Abstract
Background
We sought to develop a novel index based on the skeletal muscle mass that reflects the change of quality of life (QOL), and is the most appropriate index for the body composition of the elderly in Korea. Whether lower extremity skeletal muscle mass index (LESMI) is an appropriate novel new index to diagnose patients with sarcopenia was also evaluated. A cut-off value for each index was reported to facilitate the diagnosis of patients with sarcopenia in a Korean population.
Methods
We used the 5th Korean National Health and Nutrition Examination Survey data from 2010. We analyzed 409 elderly patients, including 231 men and 178 women, aged ≥65 years. Patients were diagnosed by calculating their skeletal muscle index based on the skeletal muscle mass measured using dual energy X-ray absorptiometry. Obesity and osteoporosis were used to screen data and EuroQOL-5 dimension as a health questionnaire.
Results
The prevalence of sarcopenia in each index was obtained based on its cut-off value for diagnosing sarcopenia. There was a significant difference between the obesity rate of elderly patients diagnosed with sarcopenia and those who were not based on each index. There was no significant difference in the prevalence of osteoporosis between the groups. Sarcopenia diagnosis based on the LESMI was significantly correlated with QOL.
Sarcopenia is defined as the reduction of skeletal muscle mass below a certain level due to aging accompanied by a reduction in muscular strength and physical function; numerous studies have been conducted worldwide to determine its cause and treatment.[1] As economic costs increase due to the efforts to improve the welfare and quality of life (QOL) of the elderly, sarcopenia is gaining more attention following been assigned a disease classification code from the Health Statistics Center under the United States (US) Centers for Disease Control and Prevention in 2016.[23]
Since Rosenberg [4] first defined sarcopenia in 1997, various methods of measuring skeletal muscle mass have been developed along with a number of measuring skeletal muscle mass index (mSMI). Furthermore, as the importance of muscle strength and physical function has been emphasized in various studies, the European Working Group on Sarcopenia in Older People (EWGSOP) in 2010 introduced for the first time a diagnostic algorithm for sarcopenia based on walking speed, grip strength, and skeletal muscle mass.[1] In 2014, the Asian Working Group for Sarcopenia (AWGS) introduced a new sarcopenia diagnostic algorithm considering the differences in ethnicity, physical characteristics, and culture between European and Asian populations.[5] However, despite such efforts, diagnostic standards for sarcopenia and methods of measuring skeletal muscle mass are yet to be established. Thus, studies have reported varying prevalence rates for sarcopenia.
Marzetti et al.[6] reported that the skeletal muscle mass of the thigh was associated with walking ability, while Landi et al.[7] reported that the skeletal muscle mass of the calf was associated with physical strength and function. Moreover, various studies have reported that muscle strength or skeletal muscle mass of the lower extremities reflects the clinical significance of sarcopenia, such as a change in the QOL, physical disability, and risk of falls.[8] Based on this, ‘the following hypothesis was considered: Is it appropriate to diagnose sarcopenia based on the index using only the skeletal muscle mass of the lower extremities?’
Thus, the first purpose of this study was to identify the most suitable mSMI for the physical condition of Korean elderly patients that reflected the change in their QOL. The second purpose was to address the difficulty in diagnosing sarcopenia by setting a reference group using cut-off values based on young, healthy adults. Thus, the 5th Korea National Health and Nutrition Examination Survey (KNHANES V) data in 2010 were used to establish the reference group, and the cut-off values were suggested to diagnose sarcopenia more easily.
