1. Kopans DB. Breast imaging. 2th ed. Philadelphia (PA): Lippincott-Raven;1998.
2. Salazar H, Tobon H, Josimovich JB. Developmental, gestational and postgestational modifications of the human breast. Clin Obstet Gynecol. 1975; 18:113–137. PMID:
1139807.

3. Rosen PP. Anatomic and physiologic morphology. In : Rosen PP, editor. Rosen's breast pathology. 2nd ed. Philadelphia (PA): Lippincott-Raven;2001. p. 1–21.
4. Vorherr H. Human lactation and breast feeding. In : Larson BL, editor. Lactation: a comprehensive treatise. 2nd ed. New York (NY): Academic Press;1978. p. 182–280.
5. Neville MC. Physiology of lactation. Clin Perinatol. 1999; 26:251–279. PMID:
10394488.

6. Neville MC. Anatomy and physiology of lactation. Pediatr Clin North Am. 2001; 48:13–34. PMID:
11236721.

7. Hogge JP, De Paredes ES, Magnant CM, Lage J. Imaging and Management of Breast Masses During Pregnancy and Lactation. Breast J. 1999; 5:272–283. PMID:
11348301.

8. Liberman L, Giess CS, Dershaw DD, Deutch BM, Petrek JA. Imaging of pregnancy-associated breast cancer. Radiology. 1994; 191:245–248. PMID:
8134581.

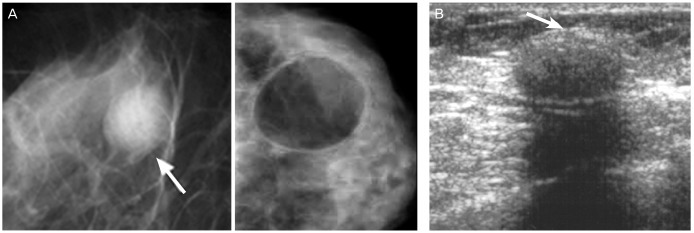
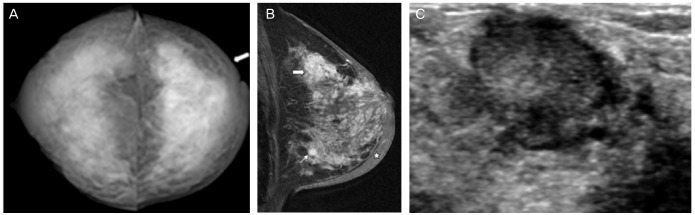
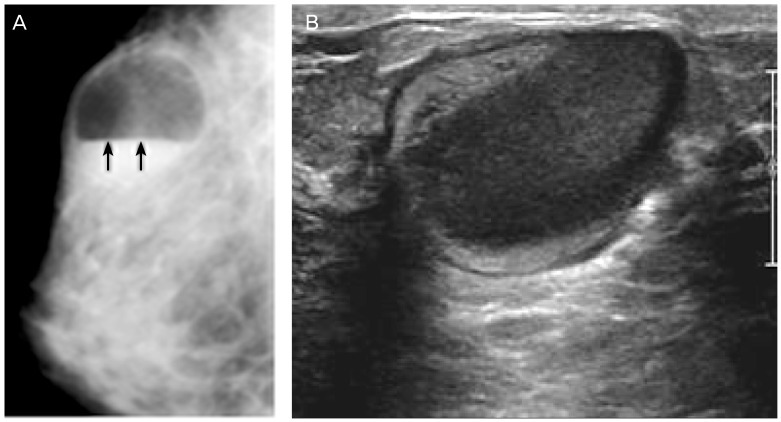
9. Ahn BY, Kim HH, Moon WK, Pisano ED, Kim HS, Cha ES, et al. Pregnancy- and lactation-associated breast cancer: mammographic and sonographic findings. J Ultrasound Med. 2003; 22:491–497. PMID:
12751860.
10. Samuels TH, Liu FF, Yaffe M, Haider M. Gestational breast cancer. Can Assoc Radiol J. 1998; 49:172–180. PMID:
9640283.
11. Son EJ, Oh KK, Kim EK. Pregnancy-associated breast disease: radiologic features and diagnostic dilemmas. Yonsei Med J. 2006; 47:34–42. PMID:
16502483.

