Abstract
Background
Osteoporosis treatment following hip fracture is well known to not enough. We previously performed intervention study for orthopaedic surgeon's education and reported twofold increase in osteoporosis detection and treatment rate observed between 2005 and 2007. This follow-up observational study was conducted to find out the rate in which a diagnostic workup and treatment for osteoporosis were done in patients with hip fracture.
Methods
Medical records and radiographs in patients who were older than 50 years and diagnosed as having femoral neck or intertrochanteric fractures at 8 hospitals in Jeju island, South Korea from 2008 to 2011 were reviewed. The numbers of patients who were studied with bone densitometry and who were treated for osteoporosis after the diagnosis of hip fracture were analyzed.
Results
Nine hundred forty five hip fractures (201 in 2008, 257 in 2009, 265 in 2010, and 304 in 2011) occurred in 191 men and 754 women during the study periods. The mean age of the patients was 79.7 years. The mean rate of osteoporosis detection using dual energy X-ray absorptiometry was 36.4% (344/945 hips) (ranged from 24.2% in 2009 to 40.5% in 2011). The mean initiation rate of osteoporosis treatment was 23.1% (218/945 hips) (ranged from 20% in 2009 to 29% in 2008).
Osteoporosis has become a major public health issue rapidly increasing around the world. It has been reported that major demographic changes will occur in Asia. Recently, several studies were reported prevalence of osteoporosis in Korea.[1,2,3] Although reported prevalence of osteoporosis were not same in studies because of different baseline characteristics such as age, demographics and proportion of elderly persons, one in 3 women and 1 in 10 men in adults aged 50 years or older in Korea has osteoporosis.[1,2,3,4] The residual lifetime probabilities of osteoporosis-related fractures at the age of 50 years are 59.5% for women and 23.8% for men and residual lifetime probabilities of hip fracture are osteoporosis-related fractures are 12.3 for women and 5.2 in men.[4] Mortality within one year after hip fracture is ranged from 6% to 44% and 5-year relative survival after osteoporotic hip fracture was below those of the general populations and was similar to thyroid and breast cancer.[5,6,7,8] Morbidity in patients with hip fracture was severely decreasing after hip fracture.[9,10,11] Only one in 3 patients with normal activity at pre-injury state could be recovered normal daily activity and 1 in 3 patients could not be able outdoor activity.[9]
To prevent osteoporotic fracture, there are a number of pharmaceutical treatments now available that have been shown in randomized trials. Reduction rate of osteoporotic fractures of anti-osteoporosis medication have demonstrated ranging from 30% to 70%.[12,13,14] However, the persistence and compliance of patients in the real world was lower than those in clinical trials. Undertreatment of anti-osteoporosis medications in patient with osteoporosis and/or osteoporotic-fractures is notorious in the real world. [15,16,17] This situation in Korea is consistent with other studies and recent study reported that the treatment rate for osteoporosis in Korea was only 12.8% in general population.[2]
We performed a before and after study of educational program for orthopedic surgeons in 2007 and reported that 94 patients (45.2%) underwent detection of osteoporosis by dual energy X-ray absorptiometry (DXA) and 67 patients (32.2%) were prescribed medication for osteoporosis at the time of discharge.[18] The detection and medication rate for osteoporosis after hip fracture increased twofold after orthopedic surgeons had attended the intervention program.[18] However, the osteoporosis treatment rate was still inadequate. After that, we have been continuously monitoring the management of osteoporosis after hip fracture since 2007.
Therefore, this study was to determine 1) the detection and medication rate and 2) type of prescription of anti-osteoporotic medications in patients with age of 50 or older who were admitted for a hip fracture between January 1, 2008 and December 31, 2011 from the eight hospitals.
Participants in the study were drawn from a cohort that has been monitored from 2002 to determine the incidences of hip fractures and mortality and morbidity rates after hip fracture.[9,18,19] This larger cohort was recruited on Jeju Island, the largest Korean island, which is located southwest of the Korean peninsula. In 2011, Jeju Island (the biggest island of Korea, which is located southwest of the Korean peninsula) had a population of 576,156 including 74,985 men and 90,481 women ≥50 years of age, with 12.1% being ≥65 years of age (9.3% of men and 14.9% of women). There are eight hospitals (one university hospital and seven general hospitals) on the island with an orthopaedic department and emergency admission facilities. The medical records and radiography of the eight hospitals between January 2008 and December 2011 were reviewed to identify patients with hip fractures.
