Abstract
Background
Subclinical thyroid dysfunction might influence a bone health. We evaluated whether subclinical hypothyroidism adversely affects bone health including bone mineral density (BMD), level of vitamin D, and bone turnover status in patients with hip fracture.
Methods
We evaluated 471 patients aged 50 years or older, who underwent hip fracture surgeries. BMD, level of vitamin D, bone turnover status, and one-year mortality were compared between subclinical hypothyroidism group and control group.
Results
BMD of femur and the level of 25-hydroxy-vitamin D (25-[OH]D) were similar in the two groups. There were no significant differences in bone turnover markers according to thyroid function. No significant differences were observed between the groups in utilization of intensive care unit (ICU), length of hospital stay, mobility, and one-year mortality.
Overt hypothyroidism reduces bone mineral density (BMD) and is well-known as one of secondary etiology for osteoporosis, which leads to increase risk of osteoporotic fracture such as hip fracture.[1,2,3] Subclinical hypothyroidism (SCH) is characterized by laboratory findings of an elevated serum thyroid stimulating hormone (TSH) level with a normal free thyroxine (T4) concentration.[4] And, it is a more common entity among the elderly population. Its prevalence ranged from 11 to 17% in community dwelling elderly population.[4,5,6,7,8,9]
Hip fracture is a representative of osteoporotic fracture, and is associated with a decreased mobility, diminished quality of life, and excess mortality.[10,11,12,13] There have not been reported the prevalence of SCH in the elderly Korean patients with hip fracture.
Although there were some reports that subclinical thyroid dysfunction might influence the prognosis of elderly patients after major surgery,[14] the clinical significance of SCH is controversial, especially in terms of bone health. Furthermore, there has been lack of studies about the effects of SCH on the bone health including BMD, vitamin D, and bone turnover marker in elderly patients with hip fracture.
The purposes of this study were (1) to evaluate the prevalence of SCH in a cohort of elderly individuals with hip fracture, (2) to determine whether SCH adversely affects bone health including BMD, level of vitamin D, and bone turnover status in patients with hip fracture, and (3) to compare the short-term clinical results between SCH group and control group.
We retrospectively reviewed medical records of 471 patients aged 50 years or older, who underwent hip fracture surgeries for femoral neck and intertrochanteric fracture from April 2010 and June 2012.
For thyroid function tests, serum TSH and free T4 concentrations were measured by immunoradiometry using commercial kits (TSH, CIS Biointernational, Gif-sur-Yvette, France; FT4, DiaSorin S.p.A, Saluggia, Italy). Euthyroidism was defined as a normal level of TSH (range, 0.3 to 4.0 mIU/L) and free T4 (range, 0.7 to 1.8 ng/dL) in the absence of thyroid medication. Individuals with TSH value below 0.3 mU/mL were considered to have hyperthyroidism and individuals with TSH value above 4.0 mU/mL were considered to have hypothyroidism. SCH was defined as a TSH concentration greater than 4.1 mIU/L and a free T4 concentration within the normal range. Subclinical hyperthyroidism was defined as a TSH level of less than 0.4 mIU/L with a T4 concentration within the normal range.
Of 358 patients with thyroid function tests, 285 had normal thyroid function, 48 had SCH, 8 had overt hypothyroidism, 12 had subclinical hyperthyroidism, and 5 had overt hyperthyroidism.
Among 333 patients with euthyroidism or SCH, 20 patients were excluded because of the history of administration of osteoporosis drug. Eleven patients were excluded because of thyroid medication. Thus, 261 patients in euthyroidism group and 41 patients in SCH group were finally analyzed in this study.
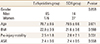
In euthyroidism group, there were 85 men and 176 women with a mean age of 78.7 years (range, 59 to 93 years) at the time of operation. Their mean body mass index (BMI) was 22.0 kg/m2 (range, 14.8 to 33.0 kg/m2). In SCH group, there were 14 men and 27 women with a mean age of 78.5 years (range, 58 to 86 years) at the time of operation. Their mean BMI was 21.6 kg/m2 (range, 19.2 to 28.7 kg/m2) (Table 1).
