Abstract
Glucocorticoid (GC) excess, including Cushing's syndrome, is a common cause of secondary osteoporosis. Thirty to fifty percent of Cushing's syndrome patients experience non-traumatic fractures, which is often the presenting manifestation of Cushing's syndrome. However, there have been rare cases of Cushing's syndrome diagnosed only based upon bone manifestations. We describe a case of Cushing's syndrome that was diagnosed in a 44-year-old woman who initially visited our hospital due to multiple non-traumatic rib fractures. She did not exhibit any other manifestations of Cushing's syndrome such as moon face, buffalo hump or abdominal striae. Initially, we evaluated her for bone metastases from a cancer of unknown origin, but there was no evidence of metastatic cancer. Instead, we found a left adrenal incidentaloma. As a result of the hormone study, she was diagnosed as having Cushing's syndrome. Interestingly, her bony manifestation of Cushing's syndrome, which was evident in the bone scan and bone mineral densitometry, completely recovered after a left adrenalectomy. Therefore, the possibility of Cushing's syndrome as a cause of secondary osteoporosis should be considered in young patients with non-traumatic multiple fractures, with or without any other typical features of Cushing's syndrome.
Glucocorticoid (GC) excess, including Cushing's syndrome, is a common cause of secondary osteoporosis.[1,2] Several reports have confirmed the high prevalence of various degrees of osteopenia/osteoporosis in patients with hypercortisolism.[3] The prevalence of osteopenia and osteoporosis in Cushing's syndrome is diverse among studies, with approximate ranges from 60-80% and 30-65%, respectively.[2,4,5] Also, 30-50% of patients with Cushing's syndrome experience non-traumatic fractures, which can be the presenting manifestation of Cushing's syndrome.[3] Approximately one third of patients develop vertebral fractures, especially at the level of the thoracic and lumbar vertebral bodies.[3,6] Spontaneous fractures may also occur in the ribs and pelvis, and less commonly in the long bones. [3] However, there are rare cases diagnosed as Cushing's syndrome based solely on bony manifestations.[7] In Korea, only two cases have been reported in which Cushing's syndrome was diagnosed after pathologic vertebral fractures occurred in young females.[7,8] We described a case where Cushing's syndrome was diagnosed in a 44-year-old woman who visited our hospital due to multiple non-traumatic rib fractures.
A 44-year-old woman was referred to our hospital on May 2009 due to an abnormal chest X-ray finding. She had a chest X-ray before a gastrofibroscopy at a local hospital. There were multiple rib fractures (Fig. 1). For further evaluation, she had a chest computed tomography (CT) scan done before visiting our hospital. The chest CT revealed multiple sclerotic masses with bone destruction in both hemithoraxes (right 2nd, 4th, 5th, 6th, 7th, and 10th ribs, left 2nd, 4th, 7th, 8th, and 9th ribs) of variable size (Fig. 2). Initially she was admitted to the pulmonology department to rule out bony metastases from a cancer of unknown origin. She had taken the bone densitometry of the L1-L4 lumbar spine by dual energy X-ray absorptiometry (DXA), at the local department of gynecology 1.5 years ago. The result of bone mineral density (BMD) was 0.726 g/cm2 and the average T-score of the L1-L4 lumbar spine was -2.6. The average Z-score of the L1-L4 lumbar spine was -2.0. Therefore, she was taking calcium, vitamin D supplements and hormone replacement therapy for osteoporosis. She also had a conization in 2002 due to squamous cell carcinoma in situ at the uterine cervix and thereafter received a total hysterectomy in 2005 due to uterine leiomyoma. She had no alcohol drinking or smoking history. There were no abnormal findings in her family history. Also, she had no trauma history. She did not have moon face, buffalo hump, or abdominal straie. She didn't have any pain on her ribs. On the physical examination, there wasn't tenderness around fracture sites. Her height and weight were 153 cm and 53 kg, respectively, with a body mass index (BMI) of 22 kg/m2. Her waist measurement was 83 cm, and she had experienced no recent weight changes. Her blood pressure was 140/80 mmHg with a pulse of 96 beats/min, a respiratory rate of 20 breaths/min, and a body temperature of 36.8℃. On the blood test, the leukocyte, hemoglobin, and platelet counts were 8,900/mm3 (neutrophils 85.9%, lymphocyte 8.4%, monocyte 5.7%), 14.9 g/dL, and 184,000/µL, respectively. Fasting glucose, albumin, aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase, and creatinine were 93 mg/dL, 4.0 g/dL, 45 IU/L, 81 IU/L, 49 IU/L, and 0.56 mg/dL, respectively. Total calcium and phosphate were 10.5 mg/dL and 3.5 mg/dL, respectively. In addition, serum intact parathyroid hormone (PTH) was 35.6 pg/mL (normal range, 13-54 pg/mL).