Patients who met the diagnostic criteria of femoral neck and intertrochanteric fractures of the International Classification of Diseases 10th revision (ICD-10; S720 and S721) and were older than 50 years at the time of the fracture were recruited. The exclusion criteria were: nonresidents of Jeju Island, fractures of pathologic bone (e.g. metastasis), isolated fractures of the greater or lesser trochanter, and fractures of the subtrochanteric region due to high energy injuries.[18]
Hospital data evaluations were performed 6 and 12 months after discharge from the hospital, and every 6 months thereafter. From the medical records we determined diagnosis at admission, mechanism of injury, detection of osteoporosis (DXA), procedures performed during hospitalization, and discharge medications.
Osteoporosis treatment was defined as medication including a selective estrogen receptor modulator (SERM), bisphosphonate, or calcitonin therapy or hormone replacement. Treatment initiation and duration were confirmed by reviewing medical records at 6 months and 12 months after discharge from hospital.
The denominator to calculate the crude fracture incidence was the mid-year population of each year (the population at July 1 of each year). We used the resident population data released annually by the Korea National Statistical Office to calculate the mid-year population, which was the mean of two populations of two consecutive years. The rate of osteoporosis detection, initiation rate of osteoporosis treatment, and type of prescribing anti-osteoporotic medication during study periods was analyzed using SPSS, version 18.0 (SPSS Inc., Chicago, IL, USA).
During the study periods, 945 hip fractures (201 in 2008, 257 in 2009, 265 in 2010, and 304 in 2011) occurred in 483 femoral neck fractures (51.1%), and 462 intertrochanteric fractures (48.9%) in 191 men and 754 women during the study periods. The mean age of the patients was 79.7 years (72.8 years in men [range, 50 to 95 years] and 81.4 years in women [range, 50 to 100 years]). The fractures occurred during winter in 268 hips (28.4%), fall in 228 (24.1%), spring in 227 (24%), and summer in 222 (23.5%). The causes of fracture were slip down in 849 (89.8%), fall down in 65 (6.9%), minor trauma in 2 (0.2%), and unknown in 29 hips (3.1%) (Table 1). Of 945 hip fractures, 432 hips (45.7%) were preformed arthroplasty, 479 hips (50.7%) were performed internal fixation, and 34 hips (3.6%) refused operations and underwent conservative treatment. The crude incidence of hip fractures in the Jeju population aged 50 years and older increased from 126.6/100,000 in 2002 (70.9/100,000 in men and 167.9/100,000 in women) to 183.7/100,000 in 2011 (89.4/100,000 in men and 261.9/100,000 in women) (Table 2).
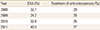
The mean rate of osteoporosis detection was 36.4% (344/945 hips) (ranged from 24.2% in 2009 to 40.5% in 2011). Of 344 who were underwent DXA, only 13 patients (3.8%) underwent DXA examination and medication prior to injury. Three hundred thirty one patients underwent DXA during admission; hip and spine in 328 and hip in three. Two hundred forty two (70.3%) of 344 patients had osteoporosis (T score ≤ -2.5) and 80 patients (23.3%) had osteopenia (-2.5 < T score < -1). The mean initiation rate of osteoporosis treatment was 23.1% (218/945 hips) (ranged from 20% in 2009 to 29% in 2008) (Table 3). Of these 218 patients who were prescribed anti-osteoporotic medications, 185 (84.9%) were prescribed oral bisphosphonates (risedronate, 110 [59.5%], or alendronate, 75 [40.5%]) at the time of discharge. Twenty two patients (10.1%) were prescribed injection of bisphosphonate and 11 patients (5%) were prescribed SERM. Other anti-osteoporotic drugs such as calcitonin and hormone replacement therapy were not prescribed. The mean duration of time these patients were taking osteoporosis medication was 8.5 months (range, 1 to 46 months), and 97 patients (44.5%) received medication for less than 6 months (Table 4).
In previous a before and after study of educational program for orthopedic surgeons in 2007, detection rate of osteoporosis by DXA was 45.2% and anti-osteoporosis medication rate underwent and 67 (32.2%) were prescribed medication for osteoporosis at the time of discharge. However, during follow-up observation period from 2008 to 2011, mean detection rate of osteoporosis and prescription rate of anti-osteoporosis medication was 36.4% and 24.1%, respectively. Our observations suggest the rate of detection and treatment of osteoporosis after a hip fracture among patients has been steady or slightly decreasing since 2007.
