/dL and otherwise non-specific. At that time, she started complaining of blurry vision. Because pre-eclampsia-related visual disturbances are common, we did not perform a formal ophthalmic examination. We decided on conservative management including nasogastric drainage, parenteral nutrition, non per os, pain control, and avoidance of toxic renal medications.
On the fifth postoperative day, the patient had flank pain, diarrhea, tachycardia (pulse 112 per minutes) and fever (38℃). Laboratory examination showed WBC count of 14,900, low Ca+ of 5.6 mg/dL, AST of 61 IU/L, ALT of 33 IU/L, elevated CRP of 8.56 mg/dL, and normalized BUN and serum creatinine. Bacterial cultures were taken from blood and urine, and antibiotics were started. Her visual loss was equivocal.
The patient still had epigastric pain, a fever (38.3℃) and visual loss in both eyes until eight days after operation. At this point, we therefore decided to do an abdominal computed tomography (CT) scan and an ophthalmology consultation. The abdominal CT scan showed enlargement of pancreas with fat infiltration, fluid collection in the pancreatic area and no other abnormal findings. Serum amylase and lipase levels were elevated at 149 U/L (normal range, 25 to 125 U/L), and 128 U/L (normal range, 5.5 to 58 U/L) respectively, on the day of CT scan. The patient was diagnosed as having acute pancreatitis based on her steady epigastric pain and abdominal CT scan. She recovered fully upon resolution of pancreatic necrosis with conservative management and drainage of the underlying fluid collection.
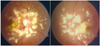
On the same day, the patient underwent an ophthalmologic examination, and her visual acuity test was 0.02 (right) and finger count 30 cm (left). There were multiple discrete retinal changes, and macular yellow patches, known as Purtscher flecken, in both eyes. A retinal splinter hemorrhage was seen in the right eye upon retinal photography (Fig. 1). A fluorescein angiogram showed arteriolar occlusion, and retinal ischemia, typical signs of Purtscher-like retinopathy. She was diagnosed with Purtscher-like retinopathy based on her symptoms and the results of the ophthalmologic examinations. Because there are no definite guidelines for the treatment of this condition, her visual acuity was closely monitored with conservative management. We also performed a brain magnetic resonance imaging (MRI) to rule out cortical blindness. The brain MRI showed unremarkable findings (Fig. 2). Two months after onset of visual loss, her visual acuity test was 0.08 (right) and 0.01 (left) and the multiple yellowish patches had decreased in both eyes on retinal photographs. At a recent follow-up (two years after the onset of her visual symptoms), her corrected visual acuity was 0.2 (right) and 0.1 (left). There was gradual improvement in the visual functions of both eyes, but she still had visual impairment.
Pre-eclampsia affects microvascular circulation and may involve cerebral, placental, hepatic, renal and ocular function [1]. Visual symptoms have been reported to occur in approximately 25% of patients with pre-eclampsia and 19% to 45% of patients with eclampsia, and include blurry vision, diplopia, amaurosis fugax, and photopsia [1,3]. Fortunately, pre-eclampsia-related visual acuity loss is usually reversible within weeks to months after the onset of symptoms [1-3]. In this case, because visual symptoms are relatively common with pre-eclampsia, serious ophthalmic diseases were not suspected when the patient complained visual problems at the first time. However, her visual symptoms had persisted until the eighth postoperative day, so we decided to perform a formal ophthalmologic examination. Purtscher-like retinopathy was confirmed according to the results of ophthalmologic examinations.
According to the recent study, the incidence of Purtscher's retinopathy estimate 0.24 case per million population per year based on the UK population of 58.8 million [4]. Purtscher's retinopathy is a rare condition, usually associated with severe head injury and blunt thoracic trauma, but also seen in patients with acute pancreatitis, fat embolism, renal failure, pre-eclampsia, childbirth and connective tissue disorders with vasculitis [4-8]. Especially Purtscher-like retinopathy is used to describe the retinopathy seen in conditions other than trauma [5]. Various systemic conditions mentioned above are attributed to the occlusion of retinal arterioles by aggregated granulocytes or platelets following complement activation, fat microemboli, or fibrin clots [4-6]. Most cases resolve spontaneously 1 to 3 months after systemic disease resolution [4-6]. Visual prognosis is variable, and is poor if optic disc swelling or leakage, choroidal hypoperfusion and involvement of the outer retina are seen upon intravenous fluorescein angiography [4,5]. At present no definite guidelines exist for the treatment of Purtscher-like retinopathy [4,5]. Although there are some case reports of successful treatment using high-dose steroids in IV form, the major treatment modality is expectancy [4,5]. The patient in this case had a gradual recovery of visual functions without treatments. However, she still has acuity impairments, and ophthalmologic follow up is ongoing.
