Abstract
Isolated hypogonadotropic hypogonadism (IHH) is known to decrease bone mineral density due to deficiency of sex steroid hormone. Graves' disease is also an important cause of secondary osteoporosis. However, IHH does not preclude the development of primary hyperthyroidism caused by Graves' disease, leading to more severe osteoporosis rapidly. Here, we describe the first case of 35-year-old Asian female patient with IHH accompanied by Graves' disease and osteoporosis-induced multiple fractures. Endocrine laboratory findings revealed preserved anterior pituitary functions except for secretion of gonadotropins and showed primary hyperthyroidism with positive autoantibodies. Sella magnetic resonance imaging showed slightly small sized pituitary gland without mass lesion. Dual energy X-ray absorptiometry revealed severe osteoporosis in lumbar spine and femur neck of the patient. Plain film radiography of the pelvis and shoulder revealed a displaced and nondisplaced fracture, respectively. After surgical fixation with screws for the femoral fracture, the patient was treated with antithyroid medication, calcium, and vitamin D until now and has been recovering fairly well. We report a patient of IHH with Graves' disease and multiple fractures that is a first case in Korea.
Isolated hypogonadotropic hypogonadism (IHH) is characterized by impairment of gonadal function secondary to deficient gonadotropin secretion.[1] It can result from a variety of congenital, acquired, and functional defects related to gonadotropin releasing hormone (GnRH) deficiency. In general, IHH is caused by genetic mutation or acquired anatomical abnormalities including infiltrative disorders or space-occupying tumors involving the hypothalamic-pituitary axis, subsequently promoting deficiency of sex hormones.[23]
Sex steroid hormones are important factors in bone mineral dynamics and play an essential role in the pathogenesis of osteoporosis. There have been many investigations of the links between sex hormone status and bone mineral density (BMD) for various clinical conditions. In renal transplant recipients, serum levels of estradiol predict BMD in women.[4] Estrogens also play a pivotal role in the regulation of bone loss and metabolism in elderly men.[5]
Maintenance of proper BMD requires not only sex steroid hormones but also thyroid hormones and vitamin D. Moreover, abnormal status of thyroid hormone or lower levels of vitamin D can promote pathologic or non-trauma induced fractures.[6789] Although abnormal thyroid hormonal status is rare in patients with IHH, IHH accompanied by primary or secondary hypothyroidism including bradycardia and heart failure was recently reported.[10] However, to our best knowledge, there has been no report of IHH associated with Graves' disease. Therefore, we herein report a rare case of IHH accompanied by multiple fractures due to thyrotoxicosis and sex steroid hormone deficiency.
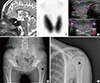
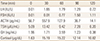
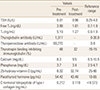
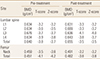
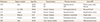
A 35-year-old Asian woman, born from non-consanguineous parents, was referred to the department of endocrinology for evaluation of a patient with multiple fragility fractures, and severe osteoporosis accompanied by diffuse goiter. The patient was an ex-smoker and non-drinker. She was 1.71 m tall and weighed 51.2 kg with a body mass index (BMI) of 17.5 kg/m2. The diagnosis of IHH was established by suggestive clinical findings with primary amenorrhea and absence of growth and development of secondary sexual characteristics and laboratory findings at 16 years. The patient had no facial anomaly or olfactory complaints. No familial history of anosmia, delayed puberty or hypogonadism was reported by the patient. The karyotype was 46XX and genetic screening for mutations in the hypogonadotropic hypogonadism genes was not performed. At that time, anterior pituitary function was preserved except for gonadotropin secretion. The patient has been treated with estrogen replacement since she was 16 years old, but she was taken off estrogen by herself several years ago. Sella magnetic resonance imaging scan revealed a small sized pituitary gland without mass-like lesion and thinning of the lower half of the pituitary stalk (Fig. 1A). In the combined pituitary stimulation test at 28 years old, the peak luteinizing hormone (LH) was 1.79 IU/L and peak follicle stimulating hormone (FSH) was 1.50 IU/L, suggesting hypogonadotropic hypogonadism (Table 1). In the recent visit, the patient's blood pressure was 130/82 mmHg and her heart rate was 98 beats/min. On laboratory examination, complete blood count revealed hemoglobin: 12.3 g/dL; leukocyte count: 4.9×109/L; and platelet: 313×109/L. Serum levels of total cholesterol (207 mg/dL), triglyceride (85 mg/dL), albumin (5.0 g/dL), aspartate transaminase (AST; 22 IU/L), and alanine aminotransferase (ALT; 20 IU/L) were all within normal range. The levels of basal LH, FSH and estradiol were 0.25 IU/L (range, follicular 0.6-6.2; mid-cycle 12-51; luteal 0.0-6.0), 0.23 IU/L (range, follicular 3.3-8.8; mid-cycle 5.4-20; luteal 1.6-8.7), and 10 pg/mL (range, follicular 21-251; mid-cycle 38-649; luteal 21-312), respectively. Symptoms and sign of thyrotoxicosis including tachycardia, smooth skin, and goiter were also developed in the patient. A Technetium-99m (Tc-99m) pertechnetate scintigraphy revealed diffuse enlargement of both lobes of the thyroid gland with markedly increased uptake (Fig. 1B). A thyroid function test showed newly developed primary hyperthyroidism in the patient (Table 2). Moreover, the level of thyrotropin binding inhibiting