Undertreatment of osteoporosis in patients who was diagnosed with osteoporosis is worldwidely similar findings.[2,17,20,21,22] Johnell and Fastbom[20] analyzed use of osteoporosis drugs in a nationwide population using the Swedish Prescribed Drug Register (n=731,105). They reported that osteoporosis drug were used by 16.1% of women and 3.4% of men.[20] Curtis et al.[22] performed cross sectional study using the REasons for Geographic and Racial Differences in Stroke (REGARDS) study (n=24,783) in USA. They reported that only 26% were receiving anti-osteoporosis treatment for high fracture risk group.[22] Choi et al.[2] performed cross sectional study using The Korea National Health and Nutrition Examination Survey 2008-2009 (n= 4,946). They reported that osteoporosis was diagnosed in 29.9% of women aged ≥50 years in Korea. The treatment rate including known and newly diagnosed osteoporosis patients was estimated to be 14.4%.[2] Similarly, the rate treatment of osteoporosis following hip fracture is also at a low rate of 5 % to 32%.[7,18,21,23,24]
However, studies have shown that it is particularly cost-effective to treat osteoporosis and compliance of anti-osteoporosis treatment.[25,26] In addition, several studies reported that compliance of anti-osteoporosis medication in Patients with hip fracture can reduce secondary hip fracture and mortality.[27,28,29] To overcome undertreatment of osteoporosis, several intervention studies targeting clinicians with a view toward increasing treatment rates was performed and reported a greater effect on osteoporosis management rates after hip fracture.[18,30,31,32] Kim et al. [18] performed education of orthopaedic surgeons for improving awareness of osteoporosis treatment following hip fracture and showed an improved medication rate of osteoporosis from 15% to 32%. However, they mentioned that the osteoporosis treatment rate 6 months after hip fracture was still lower than those reported in other intervention studies.[18,30,31,32] They mentioned that orthopaedic surgeons only underwent education sessions, whereas previous studies have involved multimodal approaches, including nurse management programs, standardized algorithms, and monitoring of adherence to treatment as the reason of lower osteoporosis treatment rate. Patient education programs or systemic approaches generally are considered more effective. However, doctor's awareness should be changed before performing studies of education programs or systemic changes for patients.[18] Therefore, intervention study with physician and patients who have diagnosed with osteoporosis is necessary and might be more effective.
Several studies reported seasonal variation of hip fracture and hip fracture most commonly occurred in winter season.[33,34,35] The hip fracture in this study is most commonly caused by slip down and occurs in winter season. The association between hip fracture and causal factors such as snow, slippery pavement and cold temperature has been reported.[36,37,38] Therefore, it is considered that there is a need to construct an alarm system using the media that can prevent osteoporotic fracture in winter season.
However, several limitations of this study should be considered. First, our study was retrospective, not prospective. And thus, selection bias might have been introduced, because this cohort have been studying incidence of hip fracture since 2002. Therefore, many orthopaedic surgeons have awareness of osteoporosis treatment following hip fracture. Nevertheless, lower rate of detection and treatment of osteoporosis is frustrated. In addition, in online survey, physicians indicated lack of patients' awareness and restriction by health insurance guideline as the biggest barriers of treatment in Korea.[39] Second, we could not follow out of town during study periods. This finding might have influence on lower rate of treatment or detection of osteoporosis.
Although the greater than twofold increase in osteoporosis detection observed between 2005 and 2007, detection and treatment rate of osteoporosis following hip fracture during follow-up periods was still not enough. Additional intervention studies are mandatory to further improvement of osteoporosis management after hip fracture.
Figures and Tables
Table 2
Crude incidence rate (per 100,000) of hip fractures among persons ≥ 50 years of age in Jeju, South Korea from 2008 to 2011