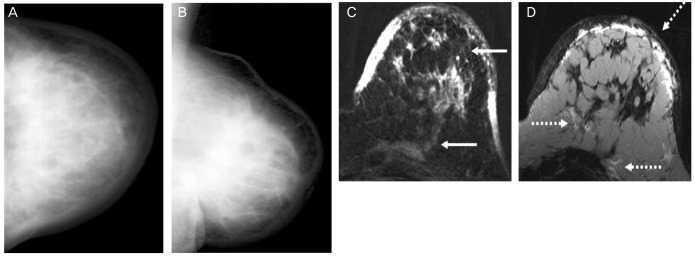
12. Yang WT, Dryden MJ, Gwyn K, Whitman GJ, Theriault R. Imaging of breast cancer diagnosed and treated with chemotherapy during pregnancy. Radiology. 2006; 239:52–60. PMID:
16484353.

13. Greskovich JF Jr, Macklis RM. Radiation therapy in pregnancy: risk calculation and risk minimization. Semin Oncol. 2000; 27:633–645. PMID:
11130470.
14. Osei EK, Faulkner K. Fetal doses from radiological examinations. Br J Radiol. 1999; 72:773–780. PMID:
10624343.

15. Kopans DB. Mammography and radiation risk. In : Janower ML, Linton OW, editors. Radiation risk: a primer. Reston (VA): American College of Radiology;1996. p. 21–22.
16. Kanal E, Borgstede JP, Barkovich AJ, Bell C, Bradley WG, Felmlee JP, et al. American College of Radiology White Paper on MR Safety. AJR Am J Roentgenol. 2002; 178:1335–1347. PMID:
12034593.

17. De Wilde JP, Rivers AW, Price DL. A review of the current use of magnetic resonance imaging in pregnancy and safety implications for the fetus. Prog Biophys Mol Biol. 2005; 87:335–353. PMID:
15556670.

18. Nagayama M, Watanabe Y, Okumura A, Amoh Y, Nakashita S, Dodo Y. Fast MR imaging in obstetrics. Radiographics. 2002; 22:563–580. PMID:
12006687.

19. Webb JA, Thomsen HS, Morcos SK. Members of Contrast Media Safety Committee of European Society of Urogenital Radiology (ESUR). The use of iodinated and gadolinium contrast media during pregnancy and lactation. Eur Radiol. 2005; 15:1234–1240. PMID:
15609057.

20. Mitre BK, Kanbour AI, Mauser N. Fine needle aspiration biopsy of breast carcinoma in pregnancy and lactation. Acta Cytol. 1997; 41:1121–1130. PMID:
9250309.

21. Gupta RK, McHutchison AG, Dowle CS, Simpson JS. Fine-needle aspiration cytodiagnosis of breast masses in pregnant and lactating women and its impact on management. Diagn Cytopathol. 1993; 9:156–159. PMID:
8513709.

22. Schackmuth EM, Harlow CL, Norton LW. Milk fistula: a complication after core breast biopsy. AJR Am J Roentgenol. 1993; 161:961–962. PMID:
8273635.

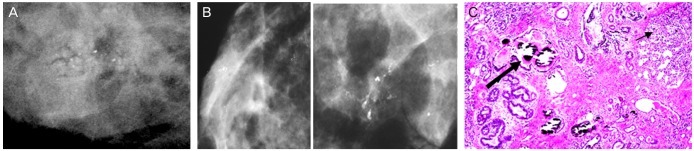
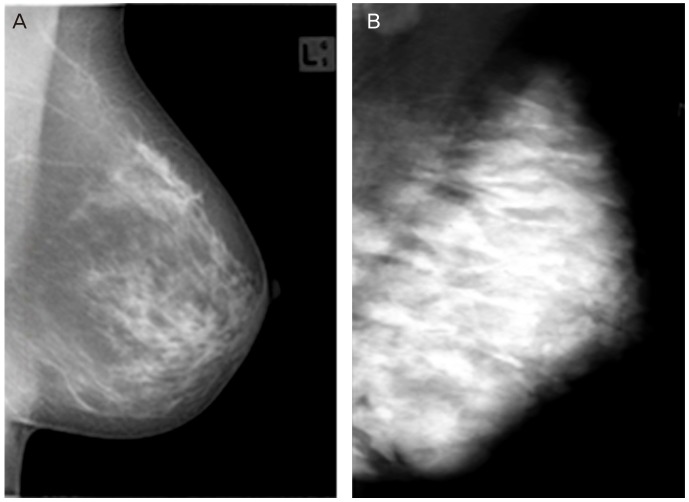
23. Stucker DT, Ikeda DM, Hartman AR, George TI, Nowels KW, Birdwell SL, et al. New bilateral microcalcifications at mammography in a postlactational woman: case report. Radiology. 2000; 217:247–250. PMID:
11012452.