To evaluate the patient for metastatic cancer, a bone biopsy was performed at the right 6th rib posterior arc in the pulmonology department. Also a bone scan and the bone densitometry of the L1-L4 lumbar spine and an abdominal CT were performed. Fragmented bony particles with small amounts of marrow tissue were observed in the biopsy tissue.
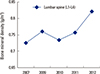
There were no cancer cells nor cytokeratin (CK)-positive epithelial cells on immunohistochemical staining. There was no cancerous lesion in abdomen CT, except a left adrenal incidentaloma, a well-marginated soft tissue mass 25 mm in diameter, was found (Fig. 3). On the bone scan, multi-focal increased uptake was observed in both ribs, suggesting non-traumatic micro-fractures caused by osteoporosis (Fig. 4A). The average BMD, T-score and Z-score of the L1-L4 lumbar spine was 0.761 g/cm2, -2.1 and -1.7, respectively. Therefore, an endocrine cause of osteoporotic fracture was suspected, and a hormonal study for adrenal incidentaloma was performed. Free cortisol in the urine and 17-hydroxycorticosteroid were 580.4 µg/day (normal range, 20-90 µg/day) and 12.93 mg/day (normal range, 3-15 mg/day), respectively. A low-dose dexamethasone suppression test showed that the serum adrenocorticotrophic hormone level was 1.4 pg/mL (normal <130 pg/mL), the basal cortisol was 26.3 µg/dL and the cortisol on the 3rd day was 35.4 µg/dL (normal, 3-6 µg/dL). Cortisol was not suppressed. Finally, she was diagnosed with Cushing's syndrome due to the left adrenocortical adenoma. A laparoscopic left adrenalectomy was performed in June 2009. A month after the laparoscopic left adrenalectomy, 24-hr urine free cortisol was checked, and was below 1.8 µg/day. A bone scan taken 1 year after the operation showed decreased multifocal uptake in the bilateral ribs (Fig. 4B) and the patient's BMD improved gradually, reaching 0.822 g/cm2 in 2012 (Fig. 5). Also, the average T-score and Z-score of the L1-L4 lumbar spine improved, reaching -1.6 and -1.0, respectively. Currently, she is being regularly followed-up and taking calcium and vitamin D for osteopenia.
Cushing's syndrome encompasses a variety of clinical features that result from chronic exposure to excess GCs of any etiology. Cushing's syndrome occurs with an incidence of 1-2 per 100,000 persons per year.[9] The clinical manifestations of Cushing's syndrome are central obesity with supraclavicular fat accumulation, a cervical fat pad, thinned skin, purple striae, proximal muscle weakness, fatigue, hypertension, glucose intolerance, acne, hirsutism, menstrual irregularity, and osteoporotic vertebral fractures.[6,9] However, the clinical manifestations of Cushing's syndrome are not always definite so that sometimes clinical suspicion should arise preferentially by the physician.[6] Furthermore, because of its variable pattern of the biochemical parameters, diagnosis of Cushing's syndrome is often difficult for clinicians.[6,10]
Osteoporosis is one of the major features of either exogenous or endogenous GC excess.[11,12] The prevalence of osteoporosis due to endogenous GC excess has been reported to be present in 50-59% of cases,[4,13,14] and approximately 30-50% of patients with the condition experience non-traumatic fractures.[2,4,11] Secondary osteoporosis is more common in men or premenopausal women than postmenopausal women.[15] Secondary osteoporosis is defined as bone loss, microarchitectural alterations, and fragility fractures due to an underlying disease or concurrent medication.[1] Clinicians should be suspicious and evaluate for secondary osteoporosis in male or premenopausal female patients with unexplained bone loss, a history of fragility fractures or very low BMD values and fractures despite anti-osteoporotic therapy, as in this case.[3,15] Moreover, because osteoporotic fractures can be the only presenting manifestation of Cushing's syndrome, secondary osteoporosis caused by Cushing's syndrome should be considered in patients with unclear causes of osteoporotic fractures.