References
1. Shin CS, Choi HJ, Kim MJ, et al. Prevalence and risk factors of osteoporosis in Korea: a community-based cohort study with lumbar spine and hip bone mineral density. Bone. 2010; 47:378–387.

2. Choi YJ, Oh HJ, Kim DJ, et al. The prevalence of osteoporosis in Korean adults aged 50 years or older and the higher diagnosis rates in women who were beneficiaries of a national screening program: the Korea National Health and Nutrition Examination Survey 2008-2009. J Bone Miner Res. 2012; 27:1879–1886.

3. Choi HJ, Shin CS, Ha YC, et al. Burden of osteoporosis in adults in Korea: a national health insurance database study. J Bone Miner Metab. 2012; 30:54–58.

4. Park C, Ha YC, Jang S, et al. The incidence and residual lifetime risk of osteoporosis-related fractures in Korea. J Bone Miner Metab. 2011; 29:744–751.

5. Lee YK, Lee YJ, Ha YC, et al. Five-year relative survival of patients with osteoporotic hip fracture. J Clin Endocrinol Metab. 2014; 99:97–100.

6. Yoon HK, Park C, Jang S, et al. Incidence and mortality following hip fracture in Korea. J Korean Med Sci. 2011; 26:1087–1092.

7. Juby AG, De Geus-Wenceslau CM. Evaluation of osteoporosis treatment in seniors after hip fracture. Osteoporos Int. 2002; 13:205–210.

8. Kang BJ, Lee YK, Lee KW, et al. Mortality after hip fractures in nonagenarians. J Bone Metab. 2012; 19:83–86.

9. Lee SR, Ha YC, Kang H, et al. Morbidity and mortality in Jeju residents over 50-years of age with hip fracture with mean 6-year follow-up: a prospective cohort study. J Korean Med Sci. 2013; 28:1089–1094.

10. Tsuboi M, Hasegawa Y, Suzuki S, et al. Mortality and mobility after hip fracture in Japan: a ten-year follow-up. J Bone Joint Surg Br. 2007; 89:461–466.
11. Borgquist L, Ceder L, Thorngren KG. Function and social status 10 years after hip fracture. Prospective follow-up of 103 patients. Acta Orthop Scand. 1990; 61:404–410.

12. Black DM, Reid IR, Boonen S, et al. The effect of 3 versus 6 years of zoledronic acid treatment of osteoporosis: a randomized extension to the HORIZON-Pivotal Fracture Trial (PFT). J Bone Miner Res. 2012; 27:243–254.

14. Hochberg MC, Thompson DE, Black DM, et al. Effect of alendronate on the age-specific incidence of symptomatic osteoporotic fractures. J Bone Miner Res. 2005; 20:971–976.

15. Mithal A, Kaur P. Osteoporosis in Asia: a call to action. Curr Osteoporos Rep. 2012; 10:245–247.

16. Varthakavi PK, Joshi AS, Bhagwat NM, et al. Osteoporosis treatment in India: call for action. Indian J Endocrinol Metab. 2014; 18:441–442.

17. Lai MM, Ang WM, McGuiness M, et al. Undertreatment of osteoporosis in regional Western Australia. Australas J Ageing. 2012; 31:110–114.