Cannulated screws (6.5 mm diameter), sliding hip screws, and intramedullary nails were used for internal fixation. Bipolar hemiarthroplasty and total hip arthroplasty were used for hip arthroplasty.
We compared the BMD, the level of 25-hydroxy-vitamin D (25-[OH]D), serum C-terminal telopeptides of type I collagen (CTX), and serum osteocalcin (OCN) in both groups. BMD was measured by DXA (Lunar Prodigy Advance, GE Lunar, Medison, WI, USA). The 25-(OH)D were measured by using Diels-Alder derivatization followed by ultrahigh-performance liquid chromatography-tandem mass spectrometry (Waters, Milford, MA, USA). Bone turnover markers, including CTX (Roche Diagnostics, Indianapolis, IN, USA) and OCN (Roche Diagnostics, Indianapolis, IN, USA), were measured.
We also compared clinical results including ambulatory ability according to Koval's categories,[15] the necessity of intensive care (the utilization of intensive care unit [ICU]), the length of hospital stay and one year mortality in both groups.
Statistical significance of the differences between the 2 groups was determined by Chi-square test for categorical variables and Student's t-test for continuous variables. Statistical analyses were conducted with the SPSS for Windows statistical package (version 12.0; SPSS Inc., Chicago, IL, USA), and P-value less than 0.05 was considered as significant.
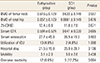
The prevalence of SCH in this study was 13.1% (41/312). BMD of femur and the level of 25-(OH)D were similar in the two groups. There were no significant differences in bone turnover markers according to thyroid function. No significant differences were observed between the groups in utilization of ICU, length of hospital stay, mobility, and one-year mortality (Table 2).
In this study, the overall prevalence of SCH was 13.1%, and SCH was not associated with reduced bone health, including BMD, the level of 25-(OH)D, and bone turnover marker. In addition, SCH did not affected to the short-term results after hip fracture surgery, in terms of utilization of ICU, hospital stay, mobility and one-year mortality after hip fracture surgery.
Prevalence of SCH ranged from 11 to 17% in general elderly population.[5,6,7,8,9] Our finding of 13.1% was comparable with these previous reports.
Factors associated with a decreased BMD include older age, female gender, diabetes, use of corticosteroid, and rheumatoid arthritis.[16,17]
Although musculoskeletal system is one of the target organs of thyroid hormone,[1,2,3] there has been a debate that hypothyroidism might affect a BMD.[4,18,19,20,21,22,23] Our finding did not support that SCH might reduce a BMD. And, bone health including vitamin D and bone turnover marker in patients with SCH were similar to those of patients without SCH.
The relationship between SCH and decreased morbidity after hip fracture surgery has not been evaluated. We could not find a significant difference in mobility between SCH group and control group in this study.
It was controversial whether SCH is associated with early mortality after major surgery.[24,25] Mortality after hip fractures in the elderly is a key outcome of treatment. Various factors affecting mortality after hip fractures have been investigated. These include delayed surgical intervention,[26,27] advanced age, the American Society of Anesthesiologists (ASA) grade, cognitive function, function or mobility before hip fracture, and number of pre-existing medical conditions.[11,13,28] Although we could not find a statistical significance between two groups, there was a marginal significance in one-year mortality between SCH group and control group in this study (P=0.064).
There were some limitations in this study. This study was retrospective, and we included small number of SCH.
In summary, the bone health of SCH patients was not different with that of control group, and there was no significant difference in morbidity and mortality after hip fracture surgery between two groups. Although some studies recommended thyroid hormone replacement to avoid early complication after major surgery such as cardiac surgery or gastrectomy,[14,29] we suggest that the well-designed larger study is necessary prior to consider thyroid hormone replacement or administration of T3.
Figures and Tables
References
2. Vestergaard P, Weeke J, Hoeck HC, et al. Fractures in patients with primary idiopathic hypothyroidism. Thyroid. 2000; 10:335–340.

