Abstract
Adefovir dipivoxil (ADV) is a nucleotide used as long-term therapy of chronic hepatitis B. Many published reports have shown that long-term high-dose therapy with adefovir can be associated with proximal renal tubular dysfunction resulting in significant hypophosphatemia, renal insufficiency and osteomalacia. We have encountered two patients who developed evidence of hypophosphatemic osteomalacia while on long-term low-dose adefovir therapy for chronic hepatitis B. We report on its clinical features and its potential resolution with cessation of the drug and supplementation with phosphate. We also reviewed the other published cases associated with hypophosphatemic osteomalacia after low-dose adefovir therapy. The symptoms and the hypophosphatemia improved after cessation of the drug and supplementation with phosphate in most cases. Patients taking adefovir long-term should receive regular investigation of the phosphate level and renal function.
The osteomalacia is a metabolic bone disease due to the mineralization disturbance of the organic matrix among the adults and its representing causes include the insufficient vitamin D or phosphate or metabolic disorder. Among the causes, osteomalacia due to hypophosphatemia induced by the impaired absorption in the gastrointestinal tract, impaired re-absorption in the renal tubules, tumor and genetic diseases.[1,2,3]
The adefovir is used as the therapeutic agent for the wild-type hepatitis B virus (HBV) and lamivudine-resistant HBV in the chronic hepatitis B patients.[4] When adefovir is used with high dose for the long time (60-120 mg once daily) to treat the human immunodeficiency virus (HIV), it may cause the nephrotoxicity due to the damages of the proximal tubule with hypophosphatemia, hypouricemia, proteinuria and glycosuria. The hypophosphatemia can lead to the osteomalacia by inhibiting the mineralization of bones.[1] Recently, several papers report the renal diseases in the renal tubules by using the adefovir with the low does (10 mg once daily) and the following hypophosphatemic osteomalacia and the author experiences 2 cases. Here, the study reviews the reported documents and the cases.
Patient: Male with the age of 43
Chief complain: Backache and pain on both knees
Current history: The patient was diagnosed as the chronic hepatitis B 20 years ago before he came to the hospital, had taken the lamivudine for 13 years. Then, the resistance appeared and has taken 10 mg of adefovir for 5 years. The backache has appeared for 6 years with the pain on both knees and myalgia and came to the hospital due to abnormal features in gait.
Past medical history and family history: No specific observation.
Physical examination: The vital sign was normal when the patient came to the hospital, the bone tenderness was found on the spine and both knees and the waddling gate appeared while walking. No observation on the motion and sense losses was found during the neurologic examination.
Lab finding: The blood examination shows 8,990/mm3 of the leukocyte, 15.3 g/dL of the hemoglobin, 429,000/mm3 of the platelet, 2.425 mmol/L of the serum calcium (normal: 2.05-2.55 mmol/L), 0.51 mmol/L of the inorganic phosphorus (normal: 0.74-1.52 mmol/L), 3.93 mmol/L of the blood urea nitrogen (BUN; normal: 2.9-8.2 mmol/L), 114.92 µmol/L of the serum creatinine (normal: 53-106 µmol/L), 21 IU/L of the aspartate transaminase (AST; normal: 10-30 IU/L), 29 IU/L of the alanine transaminase (ALT; normal: 10-40 IU/L) and 1,218 U/L of the alkaline phosphatase (ALP; normal: 30-120 U/L). During the urine examination, 1,000 mg/dL (3+) of the glycosuria and 0.6 g/day of proteinuria were observed. However, hematuria was not founded. Urinary excretion amount of the calcium and the phosphate was not measured. The serum 1,25-dihydroxy-vitamin D3 (1,25[OH]2D3) recorded 133.9 pmol/L (normal: 60-108 pmol/L) but the parathyroid hormone (PTH) was in the normal range of 42.95 pg/mL (normal: 10-65 pg/mL).
Radiographic finding: Bone density was decreased on the spine and pelvis on simple x-ray. And fracture was suspicious due to crack in the cortical bone (Fig. 1). In the bone mineral density (BMD), the T-score of the spine marked -5.1 (average value of L1-L4) and the osteoporosis was observed (Fig. 2A) and the strong multiple hot uptakes were found in the bone scan (Fig. 3A). The computed tomography (CT) test which was performed to find out the primary lesion considering the possibility for the carcinogenic bone metastasis observed the fracture on the 7th spinous process (Fig. 4).
Bone biopsy: The bone biopsy was performed on the 7th spinous process with the observation from the CT and a lot of osteoid tissues without mineralization including a lot of osteoblasts were found (Fig. 5A, B).
Treatment and progress: It was diagnosed that the osteroporosis appeared due to the hypophosphatemia based on the hypophosphatemia, ALP increase, images and biopsy and estimated that it was caused by the adefovir use. The alendronate (70 mg, once a week), the bisphosphonate medicine was administered as the treatment, the patient was instructed to take food with a lot of phosphate, to stop using the adefovir and to use the entecavir. Since then, the myalgia was mitigated and the spinal T-score was improved to -1.8 based on the BMD. Now, the patient is under the tracking observation at the clinic.
