Abstract
Background
Although osteoporosis is increasing medical issue in the elderly population, attempts to analyze the characteristics of patients diagnosed with osteoporosis are rare in South Korea. We investigated the characteristics of patients diagnosed with osteoporosis using Korea's National Health Insurance claims data, which includes almost Korean population.
Methods
We evaluated the patients who were diagnosed and treated with osteoporosis in medical institute in South Korea, using the national database by the Health Insurance Review & Assessment Service (HIRA). We evaluated the characteristic of patients and state of medical service utilization in 2010.
Results
The number of patients who were diagnosed with osteoporosis were 1,733,685, and almost of them (91.1%) were females. Fourteen point three percent of the patients had experienced osteoporosis-related fracture. The most commonly used type of institute and department was hospital and orthopedic surgery.
Conclusions
Considering increasing age population, basic information including characteristic of patients and current state of medical service utilization could be useful to perform appropriate management and treatment for osteoporosis patients in South Korea, using the National Health Insurance claims data.
Osteoporosis is a systematic skeletal disorder characterized by reduced bone mass and deterioration of bone architecture, resulting in the increased risks of fractures.[12] Recently, patients with osteoporosis are rapidly increasing while population aging is ongoing around the world.[3456] Several epidemiological studies have presented that osteoporosis and osteoporotic fracture are prevalent also in Asia.[78910]
South Korea is one of the fastest-aging societies, like as Japan and United States of America. The Korean population aged over 50 years will increase to 57% in 2050. [11] These mean that the proportion of the population at risk of osteoporosis will increase in South Korea.
Osteoporosis often silently progressed without symptom until fractures happen. Osteoporosis-related fracture results in significant disability, and mortality in elderly patients.[3456] People with osteoporosis hardly aware their sickness because it doesn't commonly involve symptoms, like as high blood pressure and diabetes. Epidemiological study on the characteristics of osteoporosis patients and the current state of medical service utilization has barely conducted in South Korea.
In order to develop policy well to manage the increased patients with osteoporosis, a comprehensive understanding of the characteristics of patients with osteoporosis and the situation of medical utilization takes priority over all others. Therefore, the purpose of this study was to analyze the characteristics of patients with osteoporosis and current state of medical utilization, based on the national database on information of medical utilization developed by the Health Insurance Review & Assessment Service (HIRA).
We used data from nationwide claims database of HIRA. More than 97% of Koreans, who are currently medical insurance subscribers, and the rest of 3% recipients of medical aid, are also included in this HIRA database. All health care providers submitted all the medical claims data for inpatients and outpatients care, including demographic information (age and gender), location (urban and rural), characteristics of healthcare provider, diagnoses using International Classification of Diseases, Tenth Revision (ICD-10) codes, type of health insurance, prescriptions records, procedures, and medical care costs, to obtain 70% reimbursement of the total medical cost from the government. The total rate of claims by electronic data processing has been reached more than 99% from the entire medical institution in South Korea since 2007. Thus, nearly all information about health care utilization can be obtained from this centralized database, except for those not covered by health insurance. Several epidemiologic studies have been published from this database in the field of osteoporosis.[121314151617]
