Abstract
Background
Malnutrition among inflammatory bowel disease (IBD) may arise from factors including inadequate dietary intake, malabsorption, and progression of disease. IBD has been reported an increased prevalence of low bone mass. The aims of the present study were to evaluate the nutritional status and to investigate the correlation between bone mineral density (BMD) and nutrient factors in patients with IBD.
Methods
A total of 41 subjects were classified into normal group (n=21) and malnourished group (n=20) by the subjective global assessment result. We surveyed the dietary habit, nutrient intake, and BMD.
Results
Subjects' average age was 36.7 years old, and included 26 ulcerative colitis and 15 Crohn's disease. The serum C-reactive protein (CRP) was significantly higher and serum calcium was significantly lower in the malnourished group. Lower bone density subjects were more in the malnourished group but no significant difference. Intake of energy, protein, carbohydrate, fiber, iron, sodium, potassium, zinc, vitamin B6, vitamin C and folate were significantly lower in the malnourished group. The BMD of malnourished group showed correlation with triceps skin fold thickness (TSF), CRP, dietary calcium, phosphorous, iron, animal iron, zinc and vitamin.
Inflammatory bowel disease (IBD) is a chronic condition that includes Crohn's disease and ulcerative colitis. The incidence of both intestinal disorders has recently increasing, and there are several problems associated with symptoms and side effects that follow a course of relapse and treatment.[1] Decrease in bone density is a relatively common complication of IBD, occurring in about 20-50% patients. Poor bone density may be caused by malabsorption of calcium and vitamin D, with steroid, malnutrition, and an unbalanced diet.[2] Another study reported that inflammatory mediators such as tumor necrosis factor, interleukin (IL)-1β, and IL-6 cause abnormalities in the bone regenerating rate, which eventually lead to a decrease in bone density.[3]
Bone density generally varies according to genetics or ethnicity. The effective way to prevent osteoporosis is to increase bone density when an individual is young, as the bone becomes dense during the growth period. Since various nutrients have already been proven to improve bone density, a long-term diet with good nutrients is important.[4] IBD can occur at a relatively young age and persist a lifetime. A previous study therefore suggested lifestyle changes to prevent bone loss and strategies to screen and treat high-risk patients.[1]
Individuals with IBD must limit their food intake due to the disease itself or other complications, which eventually leads to malnutrition. Weight loss, hypoalbuminemia, and anemia are the most frequent manifestations of malnutrition. Approximately 23% of outpatients and 85% of inpatients with IBD were reported to have malnutrition associated with the disease. Further, this prolonged malnutrition in turn decreases bone density.[5] Complete prohibition of certain foods or inappropriate food limits due to lack of adequate information also cause these problems. For effective treatment, the patient must be well nourished and be provided nutritional support when oral intake is not possible. Healthcare providers recommend that more attention be paid to the relationship between IBD, and poor nutrition.[6] However, only few studies have examined the nutritional needs of patients with IBD in Korea, although studies by decreased bone density caused by poor nutrition are currently underway.
The aim of the present study was to investigate the relationship between bone density and IBD in order to ensure that patients receive the proper nutrition needed to manage and prevent osteoporosis. Hence, we surveyed the dietary habit, nutrient intake, and bone density of patients with Crohn'sdisease and ulcerative colitis. The relationship of bone mineral density (BMD) and nutrient intake based on nutritional status were also investigated.
This study was conducted on patients with IBD who were treated at the Department of Internal Medicine, Soonchunhyang University Bucheon Hospital, between September 2010 and September 2011. A doctor evaluated compliance of patients for study when the patient visited for check ups, and they explained the purpose and procedures of the study. Patients who agreed to sign the experimental agreement were included in this study. Patients for whom the cause of poor bone density could have been completely unrelated to IBD were excluded. Other exclusion criteria included a history of colectomy, diabetes, thyroid disease, liver disease, kidney disease, sexual malfunction, fractures, and metabolic bone disease; menopause; medications such as vitamin D supplement, sex hormones, and phosphate binder; and a controlled diet that increases bone density. Although 70 patients were enrolled, data were collected only from 41 subjects who completed the study except for refused investigation, did not undergo a bone-related test, or had missing information. The 41 subjects were classified into two groups based on nutrition status: the normal group (n=21) and the malnourished group (n=20).
