Abstract
The malignant transformation of a cystic teratoma is a rare event, occurring in about 0.2% to 1.8%. Primary malignant melanoma arising from the ovary is extremely rare. A primary melanoma in an ovarian cystic teratoma originates most frequently at the dermoepidermal junction, similar to a cutaneous melanoma. Though there are no standard adjuvant regimens for the treatment of primary malignant melanoma of the ovary. We present another case report of malignant melanoma developing in cystic teratoma.
Ovarian cystic teratoma is a common tumor. It is composed of multiple cell types derived from one or more of the three germ layers. The malignant transformation of a cystic teratoma is a rare event occurring in about 0.2% to 1.8% of cases. Squamous cell carcinoma is the most frequent malignancy (88.3%) [1], followed by adenocarcinoma, fibrosarcoma, carcinoid tumor and mixed tumors, in order of decreasing frequency [2]. A primary malignant melanoma arising from the ovary is extremely rare. It was first reported by Andrews [3] in 1901. Since then, 36 cases have been reported [4-6]. A primary melanoma in an ovarian cystic teratoma originates mostly at the dermoepidermal junction, similar to a cutaneous melanoma.
Here, we present a case report of a malignant melanoma developing in a teratoma.
A 75-year-old postmenopausal woman was admitted with gall stones and was incidentally found to have a mass in her abdomen. She had no significant gynecologic history. Epigastric tenderness was noted during the general physical examination. The pelvic examination revealed a 20×10 cm, smooth, mobile, nontender cystic mass to the anterior aspect of the uterus. An ultrasound examination showed a pelvic mass measuring approximately 17×11 cm with mixed echogenicity and a thin septation, with no ascites. Computed tomography (CT-scan) revealed a multi-lobulated 19×15 cm cystic mass with calcification and fat, suggesting a teratoma. The mass was located centrally in the pelvis, appearing to originate from the right side of the uterus with no enlarged lymph nodes (Fig. 1). A 1-cm-sized gall stone was also seen. The tumor marker, CA-125, level was elevated at 56.60 IU/mL (range, 0 to 35 IU/mL), and levels of carcinoembryonic antigen and alpha feto-protein were normal. A frozen section of the ovarian tissue at the time of the laparoscopy suggested a malignant tumor of unknown type. As such, the patient underwent a laparoscopic total hysterectomy with bilateral salpingo-oophorectomy with partial omentectomy with cholectystectomy. The diagnosis of a malignant melanoma in an ovarian cystic teratoma was made by histologic examination. Grossly, the right ovary showed a 20×14 cm sized cyst and was solid in appearance, containing sebaceous material. Microscopically, an infiltrating area of atypical pleomorphic cells having macronucleoli and melanin pigments was found in the background of the mature cystic teratoma (Fig. 2A-2C). These pleomorphic cells were positive for melan A (Fig. 2D) and HMB 45 (Fig. 2E).
The patient was re-evaluated, and the possibility of a melanoma at any other site, mainly skin, central nervous system, eye and gastrointestinal tract, was ruled out. Postoperatively, she received adjuvant immunotherapy with high-dose interferon (IFN)-α. Twelve months after the operation, a metastatic lesion of the liver was diagnosed. The patient underwent two cycles of Dacarbazine and two cycles of Cisplatin-Vinblastine-Dacarbazine chemotherapy. The patient died 17 months after the initial diagnosis.
Ovarian cystic teratoma is composed of multiple cell types derived from one or more of the three germ layers. The malignant transformation of a cystic teratoma is a rare event, occurring in about 0.2% to 1.8% of cases. Squamous cell carcinoma is the most frequent malignancy (88.3%) [1]. A primary malignant melanoma arising from the ovary is extremely rare and was first reported by Andrews [3] in 1901. Since then, 36 cases have been reported [4-6].
The ovary does not contain melanocytes. The rare diagnosis of an ovarian melanoma, however, may exist as a part of a teratoid lesion [7]. A primary melanoma in a teratoma originates most frequently at the dermoepidermal junction, similar to a cutaneous melanoma. It may also be derived from meningeal or uveal tissue within the teratoma.
Malignant transformation of a dermoid or teratoma is a rare event and must be differentiated from metastases of other primaries [1]. Some reports of a so-called primary melanoma of the ovary may be secondary to metastasis from an unknown primary or a primary which has been previously excised or spontaneously regressed [8].
Diagnostic criteria for an ovarian melanoma have been established by Cronje and Woodruff [9]. 1) No other primary tumor. 2) Unilateral ovarian tumor with the associated teratoid element. 3) Good correlation of patient age and symptoms with those of the well-documented cases in the literature. 4) Demonstration of melanocytic junctional activity (not mandatory for diagnosis).