Although the patient in this case was a relatively young female who had already taken calcium, vitamin D supplements and hormonal replacement therapy for osteoporosis, asymptomatic multiple pathologic rib fractures were incidentally discovered in a routine chest X-ray. Because she exhibited no typical signs of Cushing's syndrome such as moon face, truncal obesity, thinned skin or purple striae and showed no associated features of Cushing's syndrome, such as diabetes mellitus or hypertension, she was not initially suspected of Cushing's syndrome. At first, the pulmonology department worked her up for metastatic cancer of unknown origin. However, they did not find any evidence of metastatic cancer, and incidentally found the left adrenal adenoma on abdominal CT. Then, we suspected Cushing's syndrome and performed endocrine function tests, which confirmed the diagnosis. There have only been two Korean cases of Cushing's syndrome previously diagnosed after recurrent non-traumatic fractures occurring in young females. However, both of these cases were accompanied by vertebral fractures, not rib fractures. Our case is the first report that diagnosed Cushing's syndrome by multiple ribfractures without vertebral fractures, which are the most affected fracture site in Cushing's syndrome.
GCs affect bone metabolism by enhancing bone resorption and decreasing bone formation.[16] They act in two phases: a rapid, early phase in which BMD falls by excessive bone resorption, and a slower, more progressive phase in which BMD declines as a result of impaired bone formation.[15] An early phase of excessive bone resorption is due to the action of GCs on calcium metabolism by inhibition of calcium absorption from the gut through a mechanism independent of vitamin D, increasing the urinary excretion of calcium and increasing osteoclast activity.[3,16] This induces an increase in PTH levels.[3] However, most studies have found differences between GC-induced osteoporosis (GIO) and the hyperparathyroid state. In GIO, preferential bone loss tends to occur in cancellous bone, in contrast to primary hyperparathyroidism where preferential bone loss occurs in cortical skeletal bone.[3,15] As a result, greater bone mineral loss in the vertebral spine is commonly observed in patients with Cushing's syndrome.[16] Moreover, GIO shows reduced bone turnover, whereas bone turnover is enhanced in primary hyperparathyroidism.[3,15] Also, the slower phase of impaired bone formation is due to a decrease in osteoblast number and function.[15] Hypercortisolism inhibits replication of cells of osteoblastic lineage and osteoblastogenic differentiation, decreases osteoblast function and increases apoptosis of osteoblasts and osteocytes.[3,15] In addition, GCs inhibit alkaline phosphatase activity, production of type I collagen and synthesis of non-collagenous bone protein like osteocalcin.[3] Many studies that evaluated bone formation with serum osteocalcin levels found that it was greatly suppressed in endogenous GIO.[2]
An important feature of GIO is that it is reversible. After cure of hypercortisolism by both an adrenalectomy or pituitary adenomectomy, an increase in BMD, which can even reach normal levels,[17] has been described and a time-dependent rise was observed.[2,18,19,20] Manning et al.[17] reported that the BMD of 17 adult Cushing's syndrome patients, who had been cured, recovered to normal values and there was a positive relationship between bone density and the time since cure by a unilateral adrenalectomy, which requires approximately 10 years for complete recovery. Kristo et al.[18] followed 33 patients with Cushing's syndrome before and after treatment. They also observed a time-dependent rise in BMD, which was paralleled by increased osteocalcin. One of the two Korean cases did not report progress in the bony manifestations of Cushing's syndrome after treatment,[8] while the other case showed a slight improvement in BMD, but new compression fractures developed during the course of treatment.[7] Interestingly, we showed that multifocal increased uptake of the ribs on bone scan completely disappeared one year after left adrenalectomy. Furthermore, BMD significantly increased after 2 years with no additional fractures.
In conclusion, although a patient may not exhibit typical features of Cushing's syndrome, this disease should be considered in young adults with multifocal non-traumatic rib fractures, as they could be bony manifestations that can be completely eliminated by treatment.
Figures and Tables
 | Fig. 2Chest computed tomography showed multiple sclerotic lesions of the ribs of both sides (left 4th, right 4th, 5th rib). |
 | Fig. 3Abdominal computed tomography showed a 2.5 × 2.0 cm sized mass (black arrow) on the left adrenal gland. |
References
1. Hofbauer LC, Hamann C, Ebeling PR. Approach to the patient with secondary osteoporosis. Eur J Endocrinol. 2010; 162:1009–1020.