The subjects' age and gender were obtained. The weight and height were also measured and the body mass index (BMI) was calculated. The triceps skin fold thickness (TSF) and waist circumference were measured and weight loss rate within the past 6 months were surveyed. The clinical information on the diagnosis and diagnostic period were derived from the medical records. Disease activity and cumulative steroid dose were assessed by a doctor. Disease activity of ulcerative colitis was classified by the Truelove and Witts severity index[7] and disease activity of Crohn's disease was assessed by a Crohn's disease activity index (CDAI).[8] The nutritional status was evaluated using subjective global assessment (SGA)[9] by the clinical dietitian and the subjects were classified into normal group or malnourished group.
The blood sample was collected from the subjects after 10-12 hours fast. The test items included hemoglobin, hematocrit, C-reactive protein (CRP), serum albumin, calcium and phosphorous (Technicon AutoAnalyzer methods). Serum intact parathyroid hormone (iPTH) was measured by an electrochemiluminescent immunoassay and serum 25-hydroxy-vitamin D3 (25-[OH]D3) was measured using a chemiluminescent immunoassay. The BMD was measured using the dual energy X-ray absorptiometry (DXA) equipment (Lunar Prodigy; GE Lunar Corp., Madison, WI, USA) on the subject's lumber spine and femoral neck. Bone density was expressed as BMD, Z-score and T-score. The bone density was evaluated using a T-score -1.0 or over was normal; -2.5 ~ -1.0 was osteopenia; and -2.5 or less was osteoporosis. Dichotomizing the Z-score, a cutoff value of ≤ -1 standard deviation (SD) was defined as reduced bone mass.[10]
The questions on the regularity of usual meals, skipped meals, meal time and amount of meals, drinking, smoking and exercise habits were surveyed per individual. Skilled clinical dietitian interviewed subjects using photographs of food items and a booklet containing eye measurement data as aids for the nutrient intake survey. Data on dietary intake amount were collected using the 24-hr recall method for three days and intakes of nutritents were analyzed with the CAN-Pro 3.0 (Korean Nutrition Society, Seoul, Korea). In addition, to evaluate the intake excess or deficiency by nutrient, the intake was compared with the recommended nutritional intake for Koreans.[11]
The mean and standard deviation were calculated using SPSS statistical software ver. 18.0 (SPSS Inc., Chicago, IL, USA). The difference on the frequency of food intake between the two groups was tested chi-square test while the mean was compared using t-test. The correlation between bone density and its related variables was analyzed using Pearson's correlation coefficient. All results were considered statistically significant when P<0.05.
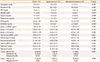
There were 25 male and 16 female subjects (total 41 subjects) and their mean age was 36.7 years old. Although more male subjects in the malnourished group, there was no significant difference. The average BMI was 22 kg/m2 and 1.9% of subject showed weight loss within the recently 6 months. The weight loss rate was 0.4% in normal group and 3.4% in malnourished group which was significantly different (P<0.001). The average waist circumference was 81.1 mm and average TSF was 12.2 mm. Twenty-six subjects (63.4%) had ulcerative colitis and 15 subjects (36.6%) had Cronhn's disease. There were more ulcerative colitis patients in general but the ratio between ulcerative colitis and Cronhn's disease was the same in the malnourished group. The average disease period was 44.2 months (approximately 3.7 years) which showed 32 subjects (78%) had the disease for more than one year while only 9 subjects (22%) had it for less than a year. In comparison of disease activity, most of ulcerative colitis was remission and mild status. Disease activity of Cronhn's disease also assessed remission status. A dose of steroids were more in the malnourished group, there was no significant difference (Table 1).