Patient: Male with the age of 42
Chief complain: Backache and pain on both chests
Current history: The patient was diagnosed as the chronic hepatitis B 11 years ago before he came to the hospital, had taken the lamivudine. Then, the resistance appeared and has taken 10mg of adefovir for 7 years. Then the patient came to the hospital due to the backache and pain on both chests suffered from 3 months before he came to the hospital.
Past medical history and family history: No specific observation.
Physical examination: The vital signs were normal when the patient came to the hospital. Tenderness of spine and both chests was observed. But, motor and sensory disturbance was not founded during neurologic examination.
Lab finding: The blood examination shows 6,760/mm3 of the leukocyte, 14.9 g/dL of the hemoglobin, 272,000/mm3 of the platelet, 2.40 mmol/L of the serum calcium, 0.52 mmol/L of the inorganic phosphorus, 7.5 mmol/L of the BUN, 141.4 µmol/L of the serum creatinine, 18 IU/L of the AST, 21 IU/L of the ALT and 702 U/L of the ALP. During the urine examination, 300 mg/dL (2+) of the glycosuria and 1.1 g/day of the proteinuria were observed. However, hematuria was not found correlated. The serum 1,25(OH)2D3 recorded 80.0 pmol/L but the PTH was in the normal range of 21.1 pg/mL.
Radiographic finding: In the BMD, the T-score of the spine marked -2.1 (average value of L1-L4) and the osteoporosis was observed (Fig. 2B) and the strong multiple hot uptakes were found in the bone scan (Fig. 3B).
Treatment and progress: As shown in the case 1, the patient in the case 2 was instructed to stop using the adefovir under the diagnosis of the hypophosphatemic osteomalacia due to hypophosphatemia, ALP increase and images, changed to use the entecarvir and the bisphosphonate medicine (alendronate) was administered with the among of 70 mg (once a week). Currently, the pain on both chests was improved and the spinal T-score was improved to 0.75 based on the BMD. The patient is under the tracking observation.
The adefovir inhibits the reverse transcriptase and the DNA synthetase to prohibit the HBV proliferation. That is why the adefovir is used for the initial treatment of the chronic hepatitis B or the tolerance against the lamivudine.[1] The nephrotoxicity appears due to the damages of the proximal tubule when the adefovir is administered with high doses for a long time. Adefovir inhibits the mitochondria DNA growth in the epithelial cell of the proximal tubule and prohibits the oxdative phosphorylation, causing the cell necrosis.[5] And then, absorption of phosphate in the proximal tubule is impaired and lead to hypophosphatemic osteomalacia.[3,5] Nephrotoxicity of the adefovir was reported depending on the quantity for the high dose over 60 mg to mainly treat the HIV.[6] Izzedine et al.[6] reported that comparision with 10 mg and 30 mg of adefovir to treat chronic hepatitis B. The group with 30 mg shows increase the serum creatinine, decrease in the serum phosphate and high portion of nephrotoxicity with proteinuria and glycosuria. However, the group with 10 mg of the adefovir shows similar result to the control group. They suggest that the use of the adefovir with the low dose of 10 mg is safe against the nephrotoxicity to treat the chronic hepatitis B. However, local and foreign studies find out that not only the nephrotoxicity but also the osteomalacia appear even after using a small dose of the adefovir of 10 mg.
The osteomalacia is due to the inhibition in the mineralization of newly formed osteoids by the deficiency in the vitamin D or phosphate or metabolic disorder, causes pain on the bone and the muscle weakness. It may be diagnosed by biochemical examinations including serum calcium, phosphorous, ALP, PTH, BUN and creatinine, image examinations like simple radiography and bone scan and osseous tissue examination.[2,3,7] The osteomalacia due to insufficient vitamin D shows the decrease in the serum calcium, phosphorous and 1,25(OH)2D and increase in the ALP and PTH. However, the hypophosphatemic osteomalacia due to damaged proximal tubule may show decrease in the serum phosphorous, ALP increase and normal serum calcium, PTH and 1,25(OH)2D.[3] In the radiogrphic aspect, the decrease in the bone shadows and pseudofracture may be found from the simple radiographic image and the hot uptake may be found in the bone scan. The BMD is not required in the diagnosis but most osteomalacia patients show decrease in the bone density and the osteomalacia is questioned from the osseous tissue examination. However, it may be rarely performed if the diagnosis is difficult from the noninvasive examination with the features of increasing the sutured gap between the osteoids, time delay to the mineralization and increase in the osteoid tissues.[1,8]