24. Mercado CL, Koenigsberg TC, Hamele-Bena D, Smith SJ. Calcifications associated with lactational changes of the breast: mammographic findings with histologic correlation. AJR Am J Roentgenol. 2002; 179:685–689. PMID:
12185045.
25. Giron GL, Boolbol SK, Gross J, Cohen JM, Feldman S. Postlactational microcalcifications. Breast J. 2004; 10:247–252. PMID:
15125754.

26. Lafreniere R. Bloody nipple discharge during pregnancy: a rationale for conservative treatment. J Surg Oncol. 1990; 43:228–230. PMID:
2325421.

27. Kline TS, Lash SR. The bleeding nipple of pregnancy and postpartum period: a cytologic and histologic study. Acta Cytol. 1964; 8:336–340. PMID:
14208372.
28. O'Callaghan MA. Atypical discharge from the breast during pregnancy and/or lactation. Aust N Z J Obstet Gynaecol. 1981; 21:214–216. PMID:
6951562.
29. Scott-Conner CEH. Diagnosing and managing breast disease during pregnancy and lactation. Medscape Womens Health. 1997; 2:1. PMID:
9746691.
30. Rosen PP. Inflammatory and reactive tumors. In : Rosen PP, editor. Rosen's breast pathology. 2nd ed. Philadelphia (PA): Lippincott-Raven;2001. p. 29–63.
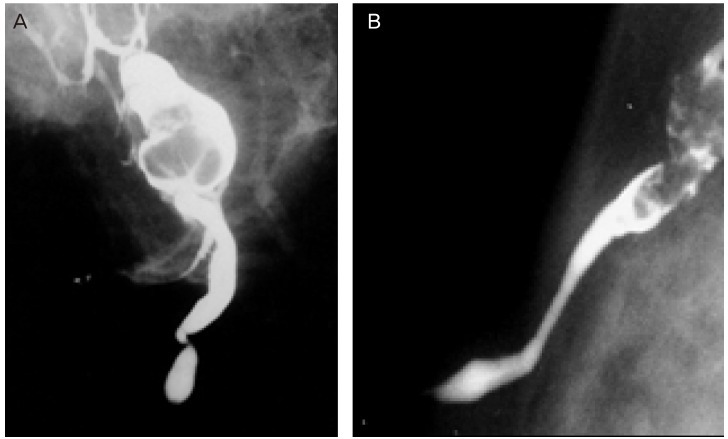
31. Gómez A, Mata JM, Donoso L, Rams A. Galactocele: three distinctive radiographic appearances. Radiology. 1986; 158:43–44. PMID:
3940395.

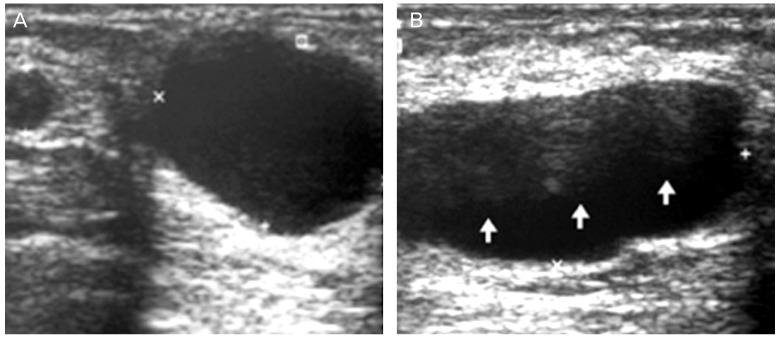
32. Sawhney S, Petkovska L, Ramadan S, Al-Muhtaseb S, Jain R, Sheikh M. Sonographic appearances of galactoceles. J Clin Ultrasound. 2002; 30:18–22. PMID:
11807850.

33. Kim MJ, Kim EK, Park SY, Jung HK, Oh KK, Seok JY. Galactoceles mimicking suspicious solid masses on sonography. J Ultrasound Med. 2006; 25:145–151. PMID:
16439776.