The blood test showed that the average hemoglobin was 12.6 g/dL, below the normal range (13-17 g/dL). The malnourished group showed a lower range than that of the normal group but the difference was not that significant. The result showed the serum albumin, calcium and phosphorous levels were within normal range but the average CRP was at 0.8 mg/dL slightly higher than the normal range (0-0.5 mg/dL). The result of CRP was significantly higher in the malnourished group than that of the normal group (P<0.05). The serum calcium and 25-(OH)D3 level were also significantly lower in the malnourished group (P<0.05). The bone density test showed that T-score of lumbar spine and femoral neck were lower in the malnourished group than those of the normal group but the difference was not significant. Fifteen subjects (36.6%) were classified into osteopenia based on their T-score while 2 subjects (4.9%) have osteoporosis. There were more subjects in the malnourished group who had a lower bone density compared with the normal group but the difference was not significant (Table 2).
The comparison of eating behaviors and their life habit is presented in Table 3. For the regularity of meals, 20 subjects (48.8%) answered 'regular' while 21 subjects (51.2%) answered 'irregular,' which meant more than half of the subjects were having irregular meals. The skipping of meals rate showed that breakfast accounted for the highest percentage with 13 (76.5%) out of the 17 subjects (41.5%) who answered 'I skip meals'. For the duration of meals, 20 subjects (48.8%) answered '10-20 minutes' while 15 subjects (36.6%) answered 'less than 10 minutes'. For the subjective assessment on the food intake 15 subjects (36.6%) answered 'I eat a lot'; 16 subjects (39%), 'I eat appropriate amount'; and 10 subjects (24.4%) 'I eat small amount'. 34 subjects (82.9%) answered they do not smoke while 28 subjects (68.3%) answered they do not exercise. There was no significant differences in smoking and drinking but the malnourished group had a lower exercise rate and a higher smoking and drinking alcohol rate. Generally, item on the diet or life habit not showed significant differences between the groups (Table 3).
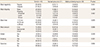
The average energy intake was 1,753.7 kcal; 1,906 kcal in the normal group and 1,527.9 kcal in the malnourished group. The energy intake was significantly lower in the malnourished group (P<0.05). Intake of protein (P<0.05), carbohydrate (P<0.05), fiber (P<0.05), iron (P<0.05), sodium (P<0.05), potassium (P<0.05), zinc (P<0.01), vitamin B6 (P<0.05), vitamin C (P<0.05), and folate (P<0.01) were significantly lower in the malnourished group. The intakes of fiber, calcium, vitamin B2, vitamin C and folate were lower than the recommended nutritional intakes for Koreans in the normal group. The intakes of fiber, calcium, zinc, vitamin B1, vitamin B2, niacin, vitamin C and folate were lower than the recommended nutritional intakes for Koreans in the malnourished group (Table 4).
The correlation with as T-score of lumbar spine and all related variables by nutritional status were analyzed and only significant results were presented in Table 5. The BMD of malnourished group showed correlation with TSF (P<0.01), CRP (P<0.05), calcium (P<0.01), phosphorous (P<0.05), iron (P<0.05), animal iron (P<0.05), zinc (P<0.05) and vitamin B1 (P<0.05) in their diet while the normal group showed correlation with TSF (P<0.05), phosphorous (P<0.05) and iron (P<0.05) in their diet (Table 5).
Over the last few decades, the incidence of IBD has increased in Asian countries.[12] The present study investigated the correlation of bone density and the rate of malnutrition with the nutrient intake of patients with IBD. A nutritional approach to determining the treatment plan for IBD is considered very important. Therefore, it is first necessary to determine the nutritional status of patients in order to provide diet intervention or nutritional support.[13] Of the subjects in this study, 48.8% were malnourished and weight loss since the 6 months in the malnourished group was significantly higher compared to normal group. More patients with Crohn's disease were malnourished than those with ulcerative colitis, but the difference was not significant. This result is related to that of another study which reported Crohn's disease affects small bowels and causes more severe malnutrition.[14] Most blood test results were within the normal range in our patients; however, although the hemoglobin level was below normal (13-17 g/dL) overall, it was substantially lower in the malnourished group. In an acute response test, CRP levels were significantly higher in the malnourished group. In a previous study, anemia, a generally observed symptom of nutritional deficiency, was found in 16% outpatient subjects and 68% inpatient subjects.[15] Another study reported that anemia needs to be treated before other symptoms as it can decrease the performance of routine activities and lower quality of life.[16] The results of the present study did not show any significant difference in anemia between the two groups with different nutritional status, although the hemoglobin level was low in the malnourished group. In general, more proactive management is required to maintain the hemoglobin level in the normal range.
