1. Medawar PB. Some immunological and endocrinological problems raised by the evolution of viviparity in vertebrates. Symp Soc Exp Biol. 1953; 7:320–338.
2. Bonney EA, Matzinger P. The maternal immune system's interaction with circulating fetal cells. J Immunol. 1997; 158:40–47. PMID:
8977173.
3. Hutter H, Hammer A, Dohr G, Hunt JS. HLA expression at the maternal-fetal interface. Dev Immunol. 1998; 6:197–204. PMID:
9814593.

4. Munn DH, Zhou M, Attwood JT, Bondarev I, Conway SJ, Marshall B, et al. Prevention of allogeneic fetal rejection by tryptophan catabolism. Science. 1998; 281:1191–1193. PMID:
9712583.

5. Yoshida R, Hayaishi O. Indoleamine 2,3-dioxygenase. Methods Enzymol. 1987; 142:188–195. PMID:
3298973.
6. Yamazaki F, Kuroiwa T, Takikawa O, Kido R. Human indolylamine 2,3-dioxygenase. Its tissue distribution, and characterization of the placental enzyme. Biochem J. 1985; 230:635–638. PMID:
3877502.

7. Yoshida R, Urade Y, Tokuda M, Hayaishi O. Induction of indoleamine 2,3-dioxygenase in mouse lung during virus infection. Proc Natl Acad Sci U S A. 1979; 76:4084–4086. PMID:
291064.

8. Dai W, Pan H, Kwok O, Dubey JP. Human indoleamine 2,3-dioxygenase inhibits Toxoplasma gondii growth in fibroblast cells. J Interferon Res. 1994; 14:313–317. PMID:
7897249.
9. Dai W, Gupta SL. Molecular cloning, sequencing and expression of human interferon-gamma-inducible indoleamine 2,3-dioxygenase cDNA. Biochem Biophys Res Commun. 1990; 168:1–8. PMID:
2109605.
10. Moffett JR, Namboodiri MA. Tryptophan and the immune response. Immunol Cell Biol. 2003; 81:247–265. PMID:
12848846.

11. Steckel NK, Kuhn U, Beelen DW, Elmaagacli AH. Indoleamine 2,3-dioxygenase expression in patients with acute graft-versus-host disease after allogeneic stem cell transplantation and in pregnant women: association with the induction of allogeneic immune tolerance? Scand J Immunol. 2003; 57:185–191. PMID:
12588666.

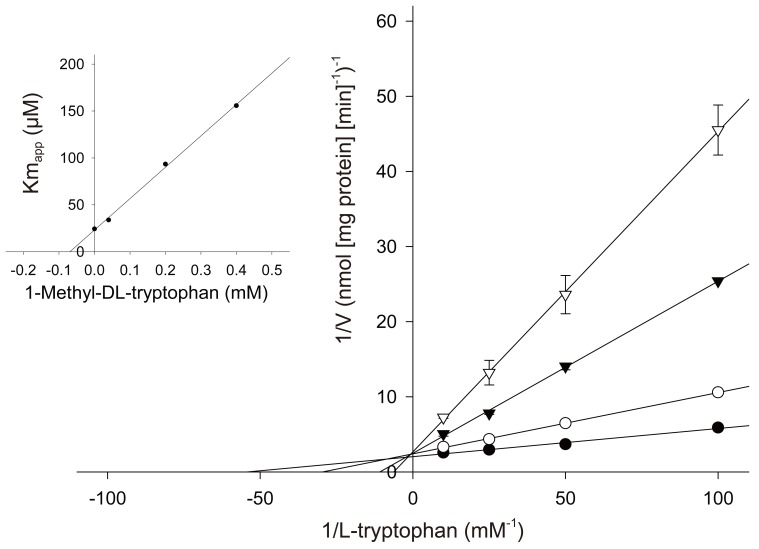
12. Cady SG, Sono M. 1-Methyl-DL-tryptophan, beta-(3-benzofuranyl)-DL-alanine (the oxygen analog of tryptophan), and beta-[3-benzo(b)thienyl]-DL-alanine (the sulfur analog of tryptophan) are competitive inhibitors for indoleamine 2,3-dioxygenase. Arch Biochem Biophys. 1991; 291:326–333. PMID:
1952947.
13. Pijnenborg R, Anthony J, Davey DA, Rees A, Tiltman A, Vercruysse L, et al. Placental bed spiral arteries in the hypertensive disorders of pregnancy. Br J Obstet Gynaecol. 1991; 98:648–655. PMID:
1883787.