From the KNHANES V conducted by the Korea Center for Disease Control and Prevention, health survey and health examination data of 6,990 subjects sampled from January to December 2010 were used.[9] First, 1,352 elderly patients (567 men and 785 women) aged ≥65 years were selected in accordance with the screening criteria recommended by the AWGS. Among them, a total of 409 subjects (231 men and 178 women) were included after excluding subjects with diseases, such as cardiovascular diseases, internal diseases (i.e., cirrhosis, kidney failure, asthma, tuberculosis, thyroid diseases, and diabetes), various types of cancers, and other diseases, including arthritis, that can limit physical activity.
Currently, the most accurate method of measuring skeletal muscle mass is magnetic resonance imaging; however, there are limitations in using such for screening owing to economic issues and inconvenience of use.[10] DXA is a widely used method of measuring skeletal muscle mass for its reasonable cost and convenience of examination. Although it uses X-ray, the skeletal muscle mass of the upper and lower extremities, head, and body can be measured at low-dose levels.[11]
The status of obesity was categorized into three levels: (1) “underweight” for a body mass index (BMI) below 18.5 kg/m2; (2) “normal” for a BMI below 25.0 kg/m2; and (3) “obese” for a BMI of ≥25.0 kg/m2 based on the anthropometry data in the health examination. In this study, the underweight and normal weight groups were simplified as the “non-obese group” and compared with the “obese group.” Osteoporosis status was classified as “yes” or “no,” excluding surveys without examination data under the “osteoporosis diagnosis status” category. Based on the aforementioned data, the prevalence of osteoporosis and obesity based on the osteoporosis status was determined.
To evaluate QOL, the EQ-5D was used, which was developed in Europe to assess the QOL of patients with chronic diseases; it consists of five categories evaluating mobility, self-care, usual activity, pain / discomfort, and anxiety/depression. Each category is classified as “no problem,” “some problem,” or “a lot of problem.” In this study, each category was simplified as either “no problem” or “problem.” The EQ-5D index can be determined when the values of the five categories are weighted, and a value close to 1 indicates healthy living.[12]
Baumgartner et al.[13] defined appendicular skeletal muscle mass (ASM) by measuring the value using DXA and excluding the bone mass from the mass of the extremities, from which fat mass is already excluded. Janssen et al.[14] used bioelectrical impedance analysis to determine the ratio of skeletal muscle mass to the weight to use it as an index for the diagnosis of sarcopenia. Based on such, Lim et al.[15] determined the value of the skeletal muscle mass index (SMI; ASM [kg]/body weight [kg]×100) (%) by dividing the ASM measured using DXA by the weight for sarcopenia diagnosis. A study including Korean elderly subjects reported this method as a meaningful sarcopenia diagnostic tool that reflects the skeletal muscle mass of the extremities and BMI. Newman et al.[16] divided the ASM by the height and adjusted the increase in the ASM with an increasing height (ASM [kg]/height [Ht]2 [m]).
This study suggests a new SMI. Lower extremity skeletal muscle mass (LESM) was calculated using the values measured via the DXA; thereafter, this outcome was divided by the LESMI (LESM [kg]/lower extremity body weight [kg]×100) (%) and squared height (LESM [kg]/Ht2 [m]) to diagnose sarcopenia (Table 1).
From the KNHANES V, patients with cardiovascular diseases, internal diseases (i.e., cirrhosis, kidney failure, asthma, tuberculosis, thyroid diseases, and diabetes), various types of cancers, and diseases that limit mobility were excluded, and 1,753 patients were selected as the reference group. The mean and standard deviation of the SMI (%), ASM/Ht2, LESMI (%), and LESM/Ht2 of this group were determined, and the cut-off value was set as less than 1 in the diagnosis of sarcopenia for each index (Table 2).[15]
Using the original data from the National Health and Nutrition Examination Survey (NHANES), a composite sample analysis was conducted, including integrated weighting, variance estimation, and colony extraction variables, taking into account the weights of the surveyed areas and the proportion of the surveyed population by year. The cut-off values of the SMI (%), ASM/Ht2, LESMI (%), and LESM/Ht2 were set as the references in determining the prevalence of sarcopenia in the men and women, and the continuous variable was converted as a categorical variable, i.e., sarcopenia status. Based on the sarcopenia status, each variable was analyzed. For the categorical variable, the Rao-Scott χ2 test reflecting the composite sample and composite sample t-test for the continuous variable were used. IBM SPSS version 22.0 (IBM Corp., Armonk, NY, USA) was used, and a P-values of less than 0.05 was considered to indicate statistical significance. All results were presented as percentages or means.