34. Stevens K, Burrell HC, Evans AJ, Sibbering DM. The ultrasound appearances of galactocoeles. Br J Radiol. 1997; 70:239–241. PMID:
9166046.

35. Stafford I, Hernandez J, Laibl V, Sheffield J, Roberts S, Wendel G Jr. Community-acquired methicillin-resistant Staphylococcus aureus among patients with puerperal mastitis requiring hospitalization. Obstet Gynecol. 2008; 112:533–537. PMID:
18757649.

36. Marchant DJ. Inflammation of the breast. Obstet Gynecol Clin North Am. 2002; 29:89–102. PMID:
11892876.

37. Dixey JJ, Shanson DC, Williams TD, Rustin MH, Crook SJ, Midgley J, et al. Toxic-shock syndrome: four cases in a London hospital. Br Med J (Clin Res Ed). 1982; 285:342–343.

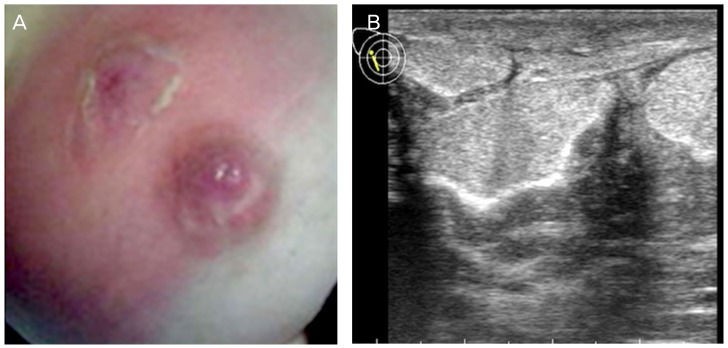
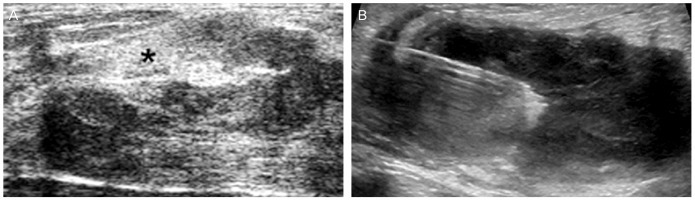
38. Karstrup S, Solvig J, Nolsoe CP, Nilsson P, Khattar S, Loren I, et al. Acute puerperal breast abscesses: US-guided drainage. Radiology. 1993; 188:807–809. PMID:
8351352.

39. Ulitzsch D, Nyman MK, Carlson RA. Breast abscess in lactating women: US-guided treatment. Radiology. 2004; 232:904–909. PMID:
15284435.

40. Eryilmaz R, Sahin M, Hakan Tekelioglu M, Daldal E. Management of lactational breast abscesses. Breast. 2005; 14:375–379. PMID:
16216739.

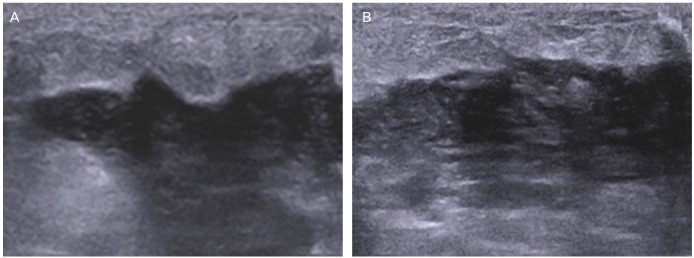
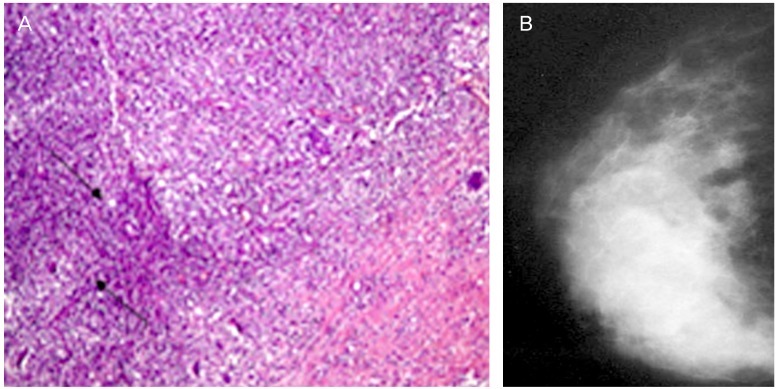
41. Memis A, Bilgen I, Ustun EE, Ozdemir N, Erhan Y, Kapkac M. Granulomatous mastitis: imaging findings with histopathologic correlation. Clin Radiol. 2002; 57:1001–1006. PMID:
12409111.