14. Davidge ST. Oxidative stress and altered endothelial cell function in preeclampsia. Semin Reprod Endocrinol. 1998; 16:65–73. PMID:
9654609.

15. Roberts JM, Taylor RN, Musci TJ, Rodgers GM, Hubel CA, McLaughlin MK. Preeclampsia: an endothelial cell disorder. Am J Obstet Gynecol. 1989; 161:1200–1204. PMID:
2589440.

16. Barden A, Graham D, Beilin LJ, Ritchie J, Baker R, Walters BN, et al. Neutrophil CD11B expression and neutrophil activation in pre-eclampsia. Clin Sci (Lond). 1997; 92:37–44. PMID:
9038589.

17. Oian P, Omsjo I, Maltau JM, Osterud B. Increased sensitivity to thromboplastin synthesis in blood monocytes from pre-eclamptic patients. Br J Obstet Gynaecol. 1985; 92:511–517. PMID:
3922396.

18. von Dadelszen P, Wilkins T, Redman CW. Maternal peripheral blood leukocytes in normal and pre-eclamptic pregnancies. Br J Obstet Gynaecol. 1999; 106:576–581. PMID:
10426616.
19. Sacks GP, Studena K, Sargent K, Redman CW. Normal pregnancy and preeclampsia both produce inflammatory changes in peripheral blood leukocytes akin to those of sepsis. Am J Obstet Gynecol. 1998; 179:80–86. PMID:
9704769.

20. Kudo Y, Boyd CA, Spyropoulou I, Redman CW, Takikawa O, Katsuki T, et al. Indoleamine 2,3-dioxygenase: distribution and function in the developing human placenta. J Reprod Immunol. 2004; 61:87–98. PMID:
15063632.

21. Kudo Y, Boyd CA. Human placental indoleamine 2,3-dioxygenase: cellular localization and characterization of an enzyme preventing fetal rejection. Biochim Biophys Acta. 2000; 1500:119–124. PMID:
10564724.

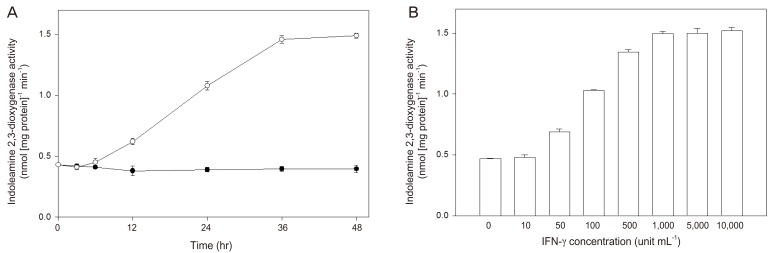
22. Takikawa O, Habara-Ohkubo A, Yoshida R. IFN-gamma is the inducer of indoleamine 2,3-dioxygenase in allografted tumor cells undergoing rejection. J Immunol. 1990; 145:1246–1250. PMID:
2116480.
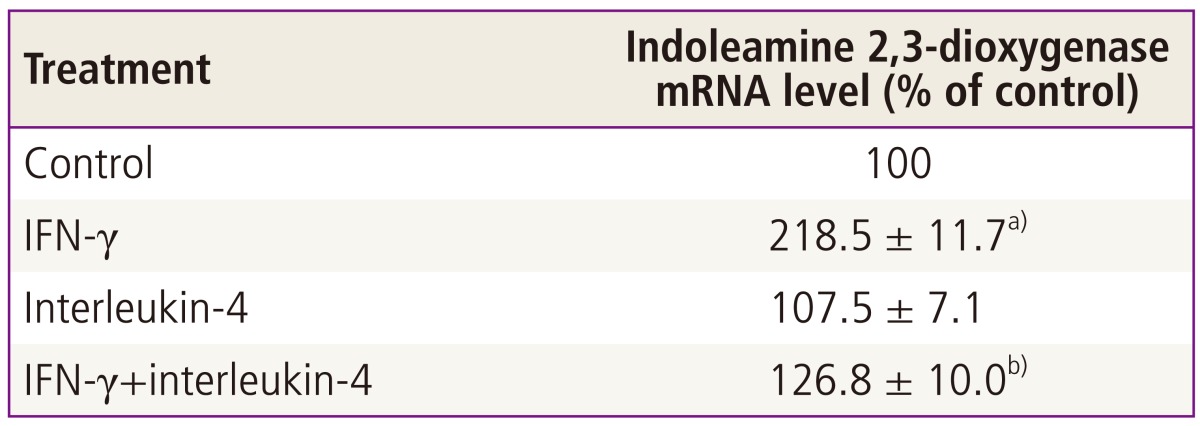
23. Musso T, Gusella GL, Brooks A, Longo DL, Varesio L. Interleukin-4 inhibits indoleamine 2,3-dioxygenase expression in human monocytes. Blood. 1994; 83:1408–1411. PMID:
8118042.