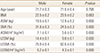
The mean age and BMI between the two groups classified by sex did not show a significant difference; conversely, the means of the indices associated with skeletal muscle mass showed significant differences maybe owing to the difference in the physical characteristics based on sex (Table 3).
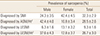
Based on the cut-off value set by the reference group, the prevalence of sarcopenia was 31.5% using the SMI, 28.4% using the ASM/Ht2, 9.8% using the LESMI, and 27.4% using the LESM/Ht2. After applying the total weight to the population diagnosed with sarcopenia based on each index, the prevalence of sarcopenia was 32.3±2.9% using the SMI, 28.5±2.6% using the ASM/Ht2, 9.3±1.6% using the LESMI, and 26.7±3.0 using the LESM/Ht2 (Table 4).
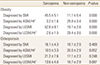
In the elderly patients diagnosed with sarcopenia based on the SMI as the index, 45.5±5.1% were obese; in the elderly patients not diagnosed with sarcopenia, 11.1±5.4% were obese, showing a significant difference in the prevalence of obesity based on sarcopenia diagnosis. When the LESMI was set as the index, the prevalence of obesity in the two groups based on sarcopenia diagnosis was 52.6±9.1% and 19.1±2.8%, respectively, showing a significant difference. Using the ASM/Ht2 and LESM/Ht2 as the indices, the prevalence of obesity based on sarcopenia diagnosis showed a reverse correlation, in which the patients without sarcopenia had a higher prevalence of obesity than those with sarcopenia. In the elderly patients with and without sarcopenia, the prevalence of osteoporosis showed a reverse correlation with the ASM/Ht2 as the index; the other indices did not show significant differences (Table 5).
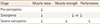
In the diagnosis of sarcopenia using the LESMI as the index and determination of the incidence of problems in the categories of the EQ-5D, a significant difference was observed in mobility, usual activity, pain/discomfort, and EQ-5D index. With the exception of the LESMI, the incidence of problems in the EQ-5D categories based on sarcopenia diagnosis using the SMI, ASM/Ht2, and LESM/Ht2 as the indices showed no significant difference (Table 6).
Previously, Chen et al.[5] attempted to establish the appropriate sarcopenia diagnosis criteria for the Asian populations via the AWGS. However, limitations included the data being weighted toward the Southeast Asian populations, and the different ethnicities of the Asian population restricted the establishment of representative sarcopenia diagnosis criteria despite such data being based on different mSMI and ages.[1718]
The purpose of the present study was to standardize the age and measuring tools based on the data obtained on DXA conducted on subjects older than 65 years as suggested by the AWGS and to determine which of SMI and ASM/Ht2 is more appropriate as mSMI for diagnosis of sarcopenia in Korean elderly. Based on the SMI, the prevalence of sarcopenia was 27.3% and 37.1% in men and women, with no significant differences in terms of sex; however, based on the ASM/Ht2, the prevalence of sarcopenia was 43.7% and 8.4% in men and women, respectively, which was significantly different. Kim et al.[19] reported that as Korean elderly women experienced dramatic industrialization, the increased height in the younger generation must be considered as it was the reference group for diagnosing sarcopenia using the ASM/Ht2 index; they also suggested that the difference in the mean height between the 20s and 80s was 14.5 cm. As this is a characteristic of Asian populations in general, including the Korean population, there are limitations in using the ASM/Ht2 as the index in evaluating sarcopenia in Asian populations.