We analyzed patients aged over 45 years who were diagnosed or treated with osteoporosis by physician between January 1, 2010 and December 31, 2010.
The date of first diagnosis was defined as the index date. We analyzed the data of medical service utilization of osteoporosis patients between the date of 2 years prior to the index date and the date of 1 year after index date. We excluded patients with a diagnosis of cancer or dementia. To analyze medical service utilization, the patients died within 2 years after diagnosis of osteoporosis were also excluded. Thus, the entire period that this study covered was from January 1, 2008 and December 31, 2012.
Because database from HIRA does not include the measurement of bone mineral density (BMD) using dual energy X-ray absorptiometry (DXA), we developed the operational definition of osteoporosis to identify patients with osteoporosis.[1417] To avoid misunderstanding, this study used the term of ‘osteoporosis-diagnosed patients’, because we could count only patients who diagnosed by doctor and paid their medical fee. Thus, the identified patients from the HIRA could be considered those who were diagnosed or treated for osteoporosis by doctors.
The operational definition for this study included those who were prescribed with medicine exclusively indicated only for osteoporosis, medicine indicated for other condition as well as osteoporosis after coding diagnostic disease for osteoporosis, and took measurement of DXA or bone turnover marker.[17]
On the basis of the national health insurance reimbursement coverage, the medicine indicated only for osteoporosis, and medicine indicated for other condition as well as osteoporosis were selected.[17]
Because some drugs may have various indications more than osteoporosis, among the patients with prescription of these drugs (estrogenic agents and calcium agents), only the patients with diagnostic code for osteoporosis (ICD-10 code, M80-82) was defined as osteoporosis patients determined by doctor. To avoid excessive overestimation due to duplication, we limited the case for outpatient only with at least twice ICD-10 code for osteoporosis diagnosis for 12 months, and for inpatient stayed more than 2 days.[17]
Previous osteoporotic fracture was evaluated for 2 years prior to the index date, by using the ICD-10 codes and procedure codes.[1819]
We evaluated the mainly used type of medical institute and department, presence of comorbidities including depression, alcoholism, and rheumatoid arthritis, disease related to secondary osteoporosis, use of drugs related drug-induced osteoporosis, and use of glucocorticoid steroid for at least 90 days during previous 1 year.[17]
Main medical institution and department meant the most used type of medical institute and department for 12 months after the index date.
The HIRA database includes four type of hospitals classified by bed size (clinics; <30 beds, hospitals; ≥30 to <100 beds, general; ≥100 beds, and tertiary hospitals; ≥300 beds).[16]
Continuous variables were summarized by means and standard deviations, while categorical variables were described by the number and percentage of patients. Data were analyzed using SAS software, version 9.2 (SAS Inc., Cary, NC, USA). This study was approved by the internal review board in HIRA, and the entire personal information used on this study was reconfigured as an unrecognizable form.
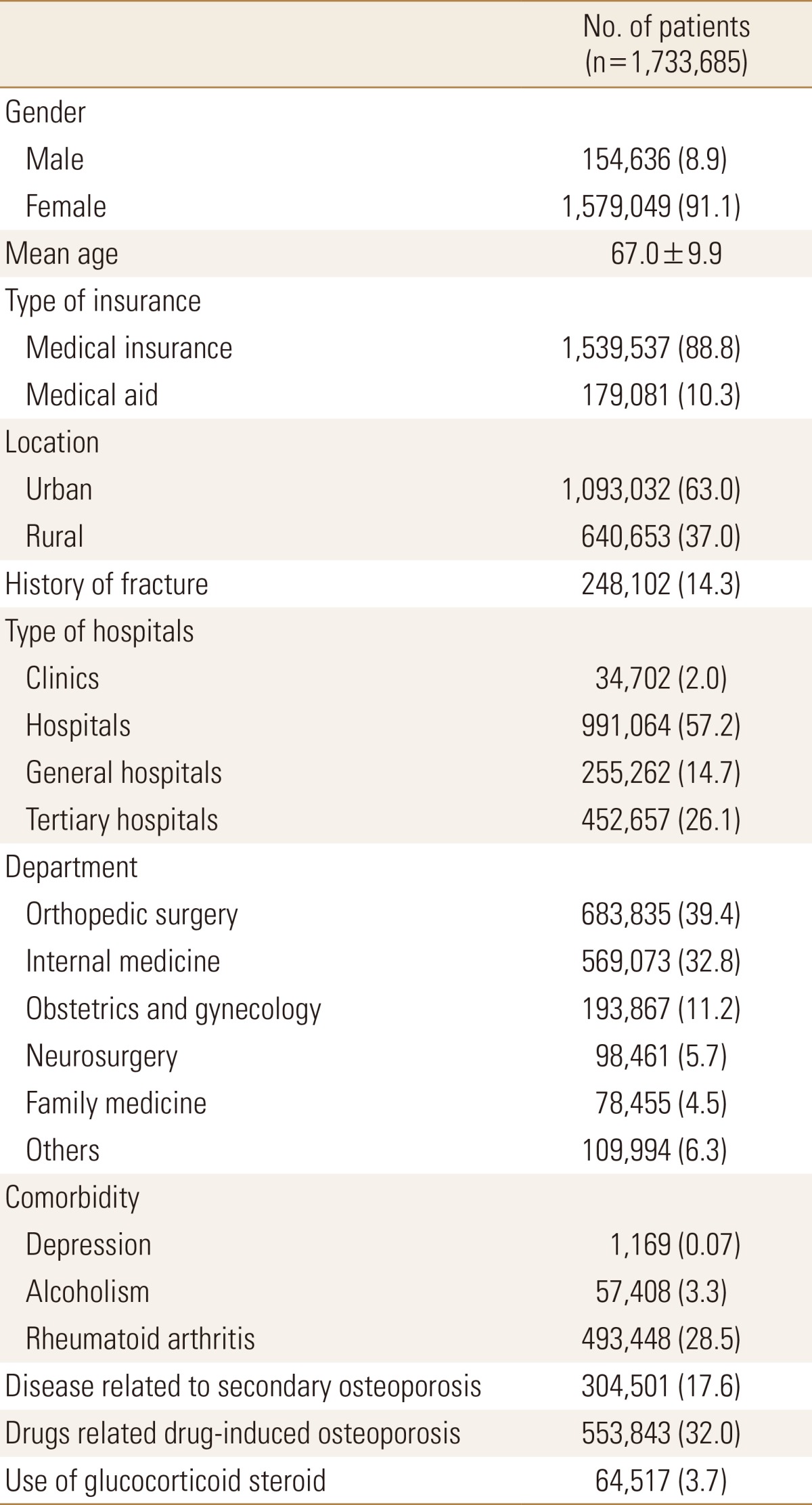
The number of osteoporosis patients aged over 45 diagnosed by doctor reached 1,733,685 in 2010, and among them, 91.1% was female patients (Table 1).