24. Kudo Y, Boyd CA, Sargent IL, Redman CW. Modulation of indoleamine 2,3-dioxygenase by interferon-gamma in human placental chorionic villi. Mol Hum Reprod. 2000; 6:369–374. PMID:
10729320.

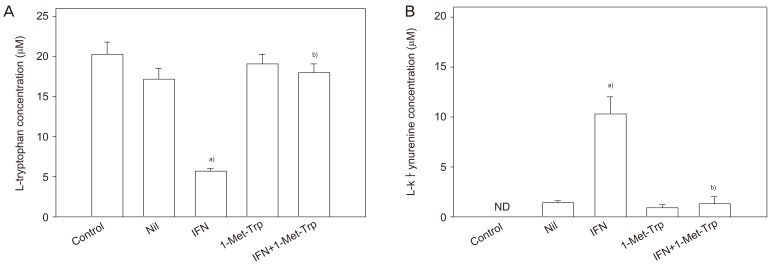
25. Kudo Y, Boyd CA. The role of L-tryptophan transport in L-tryptophan degradation by indoleamine 2,3-dioxygenase in human placental explants. J Physiol. 2001; 531:417–423. PMID:
11230514.
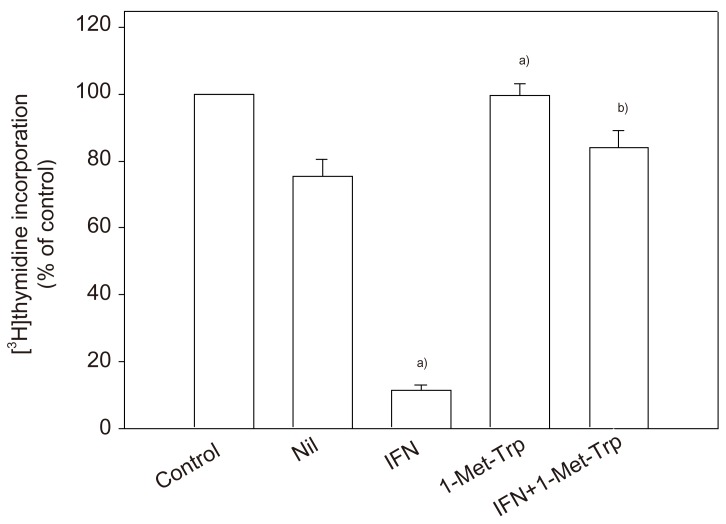
26. Kudo Y, Boyd CA, Sargent IL, Redman CW. Tryptophan degradation by human placental indoleamine 2,3-dioxygenase regulates lymphocyte proliferation. J Physiol. 2001; 535:207–215. PMID:
11507170.

27. Redman CW, Sacks GP, Sargent IL. Preeclampsia: an excessive maternal inflammatory response to pregnancy. Am J Obstet Gynecol. 1999; 180:499–506. PMID:
9988826.