The patient in the case 1 of the study has symptoms of bone pain and body weakness shows the opinions of the normal serum calcium and decrease in the serum phosphate from the hematological examination, ALP increase and normal PTH and the observation of decreasing the bone density and suspicious fracture due to the cracked cortical bone was found in the simple X-ray. Also, the multiple hot uptake was found in the bone scan and a lot of osteoid tissues without the mineralization including the osteoblast in the osseous tissue examination, being diagnosed as the osteomalacia accompanied with the hypophosphatemia. No family history of the genetic diseases is found and no evidence of the tumors are discovered from the CT. Also, there is no intake history of special medicines other than the adefovir and it is diagnosed as the hypophosphatemic osteomalacia due to using the adefovir for a long period of time. Similar to the case 2 of the study, the patient shows decrease in the serum phosphate, ALP increase and normal PTH, as well as the multiple hot uptake from the bone scan and is diagnosed as the hypophosphatemic osteomalacia due to using the adefovir.
The medicine of cause is suspended to treat the hypophosphatemic osteomalacia and it is effective to inject the vitamin D and phosphorous.[9] Two third of the daily recommended dose of the phosphorous for a normal person a day is absorbed to the intestines and most of the phosphate filtered in the proximal tubule is absorbed again. The oral intake of the phosphorous is effective in treating the hypophosphatemic osteomalacia due to degrading re-absorption of the phosphate from the kidneys by assisting the deposition of the inorganic materials from the bones.[2,10] The case also shows the improvement by suspending the use of the adefovir and injecting the phosphate.
About 18 cases of the hypophosphatemic osteomalacia due to using the adefovir with low dose have been reported since 2008 and the study collects the characteristics and various examination results (Table 1).
It is found out that 6 cases in Korea, 6 cases in China, 3 cases in Japan and 1 cases in France, Australia and Italy each, showing that most cases are reported in East Asian countries. The gender ratio of male and female patients shows the male domination of 15:3 and the average age is 52.9 (22-74) years old. Half of the patients accompany the liver cirrhosis and its main symptoms include the muscle weakness and bone pain. The median value of using the adefovir until the symptom appears is 33.7 months (8-68 months) and the median value of using the adefovir until the hypophosphatemia appears is 38.3 months (6-72 months). The phosphate level in the blood is lower than the normal range in most cases, 0.3-0.77 mmol/L and most cases with the low serum phosphorous level, glycosuria and proteinuria show that the impaired absorption in the proximal tubule. The study performs the BMD from 9 cases and confirms the osteomalacia and osteoporosis. After adefovir is discontinued in most cases and phosphate is supplied, the clinical symptoms and hypophosphatemia were improved. The adefovir is the nucleotide analogue and excreted by the active transportation through the translocator from the renal tubule, as well as the glomerular filtration.[20] The adefovir causes the nephrotoxicity due to the cell necrosis by inhibiting the mytocondria DNA synthesis and the nephrotoxicity increases more due to improper excretion by directly affeting the translocator.[24] A total of 13 patients stop using the adefovir as the treatment and 6 of them change the medicine to the entecavir. It mainly performs the glomerular excretion with the nucleoside analogue and there are a lot of reports that it shows less nephrotoxicity compared to the adefovir.[5,7,24,25] The 2 cases in the study change to the entecavir and the symptoms are improved.
It is required to periodically measure the serum phosphorous and renal function considering the possibility for the hypophosphatemic osteomalacia due to damaged proximal tubule in the patients who use the adefovir due to the chronic hepatitis B. As well, it is important to conduct the health questionnaire to the patients with the bone pains and muscle weakness on the history of drugs.
Figures and Tables
 | Fig. 1Simple x-ray of pelvis showed osteopenia. Suspicous cortical disruption at left superior pubic ramus. R/O fracture (arrow). |
 | Fig. 3(A) Whole body bone scan reveals multiplehot spots at anterior and posterior aspect of right 1-10th ribs, and left 1-11th ribs, spinous process of C-7, left 5-9th costovertebral junctions, posterior aspect of left ischium and right sided sacral wing (case 1). (B) Whole body bone scan reveals multiple hot spots in both bony ribs (case 2). |
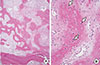 | Fig. 5(A) Light microscopic findings show unmineralized irregular bony spicules and abundant fibrotic marrow spaces. (B) High magnification of a shows unmineralized osteoid tissue with many osteoblastic cells (arrows). Hematoxylin-Eosin stain, A: ×40, B: ×200. |
Table 1
Characteristics of the 18 cases hypophosphatemic osteomalacia after low dose (10 mg once daily) adefovir therapy.