Many epidemiologic studies have reported decreased bone density in IBD, and this association was considered closely related to vitamin D deficiency, systemic inflammation, or use of oral steroids.[17,18] The risk of fractures increases with disease activity. Despite this, most patients do not receive bone-protective treatment. A previous study recommended effective screening and treatment for high-risk patients in order to prevent IBD.[19] Bone density results showed that the average bone density was -0.60±1.32 g/cm2 for the lumbar spine and -0.40±1.45 g/cm2 for the femoral neck. In the present study, the decrease in bone density was greater in the malnourished group than in the normal group as determined by the World Health Organization osteoporosis criteria, but the difference was not significant. Further, the decrease in bone density of 41.5% reported in the Korean IBD patients in our study was lower than the 63.3% cited by Park et al.[20] It was difficult to accurately compare between our study and the study by Park et al.[20] because of the different set of subjects and disease period. Nonetheless, both studies showed that bone density testing and active management from the early stages of diagnosis are necessary to prevent long-term complications of IBD.
As part of their usual dietary habit, about half the subjects in our study had irregular meals and skipped breakfast, but the difference between groups was not significant. The malnourished group also had a higher proportion of patients with drinking and smoking habits and a lower proportion of patients who exercised. Smoking affects the incidence and activity of IBD. Compared to non-smokers, smokers require a higher dose of steroids and immunosuppressive agents for Crohn's disease treatment since smoking actually accelerates disease progression.[21,22] Thus, from the treatment viewpoint, drinking and smoking should be strictly prohibited. Most IBD patients show nutrient deficiency, the malnourished group in our study as well showed lower intake of nutrients, especially energy, protein, carbohydrates, fiber, iron, sodium, potassium, zinc, vitamin B6, vitamin C, and folate. The intake of calcium, zinc, vitamin B2, vitamin C, and folate was lower than the recommended amount for Koreans.[11] However, the average intake of energy, calcium, iron, and vitamin A intake was higher in this study than in a previous study by Kang[23] Considering the malabsorption in patients with IBD,[24,25,26] selection of the right food, well-balanced nutrient intake, and use of supplements depending on an individual's nutrient intake are essential. In the statistical analysis performed in the present study to confirm the factors correlated with bone density, the results showed that inclusion of phosphorus and iron in the diet was correlated with the bone density in the normal group. On the other hand, nutrients such as calcium, phosphorous, iron, animal iron, zinc, and vitamin B1 showed a correlation with the bone density in the malnourished group.
Despite the evidence, the importance of nutritional factors as a cause of decreased bone density in IBD varies among studies.[20,27,28] However, more recommendations indicate that daily management is required to ensure adequate levels of calcium and vitamin D in the diet and to improve malnutrition to prevent osteoporosis.[1,29] Because of the limited number of subjects, this study was not able to represent all IBDs. Nonetheless, our results were useful in confirming the role of malnutrition, nutrient intake, and bone density in patients with chronic IBD. Our study also showed that patients with inflammatory bowel rarely receive treatment to improve bone density. Malnutrition among these patients was high, and about 40% had decreased bone density and unbalanced nutrient intake.
On the basis of our findings, we recommend that malnutrition be considered during the early stage of disease diagnosis and a nutrition intervention be conducted to ensure better treatment efficacy, improve quality of life, and prevent any complications related to IBD. Additionally, proper education about nutrition is required to prevent poor bone density, and multidisciplinary studies on this matter are required in the future.
Figures and Tables
Table 1
Comparison of clinical characteristics and anthropometric data according to nutritional status

