Abstract
Objective
To assess the efficacies of once-weekly bisphosphonates on bone mineral density (BMD) gains in Korean women aged 50 years or more.
Methods
We selected 166 patients who received: alendronate 70 mg (n=48), alendronate 70 mg + cholecalciferol 2,800 IU (n=31) or risedronate 35 mg (n=87) for one year. The baseline BMD and the % changes of BMD at one-year were compared among the three medication groups.
Results
The menopausal status and number of women with osteoporosis was not different among the three groups, but mean age of women was significantly lower in alendronate group. Baseline BMD at L1-4 and femur neck (FN) was similar, but baseline BMD at femur total (FT) was significantly lower in alendronate group. After one-year use, the median % changes of BMD at three sites were similar among the three groups; however, the median values were highest in alendronate + cholecalciferol group (L1-4: 4.48%, 6.74%, and 4.50%; FT: 2.09%, 3.70%, and 2.31%; FN: 3.05%, 3.79%, and 2.03%).
Osteoporosis is an increased bone turnover and bone resorption leading to decreased bone mineral density (BMD) and strength and increased fracture risk [1]. The most common consequences of osteoporosis are fractures of the hip, wrist and vertebrae. The bisphosphonate classes of drugs are commonly used for the prevention and treatment for osteoporosis. These include alendronate, risedronate and ibandronate, which act to inhibit bone resorption by interfering with the activity of osteoclasts. During treatment of anti-resorptive agents, degree of bone turnover markers or BMD changes has been known to be closely associated with risk reduction of fractures [2].
Alendronate and risedronate were commonly used anti-resorptive agents. Alendronate at 10 mg/day for three years of treatment has been shown to increase BMD by 9% in the lumbar spine and 6% in the hip [3,4]. According to long term follow-up, alendronate increased BMD at the lumbar spine and maintained the bone turnover markers to level of the premenopausal women at least 10 years [5]. By using alendronate, the risk reduction was 48% for vertebral fracture and 37% to 55% for non-vertebral fracture and the effects were observed from 6 to 18 months after the treatment [6]. Also, Risedronate 5 mg/day for three years of treatment has been shown to increase BMD by 5% in the lumbar spine, 2% in the femur neck, and 3% in the femur trochanter in postmenopausal women with history of vertebral fracture [7]. The bone turnover marker reduction effect also observed but was smaller than alendronate. Reduction of fracture risk was 36% for vertebral fracture and 19% to 27% for non-vertebral fracture [8]. Unlike alendronate, reduction of fracture risk was observed in the first year of the administration of risedronate.
In order to compare the efficacy of different drugs, direct head-to-head study was required, but such studies are impractical in aspects of the cost or resources. Thus, measurement of BMD or bone turnover marker is commonly used instead of end-point of fracture. Currently, four kinds comparative studies exist, in which alendronate has been consistently reported to be superior to risedronate in terms of BMD or bone turn-over marker [9-12].
Calcium or vitamin D supplementations are commonly recommended as co-administration of bisphosphonates, but the compliance was low [13]. Therefore, new pharmaceutical product, alendronate 70 mg including cholecalciferol 2,800 IU, was developed in 2,000, and used worldwide. Comparative studies with regards its efficacy and compliance in Korean women are sparse. Until now, studies comparing three once weekly medications directly are not available. Thus, we attempted to assess the efficacies of once-weekly bisphosphonates on BMD gains in Korean women 50 year-old or more. Three commonly used anti-resorptive agents were included; alendronate 70 mg (Fosamax), alendronate 70 mg plus cholecalciferol 2,800 IU (Fosamax Plus), and risedronate 35 mg (Actonel). The changes of BMD at one-year were compared among the three groups, retrospectively.
The medical records of women who started once-weekly bisphosphonates between 2005 and 2007 at the Seoul National University Bundang Hospital were reviewed. The Institutional Review Board of the Seoul National University Bundang Hospital approved this retrospective study. We selected 166 women who received one of three drugs for one year: alendronate 70 mg (n=48), alendronate 70 mg plus cholecalciferol 2,800 IU (n=31) and risedronate 35 mg (n=87). The inclusion criteria were 1) Korean women aged 50 years or more at initiation of the medications, and 2) who never been used medications for their low BMD. The women who received any treatments for osteoporosis/osteopenia before the time of selection were entirely excluded. Menopause was defined as no natural menses for at least 1 year, or a serum follicle stimulating hormone (FSH) level >40 IU/L with a reported hysterectomy. Osteoporosis was diagnosed that patient had a BMD t-score of ≤-2.5 at the mean lumbar spine (L1-4), femoral neck or total, or a t-score of ≤-1.0 with radiological evidence of at least one vertebral fracture. Their menopausal state, other systemic illness, and co-medications such as calcium, estrogen or glucocorticoids were recorded.
BMD at baseline and one-year was recorded. BMD of the spine and hip was measured by Dual Energy X-ray absorptiometry (Lunar Prodigy whole-body scanner, GE Medical Systems, Madison, WI, USA). In the present study, we used BMD at three sites; L1-4, femur total and femur neck. The fracture event during medications was also recorded by reviewing medical records or contacting personally.
