Abstract
Background
Alpha-blocker can result in falling and fractures because of adverse effect such as orthostatic hypotension due to vasodilatory effect. We investigated the association between the alpha-blocker and the risk of osteoporotic hip fractures using a nationwide claim database.
Methods
We identified 1,051,651 men 65 years of age or older who had prescription records of alpha-blocker from nationwide medical claim database, from 2007 to 2012. Alpha-blockers were classified as non-specific general (NSG), non-specific slow-release (NSSR), uro-specific general (USG), and uro-specific slow release (USSR).
Benign prostatic hyperplasia is a common disease with its prevalence reaching over 60% of men older than 65 years,[1] and alpha-blocker is most useful and the first line drug to manage urinary symptom in elderly men with benign prostatic hyperplasia.[2] But, alpha-blocker has adverse effect such as orthostatic hypotension, headache and dizziness due to vasodilatory effect.[3] On the other hands, syncope and falling followed by fracture are rare after alpha-blocker, even though vasodilation-associated effects also might result in.[3]
Several studies on antihypertensive drugs suggested that the antihypertensive drugs can cause orthostatic hypotension, which has been well-known risk factor for falling and fractures, in elderly patients.[4,5] Interestingly, among antihypertensive drugs, alpha-blockers have been reported to be strongly associated with orthostatic hypotension and syncope.[4,5,6] But, there has been rare study on the association between the alpha-blocker and the risk of osteoporotic hip fractures.
The purpose of this study was to investigate the association between the alpha-blocker and the risk of osteoporotic hip fractures using a nationwide claim database.
We analyzed data from a nationwide claim database, the Health Insurance Review and Assessment Service (HIRA) of South Korea. The HIRA database covered over 99.9% of all medical and pharmacy claims in South Korea. The HIRA database includes diagnosis (recorded by the International Classification of Diseases, 10th revision [ICD-10]), procedure records, prescription records (drug name, formula, dose, and duration of prescription), and demographic information.[7,8,9,10,11,12] The study protocol was approved by the institutional review boards. All nationwide claim data of HIRA database were analyzed to define prescription records of alpha-blocker medication and hip fracture from January 2007 to December 2012.
We examined men 65 years of age or older who had prescription records of alpha-blocker from January 2007 to June 2012. The first prescription date was set as the index date. We included only the new users of alpha-blocker by excluding subjects who had a prescription records for alpha-blockers in the prior 365 days from the index date. We also excluded subjects who had a hip fracture in the prior 365 days from the index date.
Alpha-blockers were classified based on uro-specificity and slow-release; non-specific general (NSG; for example; Doxazosin, Terazosin), non-specific slow-release (NSSR; for example: Doxazosin), uro-specific general (USG; for example: Silodosin, Tamsulosin, Naftopidil), and uro-specific slow release (USSR; for example: Alfuzosin, Tamsulosin). If an individual changed alpha-blocker to another type of alpha-blocker, each medication was considered as the first prescription. Discontinuation was defined by either the absence of ongoing refills or a continuous gap of 30 days or more between an expected refill and actual refill during the 360 days study period.[13]
To identify hip fracture, we used the selected codes for 7 procedures (open reduction of fractured extremity-femur, closed pinning-femur, external fixation-pelvis/femur, closed reduction of fractured extremity-pelvis/femur, bone traction, skin traction, hemiarthroplasty-hip), which were used for hip fracture.[7,8,14] When an individual had more than two procedure codes, the date of the first encoding was considered as the date of occurrence of hip fracture.
We analyzed the incidence of hip fracture within 1 year after medication of alpha-blocker. We calculated hazard ratios (HRs) of hip fracture within 15 days, 16 to 30 days, 31 to 45 days, 46 to 90 days, 91 to 180 days, and 181 to 360 days after index date. Non-using periods, between 180 and 360 days prior to index date, in each type of alpha-blocker users were chosen as the reference group, and HRs were calculated by using Cox proportional hazard model.
Statistical results were presented with 95% confidence intervals (CIs). If 95% CI did not include 1.0, it meant that the results were statistically significant. R package (version 2.15.3) was used for all statistical calculations.
From the national claims database between January 2007 and December 2012, 4,615,626 eligible subjects with alpha-blockers were identified. Among them, 2,391,842 subjects were new users of alpha-blockers (no evidence of previous alpha-blockers). Thereafter, we excluded subjects with previous hip fracture history and discontinuation of alpha-blocker. Finally, 1,051,651 subjects with alpha-blockers were analyzed in this study.
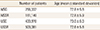
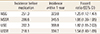
The baseline characteristics of the study cohort are shown in Table 1.
Total of 6,553 hip fractures were observed during the observation period. The incidences of hip fracture within 1 year and HR were shown in Table 2.
In this nationwide study, we found that use of alpha-blockers is associated with increased risk of hip fracture. To our knowledge, this is the largest study with longest observation period (up to five years) investigating the association between use of alpha-blockers and risk of hip fracture.
The present study showed that use of alpha-blockers was associated with higher risk of hip fracture. This is consistent with previous studies, which demonstrated that use of alpha-blockers was associated with an increased risk of fracture.[3,4,5] But, alpha-blocker was not the primary objects of the studies, but secondary, because they included alpha-blocker as one of antihypertensive medication.[4,5]
Although we did not evaluate the mechanism of alpha-blocker on risk of fracture, orthostatic hypotension and syncope by vasodilatory adverse effects have been suggested as possible mechanism that alpha-blockers could increase the risk of falling and fracture.[3,15]
In this study, HRs of uro-selective drug seems higher than those of non-selective drug, which was discrepant with expectation on lower risk of orthostatic hypotension in uro-selective drugs. However, we cannot compare directly HR with each other in this study, because we calculated HR by comparing with non-using reference periods in each type of alpha-blocker user.
However, our study might provide more important clinical implication, because we showed the risk of hip fracture according to the time after use of alpha-blocker (Fig. 1). The risk of hip fracture peaked early period after use of alpha-blocker, and decreased with time. This means that physicians should be cautious in early period when they use alpha-blocker.
Our study has several limitations. First, we did not include other factors for fall and fractures, age, gender, bone mineral density, diagnosis of osteoporosis, osteoporosis-related medication, and other medical comorbidity. Second, we did not evaluate doses of alpha-blocker, which would be important vasodilatory side-effect. Thirds, we could not differentiate the osteoporotic fracture from fracture due to high-energy trauma. Fourth, we could not evaluate the proportion of orthostatic hypotension in alpha-blocker users, because we used de-identified database. Fifth, among the used procedure codes, that for hemiarthroplasty was not exclusive for hip fracture. But, its utilization for other conditions was negligible.
In spite of these limitations, this study showed that use of alpha-blocker is associated with increased risk of hip fracture, especially in early period. Physician should be remember possibility of orthostatic hypotension followed by falling and fracture, especially in the early period, when they used alpha-blocker in the elderly patients.
Figures and Tables
Fig. 1
Hazard ratio of hip fracture after use of alpha-blocker in each type of alpha-blocker. NSG, non-specific general; NSSR, non-specific slow-release; USG, non-specific slow-release; USSR, uro-specific slow release.