References
1. Ali T, Lam D, Bronze MS, et al. Osteoporosis in inflammatory bowel disease. Am J Med. 2009; 122:599–604.

2. Cosnes J, Gower-Rousseau C, Seksik P, et al. Epidemiology and natural history of inflammatory bowel diseases. Gastroenterology. 2011; 140:1785–1794.

3. Ghishan FK, Kiela PR. Advances in the understanding of mineral and bone metabolism in inflammatory bowel diseases. Am J Physiol Gastrointest Liver Physiol. 2011; 300:G191–G201.

4. Song YJ, Paik HY, Yu CH. Factors affecting bone mineral density by dietary pattern group for some Korean college women. Korean J Nutr. 2006; 39:460–466.
5. Lee KM. Nutrition in inflammatory bowel disease. Korean J Gastroenterol. 2008; 52:1–8.
6. Prince A, Whelan K, Moosa A, et al. Nutritional problems in inflammatory bowel disease: the patient perspective. J Crohns Colitis. 2011; 5:443–450.

7. D'Haens G, Sandborn WJ, Feagan BG, et al. A review of activity indices and efficacy end points for clinical trials of medical therapy in adults with ulcerative colitis. Gastroenterology. 2007; 132:763–786.
8. Stange EF, Travis SP, Vermeire S, et al. European evidence based consensus on the diagnosis and management of Crohn's disease: definitions and diagnosis. Gut. 2006; 55:Suppl 1. i1–i15.

9. Detsky AS, McLaughlin JR, Baker JP, et al. What is subjective global assessment of nutritional status? JPEN J Parenter Enteral Nutr. 1987; 11:8–13.

10. Kanis JA, Melton LJ 3rd, Christiansen C, et al. The diagnosis of osteoporosis. J Bone Miner Res. 1994; 9:1137–1141.

11. The Korean Nutrition Society. Dietary reference intakes for Koreans: first revision 2010. Seoul: The Korean Nutrition Society, Ministry of Health & Welfare, Ministry of Food and Drug Safety;2010.
12. Prideaux L, Kamm MA, De Cruz PP, et al. Inflammatory bowel disease in Asia: a systematic review. J Gastroenterol Hepatol. 2012; 27:1266–1280.

13. Massironi S, Rossi RE, Cavalcoli FA, et al. Nutritional deficiencies in inflammatory bowel disease: therapeutic approaches. Clin Nutr. 2013; 32:904–910.

14. Carter MJ, Lobo AJ, Travis SP. Guidelines for the management of inflammatory bowel disease in adults. Gut. 2004; 53:Suppl 5. V1–V16.

15. Gomollon F, Gisbert JP. Anemia and inflammatory bowel diseases. World J Gastroenterol. 2009; 15:4659–4665.

16. Gasche C, Lomer MC, Cavill I, et al. Iron, anaemia, and inflammatory bowel diseases. Gut. 2004; 53:1190–1197.

17. Bernstein CN, Seeger LL, Sayre JW, et al. Decreased bone density in inflammatory bowel disease is related to corticosteroid use and not disease diagnosis. J Bone Miner Res. 1995; 10:250–256.

18. Jahnsen J, Falch JA, Aadland E, et al. Bone mineral density is reduced in patients with Crohn's disease but not in patients with ulcerative colitis: a population based study. Gut. 1997; 40:313–319.

19. American Gastroenterological Association. American Gastroenterological Association medical position statement: guidelines on osteoporosis in gastrointestinal diseases. Gastroenterology. 2003; 124:791–794.
20. Park JJ, Jung SA, Noh YW, et al. Analysis of risk factors for low bone mineral density in patients with inflammatory bowel disease. Korean J Gastroenterol. 2010; 55:237–244.

21. Cosnes J. Smoking, physical activity, nutrition and lifestyle: environmental factors and their impact on IBD. Dig Dis. 2010; 28:411–417.

22. Russel MG, Volovics A, Schoon EJ, et al. European Collaborative IBD Study Group. Inflammatory bowel disease: is there any relation between smoking status and disease presentation? Inflamm Bowel Dis. 1998; 4:182–186.

23. Kang EH. Nutritional state of the patients with Crohn's disease in Korea [master's thesis]. Seoul: Ewha Womans University;2002.
24. Vagianos K, Bector S, McConnell J, et al. Nutrition assessment of patients with inflammatory bowel disease. JPEN J Parenter Enteral Nutr. 2007; 31:311–319.

25. Tighe MP, Cummings JR, Afzal NA. Nutrition and inflammatory bowel disease: primary or adjuvant therapy. Curr Opin Clin Nutr Metab Care. 2011; 14:491–496.
26. Hartman C, Eliakim R, Shamir R. Nutritional status and nutritional therapy in inflammatory bowel diseases. World J Gastroenterol. 2009; 15:2570–2578.

27. Silvennoinen JA, Karttunen TJ, Niemelä SE, et al. A controlled study of bone mineral density in patients with inflammatory bowel disease. Gut. 1995; 37:71–76.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download