This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Bone mineral density (BMD) is influenced by many factors. Despite the reported association between body components and BMD, most of these studies investigated the relationship between absolute muscle mass or fat mass and BMD in postmenopausal women or elderly subjects. The aim of this study is to investigate the association between muscle mass deficits (MMD) estimated from bioelectrical impedance analysis (BIA) and lumbar spinal BMD in Korean adults 20 to 49 years of age.
Methods
This cross-sectional study included 1,765 men and women who visited a health promotion center for a routine checkup. The lumbar spinal BMD was measured by dual energy X-ray absorptiometry. Body composition analysis was performed using BIA.
Results
The mean age of the subjects was 40.2±6.3 years. Ten thousand subjects (56.7%) were males and 126 subjects (7.1%) belonged to the low BMD (Z-score ≤-2.0). MMD had the strongest influence on BMD after adjusting for all covariates. The adjusted odds ratio of Group 3 (MDD >2.6 kg) for low BMD was 2.74 (95% CI, 1.46-5.15) after adjusting for age, gender, body mass index, height, and smoking.
Conclusions
MMD estimated by BIA showed a significant association with BMD and could be regarded as an independent risk factor for low BMD in adults 20 to 49 years of age. These findings support that interventions such as physical activity or lifestyle changes may simultaneously modify both muscle and bone health in this age group.
Keywords: Body mass index, Bone density, Muscles, Osteoporosis
INTRODUCTION
Osteoporosis is a disease of aging and there is a growing emphasis on prevention. Osteoporosis is a global public health problem that affects an enormous number of people and its prevalence will increase as the population ages. The consequences of osteoporosis include fractures and re-fractures, poor quality of life, excess mortality and morbidity, and large economic burden.
Factors maximizing peak bone mass during the growing period and delaying and slowing bone loss during menopause and old age may reduce fracture risk. Bone mineral density (BMD) is influenced by many factors such as age, gender, race, body weight or body mass index (BMI), lifestyle habits, hormonal status, and medical conditions or treatments. Among them, body weight or BMI is highly related to BMD.[
123] BMI also explains approximately 20% of the variance in BMD, which is one of the best determinants of BMD.[
4]
On the other hand, the relative contribution of lean mass and fat mass to BMD remains a contentious issue. Previous studies demonstrated significant associations between body components and BMD, and some of these associations were age specific. Lean mass was the main predictor of BMD in young and premenopausal women,[
56] whereas fat mass predicted BMD better than lean mass in elderly or postmenopausal women.[
78]
Despite the reported association between body components and BMD, most of these studies investigated the relationship between absolute muscle mass or fat mass and BMD in postmenopausal women or elderly subjects. The aim of this study is to investigate the association between muscle mass deficits (MMD) that are estimated from bioelectrical impedance analysis (BIA) and lumbar spinal BMD in Korean adults 20 to 49 years of age.
METHODS
1. Subjects
Data was gathered from 2,073 adults (1,010 males and 1,063 females) aged 20 to 49 years who had visited a health promotion center for periodic health examination between May 2012 and August 2012 at Eulji University Hospital. Among these subjects, we excluded subjects who met one of the following conditions: previous or current history of various types of cancer (n=32); hysterectomy (n=65); or a history of taking oral pills or hormone therapy (n=211). After these exclusions, 1,765 subjects (1,000 males and 675 females) were analyzed in the present study. This study was approved by the institutional review board of Eulji University Hospital.
2. Data collection and anthropometric measurements
All subjects completed a self-reported questionnaire regarding lifestyle related information, which includes cigarette smoking, alcohol consumption, and regular exercise habits. A detailed medical history and current medication use were collected through medical interviews. Alcohol consumption was defined as more than four drinks per day or more than eight drinks per week for women, and more than five drinks per day and more than fifteen drinks per week for men.[
9] A smoker was defined as a current smoker or an ex-smoker who had stopped within the last six months. Regular exercise was defined as twenty minutes or more per session at three times per week with high intensity exercise or thirty minutes or more per session at five times per week with low and moderate intensity exercise.
Height, weight and waist circumference were measured in subjects wearing a light robe and no shoes. BMI was calculated as the body weight (kg) divided by the height squared (m2). Blood samples were collected after an overnight fast (>12 hr) and analyzed within three hours after the sampling. Blood chemistry was measured by an enzymatic technique using an ADVIA 2400 analyzer (Siemens Healthcare Diagnostics, Deerfield, IL, USA). Serum 25-hydroxy-vitamin D (25-[OH]D) levels were measured by chemiluminescent immunoassay using a LIAISON analyzer (DiaSorin, Saluggia, Italy).