3. Coindre JM, David JP, Rivière L, et al. Bone loss in hypothyroidism with hormone replacement. A histomorphometric study. Arch Intern Med. 1986; 146:48–53.

4. Jayme JJ, Ladenson PW. Subclinical thyroid dysfunction in the elderly. Trends Endocrinol Metab. 1994; 5:79–86.

5. Canaris GJ, Manowitz NR, Mayor G, et al. The Colorado thyroid disease prevalence study. Arch Intern Med. 2000; 160:526–534.

6. Hollowell JG, Staehling NW, Flanders WD, et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab. 2002; 87:489–499.

7. Kim YA, Park YJ. Prevalence and risk factors of subclinical thyroid disease. Endocrinol Metab. 2014; 29:20–29.

8. Sawin CT, Castelli WP, Hershman JM, et al. The aging thyroid. Thyroid deficiency in the Framingham Study. Arch Intern Med. 1985; 145:1386–1388.

9. Tunbridge WM, Evered DC, Hall R, et al. The spectrum of thyroid disease in a community: the Whickham survey. Clin Endocrinol (Oxf). 1977; 7:481–493.

10. Lee YK, Lee YJ, Ha YC, et al. Five-year relative survival of patients with osteoporotic hip fracture. J Clin Endocrinol Metab. 2014; 99:97–100.

11. Yoon HK, Park C, Jang S, et al. Incidence and mortality following hip fracture in Korea. J Korean Med Sci. 2011; 26:1087–1092.

12. Park C, Ha YC, Jang S, et al. The incidence and residual lifetime risk of osteoporosis-related fractures in Korea. J Bone Miner Metab. 2011; 29:744–751.

13. Kang BJ, Lee YK, Lee KW, et al. Mortality after hip fractures in nonagenarians. J Bone Metab. 2012; 19:83–86.

14. Park YJ, Yoon JW, Kim KI, et al. Subclinical hypothyroidism might increase the risk of transient atrial fibrillation after coronary artery bypass grafting. Ann Thorac Surg. 2009; 87:1846–1852.

15. Koval KJ, Aharonoff GB, Rosenberg AD, et al. Functional outcome after hip fracture. Effect of general versus regional anesthesia. Clin Orthop Relat Res. 1998; 37–41.
16. Shin CS, Choi HJ, Kim MJ, et al. Prevalence and risk factors of osteoporosis in Korea: a community-based cohort study with lumbar spine and hip bone mineral density. Bone. 2010; 47:378–387.

17. Rozental TD, Shah J, Chacko AT, et al. Prevalence and predictors of osteoporosis risk in orthopaedic patients. Clin Orthop Relat Res. 2010; 468:1765–1772.

18. Marwaha RK, Garg MK, Tandon N, et al. Thyroid function and bone mineral density among Indian subjects. Indian J Endocrinol Metab. 2012; 16:575–579.

19. Bertoli A, Fusco A, Andreoli A, et al. Effect of subclinical hypothyroidism and obesity on whole-body and regional bone mineral content. Horm Res. 2002; 57:79–84.

20. Meier C, Beat M, Guglielmetti M, et al. Restoration of euthyroidism accelerates bone turnover in patients with subclinical hypothyroidism: a randomized controlled trial. Osteoporos Int. 2004; 15:209–216.

22. Pines A, Dotan I, Tabori U, et al. L-thyroxine prevents the bone-conserving effect of HRT in postmenopausal women with subclinical hypothyroidism. Gynecol Endocrinol. 1999; 13:196–201.

23. Lakatos P. Thyroid hormones: beneficial or deleterious for bone? Calcif Tissue Int. 2003; 73:205–209.

24. Haentjens P, Van Meerhaeghe A, Poppe K, et al. Subclinical thyroid dysfunction and mortality: an estimate of relative and absolute excess all-cause mortality based on time-to-event data from cohort studies. Eur J Endocrinol. 2008; 159:329–341.

25. Kalra S, Williams A, Whitaker R, et al. Subclinical thyroid dysfunction does not affect one-year mortality in elderly patients after hip fracture: a prospective longitudinal study. Injury. 2010; 41:385–387.

26. Weller I, Wai EK, Jaglal S, et al. The effect of hospital type and surgical delay on mortality after surgery for hip fracture. J Bone Joint Surg Br. 2005; 87:361–366.

27. Kenzora JE, McCarthy RE, Lowell JD, et al. Hip fracture mortality. Relation to age, treatment, preoperative illness, time of surgery, and complications. Clin Orthop Relat Res. 1984; 45–56.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download