Cronje and Woodruff [9] have proposed that evidence of primary origin is most convincing if lesions can be demonstrated to arise from a focus of preinvasive melanocytic proliferation, such as junctional activity in the cyst lining of the teratoma. It has been suggested that, if an ovarian cystic teratoma is associated with marked elevation of CA-19-9, lactate dehydrogenase, and squamous cell carcinoma related antigen, the possibility of a malignant melanoma arising in the teratoma should be considered [10]. However, because of the small number of cases in the literature, no definite preoperative diagnostic criteria have been established. In almost all of the reported cases, a preoperative diagnosis was not made or even suspected. A malignant transformation was suspected preoperatively by CT-scan in only one case [6].
Surgery is the mainstay of treatment; unilateral salpingooophorectomy or total abdominal hysterectomy with bilateral salpingo-oophorectomy with pelvic clearance is the treatment of choice [2]. Adjuvant treatment using chemotherapy or immunotherapy has not yet been established. To date, six patients have received varying combinations of chemotherapy, and one received chemotherapy plus immunotherapy [5]. As there are no standard adjuvant regimens for the treatment of primary malignant melanoma of the ovary, we decided to try high-dose IFN-α treatment considering the poor prognosis. This approach is based upon the results in patients with cutaneous melanoma and resected positive regional lymph nodes.
Melanomas arising in unusual sites are generally associated with a poorer prognosis than cutaneous melanomas. The International Federation of Obstetrics and Gynecology (FIGO) staging criteria provide no useful prognostic estimates. In spite of the low stages (FIGO stage IA1 or IA2), survival rates are poor. Of the 36 cases reported, 15 patients were dead within two years of primary diagnosis, eight of whom were FIGO state IA. Seven patients lived longer than two years, and only one patient had no evidence of disease at five years post-diagnosis. No information was available for five patients, and follow-up was less than two years in nine patients.
The pattern of spread is like that of epithelial ovarian cancer plus lymphatic and hematogenous routes, involving the lymph nodes, lung, liver and bone, and the prognosis is worse than squamous cell cancer in a dermoid cyst.
The present case was stage IA ovarian cancer and received postoperative immunotherapy. Twelve months after the initial operation, a metastatic lesion of liver was diagnosed, and the patient died 17 months after initial diagnosis. Her case is reported here as a primary malignant melanoma of the ovary treated with high dosage IFN-α.
Figures and Tables
Fig. 1
Precontrast (A, C) and contrast-enhanced (B, D) computed tomography-scan images show a multi-loculated 19×15 cm cystic mass with calcification (arrow) and fat (*), suggesting a teratoma.
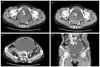
Fig. 2
There are an infiltrating area of atypical cells in the mature teratoma (A, H&E, ×100 ). The atypical cells have pleomorphic and bizarre nuclei with macronucleoli and melanin pigment (B, H&E, ×400). The tumor cells are found in the squamous epithelium lining the cystic lesion (C, H&E, ×400) showing diffuse strong positive for melan A (D) and HMB 45 (E, HMB stain ×400).

References
1. Crouet H, de Ranieri E, de Ranieri J. Secondary cancers arising in mature benign cystic teratomas of the ovary (dermoid cysts)Review of the literature apropos of a new case. J Gynecol Obstet Biol Reprod (Paris). 1986. 15:1055–1066.
2. Vimla N, Kumar L, Thulkar S, Bal S, Dawar R. Primary malignant melanoma in ovarian cystic teratoma. Gynecol Oncol. 2001. 82:380–383.
3. Andrews HR. Primary melanotic sarcoma of the ovary. Trans Obstet Soc. 1901. 43:228–231.
4. Moehrle M, Fischbach H, Nuessle B, Rassner G. Primary malignant melanoma arising in a cystic necrotic ovarian teratoma. Eur J Obstet Gynecol Reprod Biol. 2001. 99:268–271.
5. McNeilage LJ, Morgan J, Constable J, Jobling TW. Metastatic malignant melanoma arising in a mature ovarian cystic teratoma: a case report and literature review. Int J Gynecol Cancer. 2005. 15:1148–1152.
6. Moon JW, Kim JY, Shin YJ, Lee MY, Choi HJ, Park JY, et al. Primary malignant melanoma arising from ovarian mature cystic teratoma: a case report and literature review. Korean J Obstet Gynecol. 2010. 53:846–850.
7. Hermann WJ Jr, Humes JJ. A compound nevus in a benign cystic teratoma of the ovary. Am J Clin Pathol. 1976. 66:54–58.
8. Otero E, Haberland J, Valdes R, Hernandez P, Cabrera D. Malignant melanoma in an ovarian dermoid cyst. Rev Chil Obstet Ginecol. 1995. 60:43–45.
9. Cronje HS, Woodruff JD. Primary ovarian malignant melanoma arising in cystic teratoma. Gynecol Oncol. 1981. 12:379–383.
10. Nanbu Y, Fujii S, Konishi I, Nonogaki H, Mori T, Woodruff JD. Primary ovarian malignant amelanotic melanoma arising in cystic teratoma. Gynecol Oncol. 1990. 37:138–142.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download