18. Kim SR, Ha YC, Park YG, et al. Orthopedic surgeon's awareness can improve osteoporosis treatment following hip fracture: a prospective cohort study. J Korean Med Sci. 2011; 26:1501–1507.

19. Kim SR, Ha YC, Kim JR, et al. Incidence of hip fractures in Jeju Island, South Korea: a prospective study (2002-2006). Clin Orthop Surg. 2010; 2:64–68.

20. Johnell K, Fastbom J. Undertreatment of osteoporosis in the oldest old? A nationwide study of over 700,000 older people. Arch Osteoporos. 2009; 4:17–23.

21. Shibli-Rahhal A, Vaughan-Sarrazin MS, Richardson K, et al. Testing and treatment for osteoporosis following hip fracture in an integrated U.S. healthcare delivery system. Osteoporos Int. 2011; 22:2973–2980.

22. Curtis JR, McClure LA, Delzell E, et al. Population-based fracture risk assessment and osteoporosis treatment disparities by race and gender. J Gen Intern Med. 2009; 24:956–962.

23. Harrington JT, Broy SB, Derosa AM, et al. Hip fracture patients are not treated for osteoporosis: a call to action. Arthritis Rheum. 2002; 47:651–654.

24. Siris ES, Bilezikian JP, Rubin MR, et al. Pins and plaster aren't enough: a call for the evaluation and treatment of patients with osteoporotic fractures. J Clin Endocrinol Metab. 2003; 88:3482–3486.

25. Yi H, Ha YC, Lee YK, et al. National healthcare budget impact analysis of the treatment for osteoporosis and fractures in Korea. J Bone Metab. 2013; 20:17–23.

26. Goeree R, Blackhouse G, Adachi J. Cost-effectiveness of alternative treatments for women with osteoporosis in Canada. Curr Med Res Opin. 2006; 22:1425–1436.

27. Lee YK, Ha YC, Yoon BH, et al. Incidence of second hip fracture and compliant use of bisphosphonate. Osteoporos Int. 2013; 24:2099–2104.

28. Lee YK, Ha YC, Choi HJ, et al. Bisphosphonate use and subsequent hip fracture in South Korea. Osteoporos Int. 2013; 24:2887–2892.

29. Lyles KW, Colón-Emeric CS, Magaziner JS, et al. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med. 2007; 357:1799–1809.

30. Miki RA, Oetgen ME, Kirk J, et al. Orthopaedic management improves the rate of early osteoporosis treatment after hip fracture. A randomized clinical trial. J Bone Joint Surg Am. 2008; 90:2346–2353.

31. Cranney A, Lam M, Ruhland L, et al. A multifaceted intervention to improve treatment of osteoporosis in postmenopausal women with wrist fractures: a cluster randomized trial. Osteoporos Int. 2008; 19:1733–1740.

32. Majumdar SR, Beaupre LA, Harley CH, et al. Use of a case manager to improve osteoporosis treatment after hip fracture: results of a randomized controlled trial. Arch Intern Med. 2007; 167:2110–2115.

33. Rowe SM, Yoon TR, Ryang DH. An epidemiological study of hip fracture in Honam, Korea. Int Orthop. 1993; 17:139–143.

34. Mannius S, Mellström D, Odén A, et al. Incidence of hip fracture in western Sweden 1974-1982. Comparison of rural and urban populations. Acta Orthop Scand. 1987; 58:38–42.

35. Solbakken SM, Magnus JH, Meyer HE, et al. Impact of comorbidity, age, and gender on seasonal variation in hip fracture incidence. A NOREPOS study. Arch Osteoporos. 2014; 9:191.

36. Rális ZA. Epidemic of fractures during period of snow and ice. Br Med J (Clin Res Ed). 1981; 282:603–605.

37. Chiu KY, Ng TP, Chow SP. Seasonal variation of fractures of the hip in elderly persons. Injury. 1996; 27:333–336.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download