Among the osteoporosis-diagnosed patients, 14.3% experienced previously osteoporosis-related fractures. We analyzed the most used medical institution as primary used medical institution for 12 months after the first medical service. Patients mostly used hospital (57.2%), followed by tertiary hospital (26.1%), general hospital (14.7%), and local clinic (2%). Besides, the patients who were prescribed with drugs related drug-induced osteoporosis for more than 90 days were 32% during the last year, and the patients with disease related to secondary osteoporosis were 17.6% (Table 1).
This study presented the characteristics of osteoporosis-diagnosed patients and medical service utilization in South Korea, using the nationwide, cross-sectional cohort of the HIRA database.
In 2010, about 1,730,000 patients were identified as osteoporosis-diagnosed patients aged over 45. During study period, South Korea reimbursement guidelines for osteoporosis treatment required that patients had T-score of less than −3.0 or history of osteoporosis- related fracture at spine or hip, and covered a period of 6 months only.[20] Therefore, our results on the number of osteoporosis-diagnosed patients would be underestimate the real number of patients with osteoporosis. Moreover, just some patients would be visit the medical institute to diagnose and treat osteoporosis, because osteoporosis does not have any symptom until fracture.
According to the World Health Organization definition of osteoporosis (T-score ≤ −2.5), the prevalence of osteoporosis in Korea is 7.3% in males and 38.0% in females aged 50 years and older from the Korea National Health and Nutrition Examination Survey (KNHANSE).[21] When the prevalence from KNHANSE were adopted to the population in 2010, the number of real patients with osteoporosis could be estimated to be around 3,373,758 in Korean population of 50 years and older, by using the total number of men and women over the age of 50 in the Korean population.[22] This means that only about 51% (1,730,000/3,370,000) of patients with osteoporosis were diagnosed and treated in medical institute, although the age criteria were different between both studies. Considering increasing age population, the proportion of patients who were diagnosed and treated with osteoporosis remains still low.
Almost patients (91.1%) were female in this study. Understanding osteoporosis as a problem predominantly occurring in elderly women, our results can be also well understood. Inversely, our results might demonstrate that men with osteoporosis barely visit to medical institute to diagnose and treat osteoporosis.
Although medical aid covered just around 3% of Korean citizen, about 10% of patients diagnosed with osteoporosis were covered by medical aid. This means that medical aid might play an important role for patients with osteoporosis in South Korea.
Our study has a limitation. Database from HIRA does not include the measurement of BMD using DXA. But, we had to develop the operational definition of osteoporosis to identify patients with osteoporosis, named by “osteoporosis-diagnosed patients”.[1417]
Despite these limitations, the results of this study show that low proportion of patients with osteoporosis used medical institute to diagnose and treat osteoporosis in Korea. In terms of adequate management of osteoporosis, basic information including characteristic of patients and current state of medical service utilization could be useful.
ACKNOWLEDGEMENT
This research was supported by a grant of the Korea Health Technology R & D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HC15C1189 and HI13C1522).
References
1. Rapado I, Shulman LE, Fleisch HA, et al. Consensus development conference: diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med. 1993; 94:646–650. PMID: 8506892.
2. National Institutes of Health. NIH consensus development panel on osteoporosis prevention, diagnosis, and therapy, March 7-29, 2000: highlights of the conference. South Med J. 2001; 94:569–573. PMID: 11440324.
3. Reginster JY, Burlet N. Osteoporosis: a still increasing prevalence. Bone. 2006; 38:S4–S9. PMID: 16455317.