immunoglobulin was also increased (Table 2). Neck ultrasonography showed an enlarged heterogeneous echogenic thyroid gland with increased vascularity determined by the color doppler method (Fig. 1C). Serum 25-hydroxy-vitamin D level was also decreased in the patient. The antero-posterior pelvic X-ray showed left proximal femoral fracture (Fig. 1D) and shoulder X-ray revealed a non-displaced proximal humeral fracture (Fig. 1E). BMD was measured at the lumbar spine and femoral neck of the patient using dual energy X-ray absorptiometry. The patient had significantly lower BMD at both lumbar spine and femur neck (Table 3). She was treated with conservative management for humeral fracture and received surgical fixation with screws for the left femoral fracture. The patient was also treated with methimazole, estrogen replacement, calcium, and vitamin D for two years, thereby leading to 2.34% and 6.97% increase in BMD of lumbar spine and femur neck, respectively (Table 3). She was maintained in an euthyroid state with 2.5 to 5.0 mg of methimazole per day and has been recovering fairly well with estrogen replacement and treatment of calcium and vitamin D 2,000 IU per day for six months (Table 2).
In general, IHH presents as decreased ovarian function leading to menstrual defect, diminished vaginal secretion, infertility, and impaired breast development in premenopausal woman. In this case report, we presented IHH accompanied by Graves' disease and multiple fractures. To our best knowledge, this case report is the first paper describing severe osteoporosis-induced bone fracture in a patient with IHH accompanied by Graves' disease.
Pituitary hormone deficiencies causing hypogonadism, hypothyroidism, or hypoadrenalism may induce lower BMD.[11] People with IHH are also prone to develop osteoporosis or fragile bones leading to higher risk of fractures induced by otherwise minor injuries.[9] Although the mechanisms underlying the relationship between central hypogonadism and BMD have not yet been determined, unreplaced sex steroid deficiency is associated with lower BMD in adults with growth hormone deficiency.[912] Therefore, cyclical replacement of estrogen and progesterone is recommended to prevent premature osteoporosis and to promote sexual characteristics in premenopausal women. In addition, testosterone treatment was also effective for increasing lumbar spine BMD in hypogonadal middle-aged men.[1314]
IHH is rarely accompanied by central hypothyroidism due to structural abnormalities of the hypothalamic-pituitary axis.[10] Thyroid-stimulating hormone (TSH) is critical for regulating expression of sodium-iodide symporter which is important for the production of thyroid hormone in the thyroid gland. In the pre-specified subgroup of premenopausal-aged women, TSH deficiency is independently related to lower BMD in the lumbar spine and femur neck.[9] However, Graves' disease or excessive replacements of thyroid hormone are also known as risk factors of osteoporosis.[7] Graves' disease promotes bone loss by increased bone turnover, leading to decreased BMD and osteoporosis.[7] On the other hand, vitamin D deficiency is also an important risk factor for osteoporosis and increased risk of pathologic fractures in adults.[6815] Therefore, we thought that low levels of vitamin D as well as inappropriate estrogen replacement with Graves' disease might be contributing to aggravation of the osteoporosis and development of fractures in the patient.
Although the co-occurrence of hypopituitarism and Graves' disease are rare, several reports have been described in the literature (Table 4). A patient with hyperthyroidism in the presence of panhypopituitarism developed a radioiodine-induced thyroid storm.[16] Graves' disease developed eight years after the diagnosis of hypopituitarism in this case. In another case, a 24-year-old male patient presented with hypopituitarism accompanied by hyperthyroidism and diabetes insipidus was described in 1999.[17] A third report described cases of concomitant Graves' disease and Sheehan's syndrome.[18] A more recent report described that a subject with known panhypopitutarism developed thyrotoxicosis that contributed to acute glucocorticoid deficiency.[19] Another report showed that it was possible for hyperthyroidism secondary to toxic thyroid nodule, to occur with hypopituitarism.[20] However, our case is IHH rather than panhypopituitarism, and the patient presented with multiple osteoporosis-induced fractures associated with Graves' disease.
In conclusion, herein we report a case of IHH with Graves' disease and multiple fractures. Sex hormone, calcium, and vitamin D replacement are essential for prevention of osteoporosis in patients with IHH. Secondary osteoporosis-inducible factors including hyperthyroidism should also be considered in patients with fragility fracture accompanied by IHH.
Figures and Tables
Fig. 1
Image findings of the patient. (A) Mid-sagittal T2-weighted image showing thinning of the lower half of the pituitary stalk (arrow). (B) Technetium-99m pertechnetate scintigraphy for thyroid gland. Radioactive thyroid uptake was 8.9% (range, 1.7 to 4.0%). (C) Thyroid ultrasonography with color doppler method (upper panel, right thyroid; lower panel, left thyroid). (D) Antero-posterior X-ray of the pelvis demonstrating a fracture of the left femoral neck (arrow head). (E) Antero-posterior radiograph of the left shoulder showing nondisplaced fracture of proximal humerus (arrow head).
References
1. Seminara SB, Hayes FJ, Crowley WF Jr. Gonadotropin-releasing hormone deficiency in the human (idiopathic hypogonadotropic hypogonadism and Kallmann's syndrome): pathophysiological and genetic considerations. Endocr Rev. 1998; 19:521–539.