Furthermore, among the elderly diagnosed with sarcopenia based on the SMI as the index, 45.5±5.1% were obese; among those without sarcopenia, the prevalence of obesity was 11.1±5.4%, showing a significant difference. Meanwhile, in the elderly diagnosed with sarcopenia based on the ASM/Ht2 as the index, 3.2±1.6% were obese; in those without sarcopenia, 29.3±3.4% were obese, showing a reverse correlation. Stenholm et al.[20] reported that obesity causes fat permeation in the skeletal muscle, reducing its quality and function and consequently highlighting the effect of obesity on the reduction of muscular mass. Tyrovolas et al.[21] reported that BMI and weight increase, while fat-free mass decreases, especially in elderly women after menopause, and that obesity in women affects sarcopenia. Zoico et al.[22] reported that using the SMI to diagnose sarcopenia is effective in screening sarcopenia in patients with a high fat mass, along with the association of the prevalence of insulin resistance and metabolic syndrome. Meanwhile, Newman et al.[16] reported an association between the prevalence of sarcopenia and obesity using the ASM/Ht2 as the index. Therefore, weight-adjusted SMI is a more appropriate mSMI than height-adjusted ASM/Ht2 in sarcopenia diagnosis among Korean elderly patients.
With regards to the association between the LESM and physical activity, Visser et al.[23] first reported in 1998 that there is no association between skeletal muscle mass of the extremities or lower extremities and physical disorder or activity and presented supporting evidence through their prospective study.[24] In 2011, a meta-analysis of 30 cohort studies confirmed no association between skeletal muscle mass of the lower extremities and physical activity disorder and instead reported that a weak lower extremity causes physical activity disorders, which has a close relationship with falls.[25] Bouchard and Janssen [26] also conducted a cross-sectional study using the NHANES data and confirmed that poor extremity strength and low skeletal muscle mass of the lower extremities had no correlation with physical disorders; however, they supported the correlation between lower extremity strength and physical function disorders by reporting that the correlation is no longer valid when patellar extension is adjusted.
Based on the abovementioned findings, does reduction of the LESM not induce physical activity disorders? The EWGSOP classifies three stages of sarcopenia as pre-sarcopenia, sarcopenia, and severe sarcopenia and suggests appropriate treatment and recovery goals for each stage. The EWGSOP also emphasized the need for well-designed studies for each stage (Table 7).[1] Elderly patients in the pre-sarcopenia stage, which only shows reduction in skeletal muscle mass, should be screened for appropriate treatment to slow down the progression to the sarcopenia stage, which is accompanied with an abnormal muscular strength, to prevent further physical disorders or falls. In this study, sarcopenia diagnosis based on the LESMI showed a significant correlation with the incidence of problems in mobility and usual activity and pain/discomfort and the EQ-5D index, which indicates that it better reflects the QOL than sarcopenia diagnosis based on the SMI, ASM/Ht2, and LESM/Ht2.
Therefore, the LESMI can be a useful index in the diagnosis of pre-sarcopenia and sarcopenia among Korean elderly patients, as it considers the skeletal muscle mass and BMI and reflects their QOL.
The limitations of this study were the inconclusive information on proving a causal relationship as it is based on the original data from the NHANES and that there may be several confounding variables not reflected. Next, the diagnostic criteria and measuring method of sarcopenia are still under discussion. Moreover, because categories evaluating muscular strength or physical function are not included in the original data, there are limitations in the analysis only based on the skeletal muscle mass. It is necessary to propose a well-designed prospective study on the appropriate index for sarcopenia diagnosis and the definition of the LESMI.
The LESMI can be utilized for diagnosing sarcopenia, as it is appropriate for the physical condition of Korean elderly patients and well reflects changes in their QOL. In addition, as this study presents the cut-off value needed for sarcopenia diagnosis, it will make such a diagnosis among Korean researchers more convenient.
Figures and Tables
References
1. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010; 39:412–423.