The lumbar spinal BMD was measured by dual energy X-ray absorptiometry (DXA; Lunar Prodigy, GE Lunar Corp., Madison, WI, USA). The BMD values were calculated as the means of measured values from L1-L4 except for the vertebrae affected by structural change due to collapse, surgery or degenerative disease, or internal artifacts. A vertebra was also excluded from the analysis if its T-score was more than 1 SD greater or less than that of the adjacent vertebra. The low BMD was defined as Z-score ≤-2.0.[
10]
BIA was performed using InBody 720 (Biospace Co., Ltd, Seoul, Korea) after voiding before the measurement. The subject stood on the footplate in their bare feet and held both hand electrodes. The screen automatically displays measurements of lean body mass (kg), skeletal muscle mass (kg), body fat mass (kg), and body fat percentage (%). The control of results' validity was done according to device specifications using the impedance values from the measurements at six frequencies displayed on the result sheet and invalid measurements were excluded from analysis.[
11] The MMD, which is the difference between the actual muscle mass and the optimal muscle mass, is the recommended change in muscle mass and is expressed as the muscle control (kg) on the results sheet.
3. Statistics
The subjects were divided into three groups according to the tertile of the MMD. Groups 1, 2, and 3 were defined as MMD=0 kg (no muscle deficit group), MMD ≤2.6 kg and MMD >2.6 kg, respectively. To compare the differences between the three groups, we used analysis of variance (ANOVA) with Scheffé's post-hoc test and chi-square tests for continuous and categorical variables, respectively. Multivariate linear regression analysis was performed to identify the major determinants of the lumbar spine BMD. In this model, the independent variables were those that had a significant relationship with the lumbar spine BMD in the partial correlation analysis. Weight, waist circumference and body fat mass were omitted because of interclass correlation with BMI. Logistic regression analyses were used to estimate the odds ratios for low BMD in each group. Finally, analysis of covariance (ANCOVA) was performed to compare the mean values of lumbar spine BMD between groups after adjusting for covariates. All statistical analyses were performed using SPSS statistical software (version 18.0; SPSS Inc., Chicago, IL, USA). A probability value of P<0.05 was considered significant.
RESULTS
1. General characteristics between MMD groups
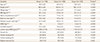
The mean ages of the 1,000 males (56.7%) and 765 females (43.3%) were 40.3±5.9 years and 40.0±6.6 years, respectively. One hundred twenty-six subjects (7.1%) belonged to the low BMD group. The mean MMD of Groups 2 and 3 were 1.3±0.7 kg and 5.0±1.9 kg, respectively (
P<0.001). Weight, BMI, waist circumference, body fat mass, skeletal muscle mass, and lumbar spine BMD were significantly different between the three groups (
P<0.001), and values decreased with increasing MMD. Serum 25-(OH)D levels showed significant difference only in Groups 1 and 3 (
P<0.001), and a higher level in Group 1 (
Table 1).
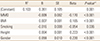
2. Major determinants of lumbar spine BMD
Lumbar spine BMD had a significant positive correlation with weight, skeletal muscle mass, BMI, waist circumference, body fat mass, and height after adjusting for age and gender (
P<0.001). In contrast, MMD was negatively correlated with the lumbar spine BMD (
P<0.001) (data not shown).
Table 2 shows that MMD had the strongest influence on the lumbar spine BMD when age, gender, and all other variables were included in the regression model. Moreover, BMI, smoking status, height, and gender were significantly associated with the lumbar spine BMD. Together, these variables explain up to 10.3% of the variation in the lumbar spine BMD.
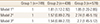
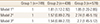
3. Odds ratios (95% CI) for low BMD according to the MMD groups
Table 3 shows the odds ratios for low BMD according to the MMD groups. The adjusted odds ratio of Group 3 for low BMD was 2.74 (95% CI, 1.46-5.15) after adjusting for age, gender, BMI, height, and smoking. This association was similar after adjusting for all other covariates including serum 25-(OH)D levels (OR 2.75; 95% CI, 1.45-5.12). The estimated means of lumbar spine BMD decreased with increasing MMD after adjusting for age, gender, smoking and BMI (
P<0.001) (
Fig. 1).