2. Silveira LF, Latronico AC. Approach to the patient with hypogonadotropic hypogonadism. J Clin Endocrinol Metab. 2013; 98:1781–1788.

3. Buck C, Balasubramanian R, Crowley WF Jr. Isolated gonadotropin-releasing hormone (GnRH) deficiency. In : Pagon RA, Adam MP, Ardinger HH, editors. GeneReviews®. Seattle: University of Washington;1993.
4. Cueto-Manzano AM, Freemont AJ, Adams JE, et al. Association of sex hormone status with the bone loss of renal transplant patients. Nephrol Dial Transplant. 2001; 16:1245–1250.

5. Gennari L, Merlotti D, Martini G, et al. Longitudinal association between sex hormone levels, bone loss, and bone turnover in elderly men. J Clin Endocrinol Metab. 2003; 88:5327–5333.

6. Bakhtiyarova S, Lesnyak O, Kyznesova N, et al. Vitamin D status among patients with hip fracture and elderly control subjects in Yekaterinburg, Russia. Osteoporos Int. 2006; 17:441–446.

7. Greenspan SL, Greenspan FS. The effect of thyroid hormone on skeletal integrity. Ann Intern Med. 1999; 130:750–758.

8. Larsen ER, Mosekilde L, Foldspang A. Vitamin D and calcium supplementation prevents osteoporotic fractures in elderly community dwelling residents: a pragmatic population-based 3-year intervention study. J Bone Miner Res. 2004; 19:370–378.

9. Tritos NA, Greenspan SL, King D, et al. Unreplaced sex steroid deficiency, corticotropin deficiency, and lower IGF-I are associated with lower bone mineral density in adults with growth hormone deficiency: a KIMS database analysis. J Clin Endocrinol Metab. 2011; 96:1516–1523.

10. Passeri E, Bonomi M, Dangelo F, et al. Wasting syndrome with deep bradycardia as presenting manifestation of long-standing severe male hypogonadotropic hypogonadism: a case series. BMC Endocr Disord. 2014; 14:78.

11. Bolanowski M, Halupczok J, Jawiarczyk-Przybylowska A. Pituitary disorders and osteoporosis. Int J Endocrinol. 2015; 2015:206853.

12. Venken K, Callewaert F, Boonen S, et al. Sex hormones, their receptors and bone health. Osteoporos Int. 2008; 19:1517–1525.

13. Kim SH. Testosterone replacement therapy and bone mineral density in men with hypogonadism. Endocrinol Metab. 2014; 29:30–32.

14. Lee MJ, Ryu HK, An SY, et al. Testosterone replacement and bone mineral density in male pituitary tumor patients. Endocrinol Metab. 2014; 29:48–53.

15. Song HR, Kweon SS, Choi JS, et al. High prevalence of vitamin D deficiency in adults aged 50 years and older in Gwangju, Korea: the Dong-gu Study. J Korean Med Sci. 2014; 29:149–152.

16. Krishnamurthy GT, Blahd WH. Case reports. Hyperthyroidism in the presence of panhypopituitarism. Thyroid crisis and hypothyroidism following radioiodine treatment. West J Med. 1974; 120:491–496.
17. Wada S, Kurihara S, Imamaki K, et al. Hypercalcemia accompanied by hypothalamic hypopituitarism, central diabetes inspidus and hyperthyroidism. Intern Med. 1999; 38:486–490.

18. Arpaci D, Cuhaci N, Saglam F, et al. Sheehan's syndrome co-existing with Graves' disease. Niger J Clin Pract. 2014; 17:662–665.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download