42. Yilmaz E, Lebe B, Usal C, Balci P. Mammographic and sonographic findings in the diagnosis of idiopathic granulomatous mastitis. Eur Radiol. 2001; 11:2236–2240. PMID:
11702165.

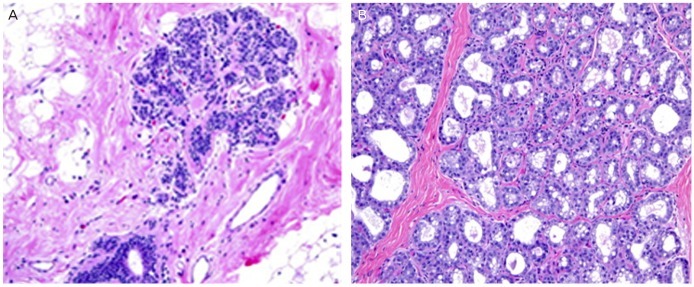
43. Han BK, Choe YH, Park JM, Moon WK, Ko YH, Yang JH, et al. Granulomatous mastitis: mammographic and sonographic appearances. AJR Am J Roentgenol. 1999; 173:317–320. PMID:
10430126.

44. Fletcher A, Magrath IM, Riddell RH, Talbot IC. Granulomatous mastitis: a report of seven cases. J Clin Pathol. 1982; 35:941–945. PMID:
6889612.

45. Asoglu O, Ozmen V, Karanlik H, Tunaci M, Cabioglu N, Igci A, et al. Feasibility of surgical management in patients with granulomatous mastitis. Breast J. 2005; 11:108–114. PMID:
15730456.

46. Tuncbilek N, Karakas HM, Okten OO. Imaging of granulomatous mastitis: assessment of three cases. Breast. 2004; 13:510–514. PMID:
15563860.

47. Lai EC, Chan WC, Ma TK, Tang AP, Poon CS, Leong HT. The role of conservative treatment in idiopathic granulomatous mastitis. Breast J. 2005; 11:454–456. PMID:
16297091.

48. Rosen PP. Breast tumors in children. In : Rosen PP, editor. Rosen's breast pathology. Philadelphia (PA): Lippincott-Raven;2001. p. 729–748.
49. Dehner LP, Hill DA, Deschryver K. Pathology of the breast in children, adolescents, and young adults. Semin Diagn Pathol. 1999; 16:235–247. PMID:
10490200.
50. Baker TP, Lenert JT, Parker J, Kemp B, Kushwaha A, Evans G, et al. Lactating adenoma: a diagnosis of exclusion. Breast J. 2001; 7:354–357. PMID:
11906446.

51. Saglam A, Can B. Coexistence of lactating adenoma and invasive ductal adenocarcinoma of the breast in a pregnant woman. J Clin Pathol. 2005; 58:87–89. PMID:
15623491.

52. Behrndt VS, Barbakoff D, Askin FB, Brem RF. Infarcted lactating adenoma presenting as a rapidly enlarging breast mass. AJR Am J Roentgenol. 1999; 173:933–935. PMID:
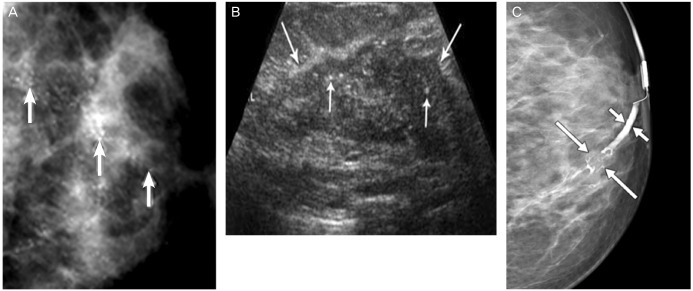
10511151.