Acute pancreatitis during pregnancy and postpartum is uncommon with an incidence of 1 case per 1,000 to 3,000 pregnancies [9]. Nearly 70% of cases of acute pancreatitis during pregnancy are secondary to biliary stones or sludge, followed by hyperlipidemia or alcohol abuse in approximately 20% of cases [9]. Pregnancy increases serum cholesterol and triglyceride levels, bile stasis, and may induce gallstone formation [9,10]. However, hyperlipidemia may directly induce acute pancreatitis [9,10]. The symptoms include the classic colicky or stabbing pain in the right upper quadrant or epigastric area, which can radiate to the right flank, scapula, and shoulder [10]. Diagnostic criteria for acute pancreatitis are presentation with at least two of the following three manifestations: 1) the typical symptoms mentioned above; 2) elevated levels of pancreatic enzyme (over three times of normal limit) in the blood, urine, or ascitic fluid; and 3) abnormal imaging findings in the pancreas associated with acute pancreatitis [9]. The general treatment of mild acute pancreatitis in pregnancy is conservative and supportive, while severe acute pancreatitis requires hospitalization in the intensive care unit and endoscopic or surgical interventions [9-11]. This patient had typical epigastric pain which was different from that normally seen after cesarean section, and abdominal CT findings compatible with acute pancreatitis. Because acute pancreatitis was not suspected initially, serum amylase and lipase were tested on eight days after symptom onset therefore the level were low for diagnosis of acute pancreatitis. The prolonged postoperative course with ileus, vague upper abdominal discomfort with mild tenderness, and hypocalcemia were likely secondary to acute pancreatitis. The disease resolved with protracted drainage of the fluid collected around the pancreas, broad-spectrum antibiotics and nutritional support.
To our knowledge, this is the first case report of Purtscher-like retinopathy developed after pre-eclampsia combined with acute pancreatitis in Korea. It is very meaningful that this case let us know there are several conditions that cause permanent visual disturbances after childbirth related to pre-eclampsia.
Figures and Tables
References
1. Roos NM, Wiegman MJ, Jansonius NM, Zeeman GG. Visual disturbances in (pre)eclampsia. Obstet Gynecol Surv. 2012. 67:242–250.
2. Dinn RB, Harris A, Marcus PS. Ocular changes in pregnancy. Obstet Gynecol Surv. 2003. 58:137–144.
3. Cunningham FG, Veno KJ, Bloom SL. Cunningham FG, Leveno KJ, Bloom SL, Hauth JC, Rouse DJ, Spong CY, editors. Pregnancy hypertension. Williams obstetrics. 2010. 23rd ed. New York (NY): The McGraw-Hill;706–750.
4. Agrawal A, McKibbin M. Purtschers retinopathy: epidemiology, clinical features and outcome. Br J Ophthalmol. 2007. 91:1456–1459.
5. Agrawal A, McKibbin MA. Purtschers and Purtscher-like retinopathies: a review. Surv Ophthalmol. 2006. 51:129–136.
6. Roncone DP. Purtschers retinopathy. Optometry. 2002. 73:166–172.
7. Stewart MW, Brazis PW, Guier CP, Thota SH, Wilson SD. Purtscher-like retinopathy in a patient with HELLP syndrome. Am J Ophthalmol. 2007. 143:886–887.
8. Cernea D, Dragoescu A, Novac M. HELLP syndrome complicated with postpartum subcapsular ruptured liver hematoma and Purtscher-like retinopathy. Case Rep Obstet Gynecol. 2012. 2012:856135.
9. Ducarme G, Chatel P, Alves A, Hammel P, Luton D. Management of necrotizing pancreatitis in the third trimester of pregnancy. Arch Gynecol Obstet. 2009. 279:561–563.
10. Parmar MS. Pancreatic necrosis associated with pre-eclampsia-eclampsia. JOP. 2004. 5:101–104.
11. Raheem M, Lala A, Abukhalil I. An aggressive presentation of postpartum acute necrotizing pancreatitis. J Obstet Gynaecol. 2004. 24:703–704.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download