DISCUSSION
Bone mass is an important determinant of fracture risk in the elderly. Absolute bone mass is the sum of the cumulative rates of bone formation and bone loss. Therefore, strategies for accruing as much bone mass as possible over the first thirty years of life and slowing the rate of age-related bone loss are the first step for achieving optimal bone health and minimizing one's risk of osteoporotic fracture. Throughout life, BMD is influenced by many factors such as age, body weight or BMI, lifestyle habits, hormonal status, and medical conditions or treatments. Among them, body weight or BMI is highly related to BMD in various populations [
12312] and maintaining a healthy body weight is important for bone health throughout life.
Body weight is largely made up of two components: fat mass and lean mass. The relative contribution of these two components to the variation in BMD remains a contentious issue. Previous studies have demonstrated significant associations between body components and BMD, and some of these associations were age specific. Lean mass was the main predictor of BMD in young and premenopausal women,[
56] whereas fat mass predicted BMD better than lean mass in older or postmenopausal women.[
78] Despite the reported association between body components and BMD, most of these studies investigated the relationship between absolute muscle mass or fat mass measured by DXA and BMD in postmenopausal women or elderly subjects. However, these results have limitations for use in clinical practice.
We investigated the relationship between muscle and BMD using MMD estimated from BIA. BIA is a less expensive, timesaving, convenient, and easily accessible modality in an outpatient clinic setting when compared with other modalities. BIA is based on the capacity of hydrated tissues, which assumes that total body water is constant. From total body water, validated equations allow the calculation of fat free mass and fat mass.[
13] For the analysis of the body composition, BIA has been shown to have good correlation with DXA.[
14] MMD is the difference between the actual muscle mass and the optimal muscle mass, which is estimated from target weight, and the recommended change in muscle mass. MMD is displayed as muscle control (kg) on the results sheet. Thus, the results are easily applicable to clinical practice.
In this study, MMD, BMI, smoking status, height, and gender were major independent variables associated with lumbar spine BMD in adults aged 20 to 49 years and MMD, not absolute skeletal muscle mass, had the strongest influence on the lumbar spine BMD after adjusting for all covariates. In addition, adjusted means of lumbar spine BMD decreased progressively with increasing MMD. These results suggest that MMD estimated from BIA might be used as a screening tool in a clinical setting to identify people with risk of low BMD. Furthermore, as BMD and MMD are negatively related, interventions intended to improve muscle mass would concurrently improve BMD.
Changes in muscle and bone mass brought about by exercise or aging are also tightly correlated in both human and experimental animal models.[
15] It has been widely assumed that the coordination of muscle and bone mass occurs through muscle force-generated mechanical signals, which transduce anabolic activity in the adjacent bone.[
16] The shared mesodermal origin of muscle and bone presents the additional possibility that common molecule networks serve to coordinate their mass.[
17181920] Many of the studies suggest a dominant role of muscle over bone in synchronizing the mass of these two tissues, at least in postnatal life.[
14]
Our study has several limitations. First, we could not verify the causality between MMD and lumbar spine BMD in this cross-sectional study. Second, we cannot rule out selection bias in our subjects who had visited a health promotion center. Therefore, study subjects may not represent the entire Korean population. Third, detailed assessment of current and past activities of subjects could not be confirmed. Finally, analyses performed only on lumbar spine BMD data, could have biased the results as the proportions of trabecular and cortical components are different according to the measured bone. Despite such limitations, our study is the first to show the consistently significant association between MMD, as assessed by BIA, with lumbar spine BMD emphasizing the importance of MMD on low BMD.
In conclusion, MMD estimated by BIA showed a significant association with lumbar spine BMD and could be regarded as an independent risk factor for low BMD in Korean adults 20 to 49 years of age. These findings support that interventions such as physical activity or lifestyle changes may simultaneously modify both muscle and bone health in this age group.
Figures and Tables
Fig. 1
Adjusted mean values of lumbar spinal BMD according to MMD groups. Bars mean standard errors. a)Adjusted for age, gender, smoking, and BMI. b)Group 1 is defined as MMD=0 kg, Group 2 is defined as 0 kg<MMD≤2.6 kg, Group 3 is defined as MMD>2.6 kg. BMD, bone mineral density; MMD, muscle mass deficit.

Table 1
General characteristics between muscle mass deficits groupsa)
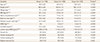
Table 2
Multivariate regression analyses with lumbar spine bone mineral density as a dependent variable
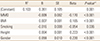
Table 3
Odds ratios (95% confidence interval) for low bone mineral density (Z-score ≤-2.0) according to muscle mass deficits groupsa)





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download