References
1. Arrighi HM, Metter EJ, Guess HA, et al. Natural history of benign prostatic hyperplasia and risk of prostatectomy. The Baltimore Longitudinal Study of Aging. Urology. 1991; 38:4–8.

2. McVary KT, Roehrborn CG, Avins AL, et al. Update on AUA guideline on the management of benign prostatic hyperplasia. J Urol. 2011; 185:1793–1803.

3. Chrischilles E, Rubenstein L, Chao J, et al. Initiation of nonselective alpha1-antagonist therapy and occurrence of hypotension-related adverse events among men with benign prostatic hyperplasia: a retrospective cohort study. Clin Ther. 2001; 23:727–743.

4. Butt DA, Mamdani M, Austin PC, et al. The risk of hip fracture after initiating antihypertensive drugs in the elderly. Arch Intern Med. 2012; 172:1739–1744.

5. Song HJ, Lee J, Kim YJ, et al. beta1 selectivity of beta-blockers and reduced risk of fractures in elderly hypertension patients. Bone. 2012; 51:1008–1015.

6. Souverein PC, Van Staa TP, Egberts AC, et al. Use of alpha-blockers and the risk of hip/femur fractures. J Intern Med. 2003; 254:548–554.

7. Park C, Ha YC, Jang S, et al. The incidence and residual lifetime risk of osteoporosis-related fractures in Korea. J Bone Miner Metab. 2011; 29:744–751.

8. Yoon HK, Park C, Jang S, et al. Incidence and mortality following hip fracture in Korea. J Korean Med Sci. 2011; 26:1087–1092.

9. Lee YK, Jang S, Jang S, et al. Mortality after vertebral fracture in Korea: analysis of the National Claim Registry. Osteoporos Int. 2012; 23:1859–1865.
10. Park C, Jang S, Jang S, et al. Identification and validation of osteoporotic hip fracture using the national health insurance database. J Korean Hip Soc. 2010; 22:305–311.

11. Lee YK, Ha YC, Park C, et al. Bisphosphonate use and increased incidence of subtrochanteric fracture in South Korea: results from the National Claim Registry. Osteoporos Int. 2013; 24:707–711.

12. Kim SH, Ko YB, Lee YK, et al. National utilization of calcium supplements in patients with osteoporotic hip fracture in Korea. J Bone Metab. 2013; 20:99–103.

13. Lee YK, Ha YC, Choi HJ, et al. Bisphosphonate use and subsequent hip fracture in South Korea. Osteoporos Int. 2013; 24:2887–2892.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download