Age of women, baseline BMD, and % changes of BMD at one-year were calculated and presented as median (25th percentile, 75th percentile). The Kruskal-Wallis test was performed to compare median values among three medication groups because data from each group did not show a normal distribution. A P-value of <0.05 was considered statistically significant.
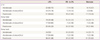
The baseline characteristics of the study subjects were presented in Table 1. The mean age of women was significantly lower in risedronate group. However, menopausal status and number of women with preexisting osteoporosis was not different among the three medication groups. Baseline BMD at L1-4 and femur neck was similar between three groups; however, baseline BMD at femur total was significantly lower in alendronate group. Number of women with calcium supplementation was significantly lower in alendronate plus cholecalciferol group; but use of estrogen or glucocorticoids (prednisolone or dexamethasone) was similar between three groups (Table 1).
After one-year use, the median % changes of BMD at three sites were similar among the three medication groups; however, the median values at all of three sites were highest in alendronate plus cholecalciferol group (Fig. 1). Among three once-weekly bisphosphonates, BMD gains were highest by use of alendronate plus cholecalciferol, although statistically not significant. In addition, non-response rate was the lowest in alendronate plus cholecalciferol group among 3 groups and this effect was particularly prominent in lumbar spine (Table 2).
This study demonstrated that the median % changes of BMD at three sites were similar among the three medication groups after one-year use. However, among three once-weekly bisphosphonates, BMD gains were highest by use of alendronate 70 mg+cholecalciferol 2,800 IU, although statistically not significant. In addition, non-response rate was the lowest in alendronate plus cholecalciferol group among 3 groups and this effect was particularly prominent in lumbar spine.
Bisphosphonates are approved drugs on prevention and treatment of osteoporosis. Therefore, these drugs are considered as a first-line therapy for the treatment of osteoporosis. Bisphosphonates inhibit osteoclast-mediated bone resorption, increase BMD, and decrease the risk of vertebral and other nonvertebral fractures. The four kinds of run in head-to-head study, alendronate have been consistently reported to be superior to risedronate at BMD gain or bone turnover markers [9-12].
Vitamin D deficiency and insufficiency are prevalent worldwide, especially among osteoporotic women. One epidemiological study from Korea has shown that 90.6% of postmenopausal women had vitamin D insufficiency [13]. Vitamin D regulates calcium and phosphorus absorption and plays a central role in the mineralization, growth and remodeling of bone. Previous studies have shown that serum vitamin D levels correlate positively with BMD [11]. There is also evidence to suggest that vitamin D reduces fracture risk, with antifracture efficacy best documented in older individuals receiving vitamin D3 supplementation at 700 to 800 IU per day. Barone et al. [14]. studied the effect of alendronate 70 mg weekly plus placebo versus alendronate 70 mg weekly plus 0.5 µg calcitriol daily (1,25(OH)2D3) on BMD in postmenopausal women with vitamin D insufficiency, a BMD of the spine or total hip or femoral neck <-2.5 standard deviation T-score. In that study, the increase of BMD of the spine was 3.7% in the alendronate alone and 6.5% in the alendronate plus calcitriol group after one-year treatment, which is statistically significant. Therefore, vitamin D supplement are widely prescribed as an adjunct to other osteoporosis treatments.
Unfortunately, adherence to these supplements is poor, despite the fact that coadministration of vitamin D with anti-osteoporosis therapy enhances the therapeutic response. One study reported that the rate of regular vitamin D intake on Korean osteoporosis woman was 21% [13]. Therefore, a fixed-dose combination of weekly alendronate 70 mg and cholecalciferol 2,800 IU has been introduced for the treatment of postmenopausal osteoporosis.
Yoon et al. [15] demonstrated that use of alondronate 70 mg with or without cholecalciferol 2,800 IU has no significant difference in BMD gain by comparative study. Recker et al. [16] conducted a 15-week, double-blind, randomized, active controlled clinical trial evaluated the safety and efficacy of a single once-weekly tablet containing alendronate 70 mg and cholecalciferol 2,800 IU. The once-weekly alendronate 70 mg with cholecalciferol 2,800 IU tablet provided equivalent anti-resorptive efficacy when compared with once-weekly alendronate 70 mg without cholecalciferol and improved vitamin D status. Our results are in line with that study.
As our knowledgement, this is the first study comparing the efficacy of commonly used three kinds of once weekly bisphosphonates in Korean women. In our study, the BMD gain between alendronate and risedronate was similar. Our results do not agree with previous head to head studies, but, the ethnic difference, uncontrolled compliance of the medication and calcium intake could be factors to lead this discrepancy. Addition of cholecalciferol 2,800 IU to alendronate 70 mg had some benefit for BMD gain thus this information appears to be valuable to manage osteoporotic women.