4. Johnell O, Kanis J. Epidemiology of osteoporotic fractures. Osteoporos Int. 2005; 16(Suppl 2):S3–S7. PMID: 15365697.

5. Borgström F, Sobocki P, Ström O, et al. The societal burden of osteoporosis in Sweden. Bone. 2007; 40:1602–1609. PMID: 17433804.

6. Delmas PD. Treatment of postmenopausal osteoporosis. Lancet. 2002; 359:2018–2026. PMID: 12076571.

7. Cooper C, Campion G, Melton LJ 3rd. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992; 2:285–289. PMID: 1421796.

8. Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997; 7:407–413. PMID: 9425497.

9. Lau EM, Lee JK, Suriwongpaisal P, et al. The incidence of hip fracture in four Asian countries: the Asian Osteoporosis Study (AOS). Osteoporos Int. 2001; 12:239–243. PMID: 11315243.

10. Hagino H, Katagiri H, Okano T, et al. Increasing incidence of hip fracture in Tottori Prefecture, Japan: trend from 1986 to 2001. Osteoporos Int. 2005; 16:1963–1968. PMID: 16133645.

11. Yoon HK, Park C, Jang S, et al. Incidence and mortality following hip fracture in Korea. J Korean Med Sci. 2011; 26:1087–1092. PMID: 21860561.

12. Seo GH, Lee YK, Ha YC. Risk of hip fractures in men with alpha-blockers: a nationwide study base on claim registry. J Bone Metab. 2015; 22:29–32. PMID: 25774362.

13. Seo GH, Choi HJ. Oral bisphosphonate and risk of esophageal cancer: a nationwide claim study. J Bone Metab. 2015; 22:77–81. PMID: 26082917.

14. Park C, Jang S, Lee A, et al. Incidence and mortality after proximal humerus fractures over 50 years of age in South Korea: national claim data from 2008 to 2012. J Bone Metab. 2015; 22:17–21. PMID: 25774360.

15. Kim SH, Ko YB, Lee YK, et al. National utilization of calcium supplements in patients with osteoporotic hip fracture in Korea. J Bone Metab. 2013; 20:99–103. PMID: 24524065.

16. Lee YK, Ha YC, Yoon BH, et al. National trends of hip arthroscopy in Korea. J Korean Med Sci. 2014; 29:277–280. PMID: 24550658.

17. Jang S, Park C, Jang S, et al. Medical service utilization with osteoporosis. Endocrinol Metab. 2010; 25:326–339.

18. Park C, Ha YC, Jang S, et al. The incidence and residual lifetime risk of osteoporosis-related fractures in Korea. J Bone Miner Metab. 2011; 29:744–751. PMID: 21644058.

19. Yoo JH, Moon SH, Ha YC, et al. Osteoporotic fracture: 2015 position statement of the Korean society for bone and mineral research. J Bone Metab. 2015; 22:175–181. PMID: 26713308.

20. Lee YK, Ha YC, Choi HJ, et al. Bisphosphonate use and subsequent hip fracture in South Korea. Osteoporos Int. 2013; 24:2887–2892. PMID: 23681088.

21. Park EJ, Joo IW, Jang MJ, et al. Prevalence of osteoporosis in the Korean population based on Korea National Health and Nutrition Examination Survey (KNHANES), 2008-2011. Yonsei Med J. 2014; 55:1049–1057. PMID: 24954336.

22. Ministry of Health & Welfare. Korea Centers for Disease Control & Prevention. Korea health statistics 2009: Korea national health and nutrition examination survey (KNHANES IV-3). Seoul: Ministry of Health & Welfare;2010.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download