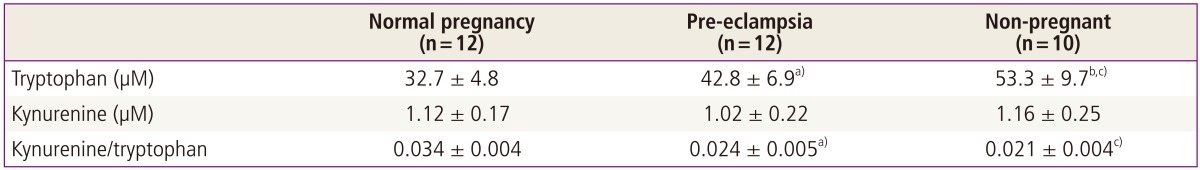
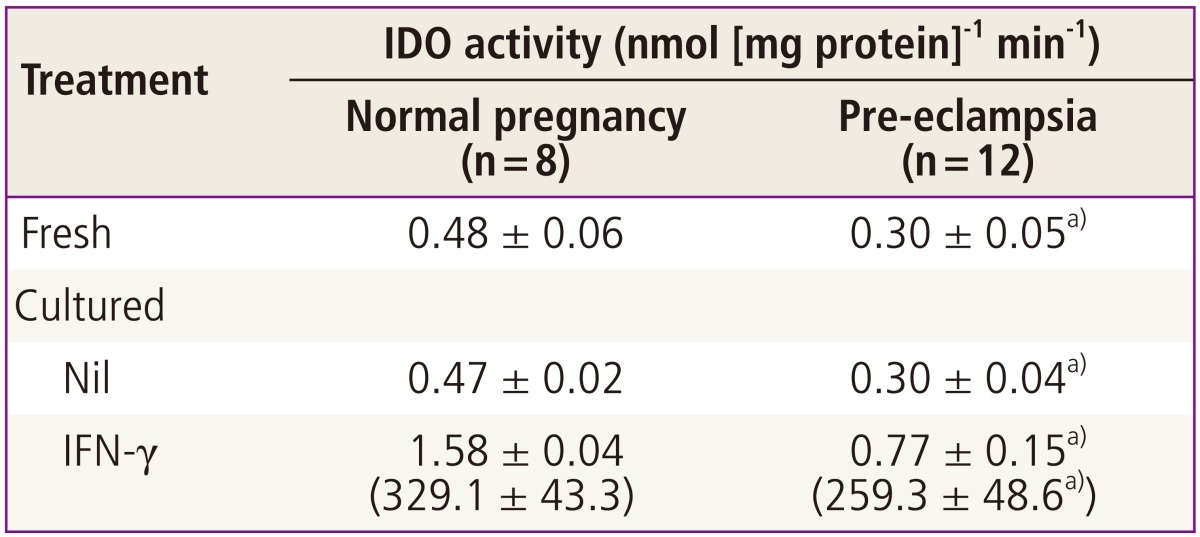
28. Kudo Y, Boyd CA, Sargent IL, Redman CW. Decreased tryptophan catabolism by placental indoleamine 2,3-dioxygenase in preeclampsia. Am J Obstet Gynecol. 2003; 188:719–726. PMID:
12634647.

29. Munn DH, Shafizadeh E, Attwood JT, Bondarev I, Pashine A, Mellor AL. Inhibition of T cell proliferation by macrophage tryptophan catabolism. J Exp Med. 1999; 189:1363–1372. PMID:
10224276.

30. Thellin O, Coumans B, Zorzi W, Igout A, Heinen E. Tolerance to the foeto-placental 'graft': ten ways to support a child for nine months. Curr Opin Immunol. 2000; 12:731–737. PMID:
11102780.

31. Redman CW, Sargent IL. Placental debris, oxidative stress and pre-eclampsia. Placenta. 2000; 21:597–602. PMID:
10985960.

32. Roberts JM, Cooper DW. Pathogenesis and genetics of pre-eclampsia. Lancet. 2001; 357:53–56. PMID:
11197372.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download