This study is a retrospective chart reviewed analysis which has several limitations, such as small sample size, no bone turnover marker measurements, significant differences in some baseline data, uncertainty of diagnose of osteoporosis, no history of fragility fractures, or incident vertebral fractures, no exclusion of subjects with low bone mass caused by secondary factors. In addition, we did not validate the accuracy of Dual Energy X-ray absorptiometry and error according to the inspector. Further prospective studies including patients' details (such as serum vitamin D, parathyroid hormone level, degree of sun exposure, use of sun cream) would be needed.
Figures and Tables
Fig. 1
Percent changes of bone mineral density at three sites after one-year use of medications (horizontal solid line within the box indicates the median, the box means 75 and 25 percentile, respectively, and upper and lower bar indicate 95 and 5 percentile, respectively).

References
1. Poole KE, Compston JE. Osteoporosis and its management. BMJ. 2006. 333:1251–1256.
2. Delmas PD, Seeman E. Changes in bone mineral density explain little of the reduction in vertebral or nonvertebral fracture risk with anti-resorptive therapy. Bone. 2004. 34:599–604.
3. Liberman UA, Weiss SR, Broll J, Minne HW, Quan H, Bell NH, et al. The Alendronate Phase III Osteoporosis Treatment Study Group. Effect of oral alendronate on bone mineral density and the incidence of fractures in postmenopausal osteoporosis. N Engl J Med. 1995. 333:1437–1443.
4. Cummings SR, Black DM, Thompson DE, Applegate WB, Barrett-Connor E, Musliner TA, et al. Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures: results from the Fracture Intervention Trial. JAMA. 1998. 280:2077–2082.
5. Bone HG, Hosking D, Devogelaer JP, Tucci JR, Emkey RD, Tonino RP, et al. Ten years' experience with alendronate for osteoporosis in postmenopausal women. N Engl J Med. 2004. 350:1189–1199.
6. Cranney A, Wells G, Willan A, Griffith L, Zytaruk N, Robinson V, et al. Meta-analyses of therapies for postmenopausal osteoporosis. II. Meta-analysis of alendronate for the treatment of postmenopausal women. Endocr Rev. 2002. 23:508–516.
7. Harris ST, Watts NB, Genant HK, McKeever CD, Hangartner T, Keller M, et al. Vertebral Efficacy With Risedronate Therapy (VERT) Study Group. Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. JAMA. 1999. 282:1344–1352.
8. Cranney A, Tugwell P, Adachi J, Weaver B, Zytaruk N, Papaioannou A, et al. Meta-analyses of therapies for postmenopausal osteoporosis. III. Meta-analysis of risedronate for the treatment of postmenopausal osteoporosis. Endocr Rev. 2002. 23:517–523.
9. Hosking D, Adami S, Felsenberg D, Andia JC, Valimaki M, Benhamou L, et al. Comparison of change in bone resorption and bone mineral density with once-weekly alendronate and daily risedronate: a randomised, placebo-controlled study. Curr Med Res Opin. 2003. 19:383–394.
10. Rosen CJ, Hochberg MC, Bonnick SL, McClung M, Miller P, Broy S, et al. Treatment with once-weekly alendronate 70 mg compared with once-weekly risedronate 35 mg in women with postmenopausal osteoporosis: a randomized double-blind study. J Bone Miner Res. 2005. 20:141–151.
11. Reid DM, Hosking D, Kendler D, Brandi ML, Wark JD, Weryha G, et al. Alendronic acid produces greater effects than risedronic acid on bone density and turnover in postmenopausal women with osteoporosis: results of FACTS-international. Clin Drug Investig. 2006. 26:63–74.
12. Reid DM, Hosking D, Kendler D, Brandi ML, Wark JD, Marques-Neto JF, et al. A comparison of the effect of alendronate and risedronate on bone mineral density in postmenopausal women with osteoporosis: 24-month results from FACTS-International. Int J Clin Pract. 2008. 62:575–584.
13. Chung HY, Chin SO, Kang MI, Koh JM, Moon SH, Yoon BK, et al. Efficacy of risedronate with cholecalciferol on 25-hydroxyvitamin D level and bone turnover in Korean patients with osteoporosis. Clin Endocrinol (Oxf). 2011. 74:699–704.
14. Barone A, Giusti A, Pioli G, Girasole G, Razzano M, Pizzonia M, et al. Secondary hyperparathyroidism due to hypovitaminosis D affects bone mineral density response to alendronate in elderly women with osteoporosis: a randomized controlled trial. J Am Geriatr Soc. 2007. 55:752–757.
15. Yoon JW, Lee BK, Song YC, Kim JY, Shin HY, Lee YH, et al. A comparison of effectiveness and compliance among alendronate pharmaceutical products in Koreans. Korean J Clin Pharm. 2008. 18:114–119.
16. Recker R, Lips P, Felsenberg D, Lippuner K, Benhamou L, Hawkins F, et al. Alendronate with and without cholecalciferol for osteoporosis: results of a 15-week randomized controlled trial. Curr Med Res Opin. 2006. 22:1745–1755.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download