2. Cao L, Morley JE. Sarcopenia Is recognized as an independent condition by an international classification of disease, tenth revision, clinical modification (ICD-10-CM) code. J Am Med Dir Assoc. 2016; 17:675–677.

3. Park HM, Ha YC, Yoo JI, et al. Prevalence of sarcopenia adjusted body mass index in the Korean woman based on the Korean national health and nutritional examination surveys. J Bone Metab. 2016; 23:243–247.

5. Chen LK, Liu LK, Woo J, et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc. 2014; 15:95–101.

6. Marzetti E, Lees HA, Manini TM, et al. Skeletal muscle apoptotic signaling predicts thigh muscle volume and gait speed in community-dwelling older persons: an exploratory study. PLoS One. 2012; 7:e32829.

7. Landi F, Liperoti R, Russo A, et al. Sarcopenia as a risk factor for falls in elderly individuals: results from the ilSIRENTE study. Clin Nutr. 2012; 31:652–658.

9. Ministry of Health & Welfare, Korea Centers for Disease Control & Prevention. Korea health statistics 2011: Korea national health and nutrition examination survey (KNHANES V-2). Seoul: Ministry of Health & Welfare;2012.
10. Chien MY, Huang TY, Wu YT. Prevalence of sarcopenia estimated using a bioelectrical impedance analysis prediction equation in community-dwelling elderly people in Taiwan. J Am Geriatr Soc. 2008; 56:1710–1715.

11. Hong S, Choi WH. Clinical and physiopathological mechanism of sarcopenia. Korean J Med. 2012; 83:444–454.

12. Szende A, Oppe M, Devlin N. EQ-5D value sets: inventory, comparative review and user guide. Dordrecht, NL: Springer;2007.
13. Baumgartner RN, Koehler KM, Gallagher D, et al. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol. 1998; 147:755–763.

14. Janssen I, Heymsfield SB, Ross R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc. 2002; 50:889–896.

15. Lim S, Kim JH, Yoon JW, et al. Sarcopenic obesity: prevalence and association with metabolic syndrome in the Korean Longitudinal Study on Health and Aging (KLoSHA). Diabetes Care. 2010; 33:1652–1654.

16. Newman AB, Kupelian V, Visser M, et al. Sarcopenia: alternative definitions and associations with lower extremity function. J Am Geriatr Soc. 2003; 51:1602–1609.

17. Sanada K, Miyachi M, Tanimoto M, et al. A cross-sectional study of sarcopenia in Japanese men and women: reference values and association with cardiovascular risk factors. Eur J Appl Physiol. 2010; 110:57–65.

18. Lee WJ, Liu LK, Peng LN, et al. Comparisons of sarcopenia defined by IWGS and EWGSOP criteria among older people: results from the I-Lan longitudinal aging study. J Am Med Dir Assoc. 2013; 14:528.e1–528.e7.

19. Kim YS, Lee Y, Chung YS, et al. Prevalence of sarcopenia and sarcopenic obesity in the Korean population based on the Fourth Korean National Health and Nutritional Examination Surveys. J Gerontol A Biol Sci Med Sci. 2012; 67:1107–1113.

20. Stenholm S, Harris TB, Rantanen T, et al. Sarcopenic obesity: definition, cause and consequences. Curr Opin Clin Nutr Metab Care. 2008; 11:693–700.

21. Tyrovolas S, Koyanagi A, Olaya B, et al. Factors associated with skeletal muscle mass, sarcopenia, and sarcopenic obesity in older adults: a multi-continent study. J Cachexia Sarcopenia Muscle. 2016; 7:312–321.

22. Zoico E, Di Francesco V, Bissoli L, et al. Interrelationships between leptin resistance, body composition, and aging in elderly women. J Am Geriatr Soc. 2008; 56:1768–1769.

23. Visser M, Harris TB, Langlois J, et al. Body fat and skeletal muscle mass in relation to physical disability in very old men and women of the Framingham Heart Study. J Gerontol A Biol Sci Med Sci. 1998; 53:M214–M221.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download