2. Tóth M, Grossman A. Glucocorticoid-induced osteoporosis: lessons from Cushing's syndrome. Clin Endocrinol (Oxf). 2013; 79:1–11.

4. Kawamata A, Iihara M, Okamoto T, et al. Bone mineral density before and after surgical cure of Cushing's syndrome due to adrenocortical adenoma: prospective study. World J Surg. 2008; 32:890–896.

5. van der Eerden AW, den Heijer M, Oyen WJ, et al. Cushing's syndrome and bone mineral density: lowest Z scores in young patients. Neth J Med. 2007; 65:137–141.
6. Arnaldi G, Angeli A, Atkinson AB, et al. Diagnosis and complications of Cushing's syndrome: a consensus statement. J Clin Endocrinol Metab. 2003; 88:5593–5602.

7. Han JY, Lee J, Kim GE, et al. A case of cushing syndrome diagnosed by recurrent pathologic fractures in a young woman. J Bone Metab. 2012; 19:153–158.

8. Jung MH, Choi H, Kim JY, et al. Vertebral compression fracture in Cushing's syndrome with adrenal adenoma. J Korean Soc Osteoporos. 2009; 7:209–213.
9. Longo DL, Fauci AS, Kasper DL, et al. Harrison's principles of internal medicine. 18th ed. New York, NY: McGraw-Hill;2012.
11. Vestergaard P, Lindholm J, Jørgensen JO, et al. Increased risk of osteoporotic fractures in patients with Cushing's syndrome. Eur J Endocrinol. 2002; 146:51–56.

12. Camozzi V, Sanguin F, Albigier N, et al. Persistent increase of osteoprotegerin levels after cortisol normalization in patients with Cushing's syndrome. Eur J Endocrinol. 2010; 162:85–90.

13. Minetto M, Reimondo G, Osella G, et al. Bone loss is more severe in primary adrenal than in pituitary-dependent Cushing's syndrome. Osteoporos Int. 2004; 15:855–861.

14. Ohmori N, Nomura K, Ohmori K, et al. Osteoporosis is more prevalent in adrenal than in pituitary Cushing's syndrome. Endocr J. 2003; 50:1–7.

15. Mazziotti G, Angeli A, Bilezikian JP, et al. Glucocorticoid-induced osteoporosis: an update. Trends Endocrinol Metab. 2006; 17:144–149.

16. Canalis E. Clinical review 83: mechanisms of glucocorticoid action in bone: implications to glucocorticoid-induced osteoporosis. J Clin Endocrinol Metab. 1996; 81:3441–3447.

17. Manning PJ, Evans MC, Reid IR. Normal bone mineral density following cure of Cushing's syndrome. Clin Endocrinol (Oxf). 1992; 36:229–234.

18. Kristo C, Jemtland R, Ueland T, et al. Restoration of the coupling process and normalization of bone mass following successful treatment of endogenous Cushing's syndrome: a prospective, long-term study. Eur J Endocrinol. 2006; 154:109–118.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download