ADV, adefovir; CHB, chronic hepatitis B; LC, liver cirrhosis; HCC, hepatocellular carcinoma; DM, diabetes mellitus; LTP, liver transplant; RTP, renal transplant; P, phosphate; Ca, calcium; PTH, parathyroid hormone; 1,25(OH)2D3, 1,25-dihydroxy-vitamin D3; Cr, creatinine; BMD, bone mineral density; ETV, entecavir.
References
1. Lee HJ, Choi JW, Kim TN, et al. A case of severe hypophosphatemia related to adefovir dipivoxil treatment in a patient with liver cirrhosis related to hepatitis B virus. Korean J Hepatol. 2008; 14:381–386.

2. Lee HC, Song YD, Ahn KJ, et al. A case adult onset hypophosphatemic osteomalacia. J Korean Soc Endocrinol. 1991; 6:75–81.
3. Yoo KD, Jeong JH, Cho SK, et al. A case of hypophosphatemic osteomalacia associated with low-dose adefovir dipivoxil treatment. Korean J Med. 2010; 78:261–265.
5. Tanji N, Tanji K, Kambham N, et al. Adefovir nephrotoxicity: possible role of mitochondrial DNA depletion. Hum Pathol. 2001; 32:734–740.

6. Izzedine H, Hulot JS, Launay-Vacher V, et al. Renal safety of adefovir dipivoxil in patients with chronic hepatitis B: two double-blind, randomized, placebo-controlled studies. Kidney Int. 2004; 66:1153–1158.