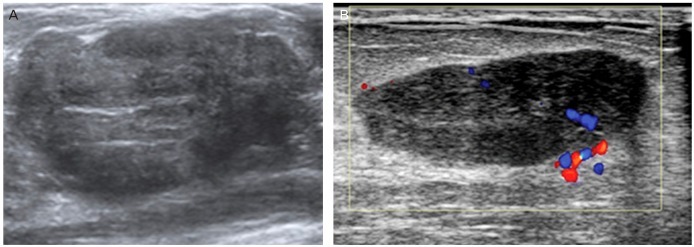
53. Sumkin JH, Perrone AM, Harris KM, Nath ME, Amortegui AJ, Weinstein BJ. Lactating adenoma: US features and literature review. Radiology. 1998; 206:271–274. PMID:
9423682.

54. Yang WT, Suen M, Metreweli C. Lactating adenoma of the breast: antepartum and postpartum sonographic and color Doppler imaging appearances with histopathologic correlation. J Ultrasound Med. 1997; 16:145–147. PMID:
9166808.

55. Darling ML, Smith DN, Rhei E, Denison CM, Lester SC, Meyer JE. Lactating adenoma: sonographic features. Breast J. 2000; 6:252–256. PMID:
11348374.

56. Rosen PP. Fibroepithelial neoplasms. In : Rosen PP, editor. Rosen's breast pathology. 2nd ed. Philadelphia (PA): Lippincott-Raven;2001. p. 163–200.
57. O'Hara MF, Page DL. Adenomas of the breast and ectopic breast under lactational influences. Hum Pathol. 1985; 16:707–712. PMID:
4007846.
58. Novotny DB, Maygarden SJ, Shermer RW, Frable WJ. Fine needle aspiration of benign and malignant breast masses associated with pregnancy. Acta Cytol. 1991; 35:676–686. PMID:
1659095.
59. Raju GC, Naraynsingh V. Infarction of fibroadenoma of the breast. J R Coll Surg Edinb. 1985; 30:162–163. PMID:
4045773.
60. Majmudar B, Rosales-Quintana S. Infarction of breast fibroadenomas during pregnancy. JAMA. 1975; 231:963–964. PMID:
1173104.

61. Jimenez JF, Ryals RO, Cohen C. Spontaneous breast infarction associated with pregnancy presenting as a palpable mass. J Surg Oncol. 1986; 32:174–178. PMID:
3736054.

62. Petrek JA, Theriault RL. Pregnancy-associated breast cancer and subsequent pregnancy in breast cancer survivors. In : Harris JR, Lippman ME, Morrow M, Osborne CK, editors. Diseases of the breast. 3rd ed. Philadelphia (PA): Lippincott Williams & Williams;2004. p. 1035–1046.
63. Ring AE, Smith IE, Ellis PA. Breast cancer and pregnancy. Ann Oncol. 2005; 16:1855–1860. PMID:
16030024.

64. Fuentes-Alburo A, Chavez-McGregor R, Ramirez Ugalde MT, De la Garza-Salazar JG. Early detection of breast cancer: who is responsible? 23rd Annual San Antonio Breast Cancer Symposium. Breast Cancer Res Treat. 2000; 64:abstract 205.
65. Chiechi LM, Lobascio A, Loizzi P. Breast cancer in pregnancy. Resistance to screening. Minerva Ginecol. 1998; 50:301–304. PMID:
9808953.
66. Nettleton J, Long J, Kuban D, Wu R, Shaefffer J, El-Mahdi A. Breast cancer during pregnancy: quantifying the risk of treatment delay. Obstet Gynecol. 1996; 87:414–418. PMID:
8598965.

67. Johannsson O, Loman N, Borg A, Olsson H. Pregnancy-associated breast cancer in BRCA1 and BRCA2 germline mutation carriers. Lancet. 1998; 352:1359–1360. PMID:
9802282.

68. Jernström H, Lerman C, Ghadirian P, Lynch HT, Weber B, Garber J, et al. Pregnancy and risk of early breast cancer in carriers of BRCA1 and BRCA2. Lancet. 1999; 354:1846–1850. PMID:
10584720.

69. Andrieu N, Goldgar DE, Easton DF, Rookus M, Brohet R, Antoniou AC, et al. Pregnancies, breast-feeding, and breast cancer risk in the International BRCA1/2 Carrier Cohort Study (IBCCS). J Natl Cancer Inst. 2006; 98:535–544. PMID:
16622123.
70. Cullins SL, Pridjian G, Sutherland CM. Goldenhar's syndrome associated with tamoxifen given to the mother during gestation. JAMA. 1994; 271:1905–1906. PMID:
8201729.







 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download