7. Gara N, Zhao X, Collins MT, et al. Renal tubular dysfunction during long-term adefovir or tenofovir therapy in chronic hepatitis B. Aliment Pharmacol Ther. 2012; 35:1317–1325.

8. Parfitt AM. Vitamin D and the pathogenesis of riskets and osteomalacia. In : Feldman D, Pike JW, Glorieux FH, editors. Vitamin D. 2nd ed. San Diego, CA: Elsevier Academic Press;2005. p. 1029–1048.
9. Kwon SY, Ahn SY, Ko SY, et al. A case of osteomalacia related to adefovir in a patient with chronic hepatitis B. Korean J Gastroenterol. 2010; 56:117–120.

10. Wilson DR, York SE, Jaworski ZF, et al. Studies in hypophosphatemic vitamin D-refractory osteomalacia in adults. Medicine (Baltimore). 1965; 44:99–134.

11. Jung YK, Yeon JE, Choi JH, et al. Fanconi's syndrome associated with prolonged adefovir dipivoxil therapy in a hepatitis B virus patient. Gut Liver. 2010; 4:389–393.

12. Kim DH, Sung DH, Min YK. Hypophosphatemic osteomalacia induced by low-dose adefovir therapy: focus on manifestations in the skeletal system and literature review. J Bone Miner Metab. 2013; 31:240–246.

13. Girgis CM, Wong T, Ngu MC, et al. Hypophosphataemic osteomalacia in patients on adefovir dipivoxil. J Clin Gastroenterol. 2011; 45:468–473.

14. Law ST, Li KK, Ho YY. Acquired Fanconi syndrome associated with prolonged adefovir dipivoxil therapy in a chronic hepatitis B patient. Am J Ther. 2013; 20:e713–e716. doi: 10.1097/MJT.0b013e31820c4b20.

15. Sun XF, Zhang HB, Li XP, et al. A case of adefovir dipivoxil induced hypophosphataemic osteomalacia and literature review. Zhonghua Nei Ke Za Zhi. 2011; 50:754–757.
16. Li L, Dong GF, Zhang X, et al. Adefovir dipivoxil-induced Fanconi syndrome and hypophosphatemic osteomalacia associated with muscular weakness in a patient with chronic hepatitis B. Nan Fang Yi Ke Da Xue Xue Bao. 2011; 31:1956.
17. Wu C, Zhang H, Qian Y, et al. Hypophosphatemic osteomalacia and renal Fanconi syndrome induced by low-dose adefovir dipivoxil: a case report and literature review suggesting ethnic predisposition. J Clin Pharm Ther. 2013; 38:321–326.

18. Tamori A, Enomoto M, Kobayashi S, et al. Add-on combination therapy with adefovir dipivoxil induces renal impairment in patients with lamivudine-refractory hepatitis B virus. J Viral Hepat. 2010; 17:123–129.

19. Minemura M, Tokimitsu Y, Tajiri K, et al. Development of osteomalacia in a post-liver transplant patient receiving adefovir dipivoxil. World J Hepatol. 2010; 2:442–446.

20. Shimohata H, Sakai S, Ogawa Y, et al. Osteomalacia due to Fanconi's syndrome and renal failure caused by long-term low-dose adefovir dipivoxil. Clin Exp Nephrol. 2013; 17:147–148.

21. Izzedine H, Kheder-Elfekih R, Housset P, et al. Adefovir dipivoxil-induced acute tubular necrosis and Fanconi syndrome in a renal transplant patient. AIDS. 2009; 23:544–545.

22. Wong T, Girgis CM, Ngu MC, et al. Hypophosphatemic osteomalacia after low-dose adefovir dipivoxil therapy for hepatitis B. J Clin Endocrinol Metab. 2010; 95:479–480.

23. Fabbriciani G, de Socio GV, Massarotti M, et al. Adefovir induced hypophosphatemic osteomalacia. Scand J Infect Dis. 2011; 43:990–992.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download